Published online Apr 21, 2007. doi: 10.3748/wjg.v13.i15.2179
Revised: February 3, 2007
Accepted: February 14, 2007
Published online: April 21, 2007
AIM: To introduce a new method: small endoscopic sphincterotomy (ES) combined with endoscopic papillary large balloon dilation (SES + EPLBD) to treat patients with large biliary stones.
METHODS: Retrieval of large biliary stones was performed in 88 patients. Mean stone size was 14 ± 3 mm and mean number of stones was 2.5 ± 3.5. Firstly, ES with a small incision was performed. Next, endoscopic papillary dilation was performed with a large balloon to slowly match the size of the bile duct. Stones were then retrieved from the biliary duct with a balloon and a basket.
RESULTS: Stone retrieval was successful in all cases except one cystic duct stone case without the need to crush large stones. Mean procedure time was 30 ± 5 min. Dilating the papillary orifice with a large balloon made it possible to remove large stones smoothly without crushing them. After dilation with the large balloon, there were some instances of oozing, but no perforations. One instance of post-procedural pancreatitis (1%) occurred.
CONCLUSION: SES + EPLBD was effective for the retrieval of large biliary stones without the use of mechanical lithotripsy.
- Citation: Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol 2007; 13(15): 2179-2182
- URL: https://www.wjgnet.com/1007-9327/full/v13/i15/2179.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i15.2179
Endoscopic sphincterotomy (ES), first described in 1974, has gained wide acceptance in the treatment of common bile duct stones[1]. Complications in ES include hemorrhage, pancreatitis, cholangitis, and perforation of the duodenal wall[2]. Concerns still exist about the size and number of stones in ES. It is especially difficult to remove large and multiple stones. Endoscopic papillary dilation combined with small endoscopic sphincterotomy addresses these concerns and is indeed necessary for complete clearance of the bile duct. Simultaneous and gradual large dilation of the sphincter of Oddi and a small ES facilitate proper extraction of larges sizes and/or multiple bile duct stones without complications. Eighty-eight cases of extraction of large and/or multiple common bile duct (CBD) stones were performed. The results of this combined method of stone extraction showed advantages over the use of ES or EPD alone with regards to complications and procedure time.
Between May 2003 and April 2006, small ES combined with endoscopic papillary large balloon dilation (SES + EPLBD) was carried out in patients with large and multiple CBD stones. Eighty-eight consecutive patients who had CBD stones over 12 mm in diameter were selected for this treatment. The stone size (over 12 mm in diameter) and number (1-25) were determined by endoscopic retrograde cholangiopancreatography (ERCP). ERCP was performed by one experienced endoscopist and the diagnosis was confirmed in each instance. The median age of patients was 74 ± 17 year, with a range of 42 to 98 year (41 women and 47 men). Forty-six patients had both gallbladder and CBD stones and 33 patients had undergone cholecystectomy prior to this treatment. Coagulation indices in all but 2 patients were normal. Stone size 14.0 ± 3.4 mm; Number of stones 2.5 ± 3.5; Number of patients with gallbladder 55; Number of patients with gallbladder stones 46; Patients with cholangitis 22. Informed consent of the hospital was obtained from each patient who underwent the clinical treatment in accordance with the Helsinki Declaration.
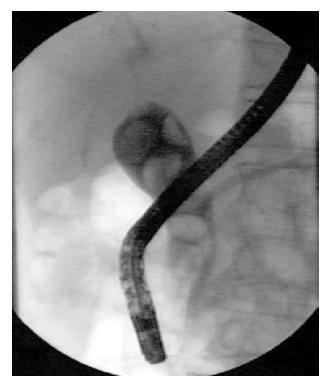
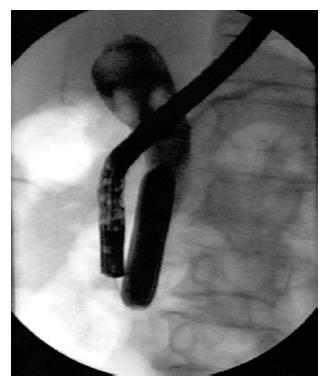
After diagnostic cholangiography at ERCP (Figure 1) using an Olympus video duodenoscope, a guidewire was passed through the diagnostic cannula into the bile duct. A balloon catheter (total length 200 cm) with a balloon dilator (diameter: 20 mm; length: 5 cm; Boston Scientific Corp., Watertown, MA) was then passed over the guidewire and positioned across the papilla. The balloon was then inflated little by little (Figure 2). Using a basket, CBD stones were extracted (Figure 3). The small fragments were extracted by an 8 wire basket (Memory Helical stone extractor basket, Cook Endoscopy, Winston-Salem, USA). Then smaller stones were retrieved or pulled out by a balloon catheter. Patients were then examined by repeated cholangiography to determine the presence of any residual stones. As residual small stones in the bile duct were difficult to detect under fluoroscopic examination, washing with normal saline was carried out to clear the bile duct. During the procedure, isosorbide dinitrate was administered intravenously at a rate of 5 mg/h to relax the papilla because nitrates are known to have a dilating effect on the sphincter of Oddi[3]. After SES + EPLBD, patients were kept in the hospital for at least two days to observe whether pancreatitis or other complications arose. All patients received prophylactic antibiotics (cefoperazone sodium/sulbactam sodium) immediately after the procedure.
