Published online Apr 28, 2007. doi: 10.3748/wjg.v13.i16.2388
Revised: January 15, 2006
Accepted: January 31, 2007
Published online: April 28, 2007
Large type 1 cysts are prone to perforation. Furthermore, insufficient drainage with subsequent abscess is a frequent problem of large cysts. We report here a case of a 19-year old man who was admitted to the hospital with pain in the right upper quadrant and epigastric region. An asymmetrical right upper quadrant enlargement was detected on physical examination. Ultrasonography and computerized tomography revealed a type 1 giant hydatid cyst in the right hepatic lobe, measuring 16 cm in diameter. During operation, partial cystectomy and drainage were done. The large dead space was obliterated by the ‘sandwich’ method. Omentum and gelatin sponges were used to fill the cavity. The postoperative period was uneventful and the patient was discharged on the 5th postoperative day.
- Citation: Ezer A, Nursal TZ, Noyan T, Moray G. Giant hepatic hydatid cyst: A case report. World J Gastroenterol 2007; 13(16): 2388-2389
- URL: https://www.wjgnet.com/1007-9327/full/v13/i16/2388.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i16.2388
Of all cysts in the liver, 50%-70% are caused by Echinococcus granulosus. Most of these cysts are unique and settle in the right lobe of the liver. Hydatid cysts may be asymptomatic, or may cause abdominal pain, jaundice, or a visible abdominal mass[1].
Patients affected by liver hydatid cysts from Echinococcus granulosus are generally asymptomatic for a long time. They usually seek medical care when their cysts have reached a large size, and a large amount of liver parenchyma has already been destroyed[2]. Because there is no reliable pharmaceutical intervention, the recommended and most effective treatment of hepatic hydatid cysts is surgery, the primary goal of which is to resect the cysts without spilling its contents[3]. Although percutaneous treatment is a first-line treatment for typeIand II liver hydatid diseases, surgery is advocated for unusual typeIand II cases. Large typeIcysts are prone to perforation. Furthermore, insufficient drainage with subsequent abscess is a frequent problem of large cysts.
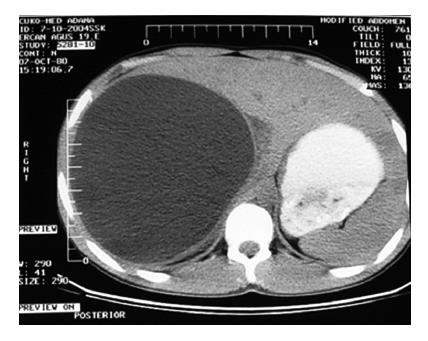
A 19-year-old man was admitted to our hospital with pain in the right upper quadrant and epigastric region beginning 1 mo earlier. Abdominal examination revealed remarkable epigastric tenderness and an asymmetric right upper quadrant enlargement. Results of laboratory tests were normal except for an elevated alkaline phosphatase level (111 IU/L; normal 40-100 IU/L). Ultrasonography and computerized tomography (CT) scans of the abdomen revealed a typeIgiant hydatid cyst in the right hepatic lobe, measuring 16 cm in diameter (Figure 1). During operation, the incision and operative field were carefully isolated with abdominal packs soaked in 200 g/L saline. The hydatid cyst was aspirated through its most prominent part using a blunt spinal needle. The cavity was filled with 20% saline for 10 min, aspirated again, and then opened through a vertical 10 cm incision. The contents in the cyst were evacuated, and inspection of the cavity revealed biliary communication that was sutured primarily. The large dead space was eliminated using the “sandwich” method. The cavity was eliminated manually by compressing the surrounding healthy parenchyma from left to right toward the cavity’s midline. While compression was maintained, the cyst’s edges were sutured together using generous mattress sutures passing through the fibrous capsule’s cranial, anterior, and ventral aspects. Because the omentum was not sufficient to completely fill the cavity, some dead spaces in the liver were filled with gelatin sponge and omentum. A prophylactic large-caliber passive tube drain was placed in contact with the inferior liver surface. The abdominal wall was closed in layers.
During the postoperative period, 100 cc of serous fluid was measured from the abdominal drain. The drain was withdrawn on the second postoperative day. The postoperative period was uneventful, and the patient was discharged on the fifth postoperative day. Control abdominal CT was performed 3 mo after operation, revealing a small residual cavity (Figure 2).
A variety of techniques have been recommended to manage the residual cavity after cystectomy. Alternatives include hepatic resection, pericystectomy, partial cystectomy combined with omentoplasty, suture obliteration (capitonnage), introflexion, cystojejunostomy, marsupialization, external drainage, and primary closure after installation of saline solution[4]. The strong possibility of a residual cavity after percutaneous treatment limits the use of this form of therapy for large cysts. Therefore, the sandwich technique was used for this patient. Losanoff and coworkers[5] safely used this technique (which preserves the liver parenchyma) in 8 patients to close giant cyst cavities between 1993 and 2000. In this study, there were no reports of sepsis, postoperative bile leak, or other complications. Dead spaces were filled with pedicled omentum. If omentum is not available, gelatin sponges may be used prior to suture[5]. We advocate this technique for giant hydatid cysts irrespective of the type.
S- Editor Wang J L- Editor Wang XL E- Editor Ma WH
| 1. | Yalin R, Aktan AO, Yeğen C, Döşlüoğlu HH. Significance of intracystic pressure in abdominal hydatid disease. Br J Surg. 1992;79:1182-1183. |
| 2. | Sayek I, Tirnaksiz MB, Dogan R. Cystic hydatid disease: current trends in diagnosis and management. Surg Today. 2004;34:987-996. |
| 3. | Hofstetter C, Segovia E, Vara-Thorbeck R. Treatment of uncomplicated hydatid cyst of the liver by closed marsupialization and fibrin glue obliteration. World J Surg. 2004;28:173-178. |