The bile duct was cleared completely in 87 of 88 patients (success rate: 99%). Complete stone removal was completed in one endoscopic session in 87 of 88 patients (99%) with large stones of more than 12 mm in diameter. This procedure failed in one patient with a stone in the cystic duct. The results of SES + EPLBD were as follows: Duct clearance 1/88 (99%); Immediate complications were Bleeding (excluded oozing) 1/88 (1%); Acute pancreatitis 1/88 (1%); Acute cholangitis 1/88 (1%); Perforation 0/88 (0%); Injured bile duct Case 1/88 (1%); Hypoxia 1/88 (1%); Hypotension 10/88 (11%). Mechanical lithotripsy was used to extract stones in only this failed case. There was no basket impaction at the sphincter orifice. Procedure time ranged from 12-71 min. Mean procedure time in the last 30 patients was 25 ± 6 min.
Acute cholangitis after the treatment was observed in one patient, who had combined therapy, but no endoscopic treatment was needed in this case and the patient’s condition improved through the use of an antibiotic drip.
Transient abdominal discomfort was noted in 48 patients during large balloon dilation. There were some instances of oozing, but no procedure related hemorrhage was seen immediately after SES + EPLBD or after the stone clearance. Slight acute pancreatitis occurred in 1 patient (1%) after the procedure. This patient needed 3 d of fasting. One 58 year-old required endoscopic hemostasis by clipping because of bleeding at the papilla 3 d after the procedure. However, he did not need a blood transfusion and did not have hypotension. He was discharged 3 d after hemostasis. Hypotension (below 90 mm Hg) was observed in 10 of the patients (11%) receiving the procedure. Drip infusion of isosorbide dinitrate was immediately stopped to maintain normal blood pressure and the patients did not show any problems. There was one case of a small amount of leakage. In this case, there was a stenosis in the lower third of the bile duct. After dilation, a little leakage was recognized under X-ray. This patient had no clinical symptoms and normal laboratory data. No other complications were seen in patients who had SES + EPLBD.
EST is the commonly accepted therapy for the extraction of CBD stones. It has many early complications including bleeding, pancreatitis, and perforation[2-11]. Nonsurgical alternatives, including EPD by balloon[12], and medical sphincter dilation by nitroglycerin spray or drip infusion have also been described[3,13]. These dilation methods have some limitations in regard to the size and number of stones[14]. It is difficult to extract large and multiple stones from the bile duct by 10-8 mm balloon dilation. In this new treatment, in addition to small ES, we applied large balloon (20 mm) dilation to facilitate extraction of large and multiple stones without lithotripsy. This technique was originally presented in English at the DDW in 2004[15]. This new data on SES + EPLBD cases reveals an acceptable complication rate.
Mathuna et al[16] reported that the size of common bile duct stones to be extracted by EPD alone was smaller (mean size: 8 mm) and observed that EPD alone was unsuccessful in clearing the bile duct in 1 or 2 sessions in 18% of patients. On the other hand, combining SES + EPLBD, the mean size of stones extracted in our study increased to 20 mm without the need for mechanical lithotripsy. Moreover, the treatment could be performed in only one session.
Balloon dilation alone causes an acute transmural inflammatory response and intramucosal hemorrhage as described in a previous study[17]. A small ES frees access to the common cannel. It is reasonable to conclude that less injury to the pancreatic duct was produced in the sphincter of Oddi by large balloon dilation when small ES was combined during the procedure. This may cause fewer pancreatic complications compared to ES and balloon dilation alone.
Baron et al[18] and Vlavianos et al[19] reported that EPD was associated with an unacceptable rate of pancreatitis, and subsequent studies reported that the incidence of acute pancreatitis was 5%-7%[13,17]. Using combined therapy, we experienced only one patient who developed pancreatitis (1%). Hypotension is a common side effect of isosorbide nitrate in patients and healthy individuals[13]. Ten out of 88 patients (11%) developed hypotension during the procedure, requiring immediate discontinuation. Blood pressure should be monitored continuously while patients undergo dripping of isosorbide nitrate and sedation.
To clear fragments of stones from the bile duct after dilation, washing by normal saline was performed in all patients. Consequently, only one instance of cholangitis was observed in all patients without biliary drainage, suggesting that large dilation might be useful in preventing post procedural cholangitis. More cases are needed to ascertain the complete safety of not inserting a plastic stent or nasal biliary drainage tube after CBD stone extraction. Washing the bile duct was performed to identify missed stones that were subsequently removed and was found to be effective in reducing stone recurrence.
In our experience, the use of SES + EPLBD resulted in a mean procedure time of 30 min in all cases, except for 7 B-II cases. Stone extraction with SES + EPLBD was faster compared to ES and EPD alone for large stones (> 12 mm in diameter). Procedure time is expected to decrease if the technique is applied frequently in a large series of patients.
In conclusion, the results indicated that SES + EPLBD therapy may decrease complications associated with the extraction of large and multiple stones. We speculate that EPLBD combined with small ES may be easier to perform and more efficacious than EPD and ES alone for the extraction of large and multiple stones, but this remains to be seen in future studies for diverticulum cases and lower bile duct stenosis cases.
S- Editor Zhu LH L- Editor Alpini GD E- Editor Ma WH
| 1. | Classen M, Demling L. Endoscopic sphincterotomy of the papilla of vater and extraction of stones from the choledochal duct (author's transl). Dtsch Med Wochenschr. 1974;99:496-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 391] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 2. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1687] [Article Influence: 58.2] [Reference Citation Analysis (2)] |
| 3. | Staritz M, Poralla T, Dormeyer HH, Meyer zum Büschenfelde KH. Endoscopic removal of common bile duct stones through the intact papilla after medical sphincter dilation. Gastroenterology. 1985;88:1807-1811. [PubMed] |
| 4. | Classen M. Endoscopic papillotomy--new indications, short- and long-term results. Clin Gastroenterol. 1986;15:457-469. [PubMed] |
| 5. | Miller BM, Kozarek RA, Ryan JA, Ball TJ, Traverso LW. Surgical versus endoscopic management of common bile duct stones. Ann Surg. 1988;207:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 81] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Sherman S, Ruffolo TA, Hawes RH, Lehman GA. Complications of endoscopic sphincterotomy. A prospective series with emphasis on the increased risk associated with sphincter of Oddi dysfunction and nondilated bile ducts. Gastroenterology. 1991;101:1068-1075. [PubMed] |
| 7. | Seifert E, Gail K, Weismüller J. Long term results after endoscopic sphincterotomy. Dtsch Med Wochenschr. 1982;107:610-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 46] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Riemann JF, Lux G, Förster P, Altendorf A. Long-term results after endoscopic papillotomy. Endoscopy. 1983;15 Suppl 1:165-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Rösch W, Riemann JF, Lux G, Lindner HG. Long-term follow-up after endoscopic sphincterotomy. Endoscopy. 1981;13:152-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Escourrou J, Cordova JA, Lazorthes F, Frexinos J, Ribet A. Early and late complications after endoscopic sphincterotomy for biliary lithiasis with and without the gall bladder 'in situ'. Gut. 1984;25:598-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 171] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Ikeda S, Tanaka M, Matsumoto S, Yoshimoto H, Itoh H. Endoscopic sphincterotomy: long-term results in 408 patients with complete follow-up. Endoscopy. 1988;20:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy. 1983;15 Suppl 1:197-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 146] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Ibuki Y, Kudo M, Todo A. Endoscopic retrograde extraction of common bile duct stones with drip infusion of isosorbide dinitrate. Gastrointest Endosc. 1992;38:178-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Bergman JJ, Rauws EA, Fockens P, van Berkel AM, Bossuyt PM, Tijssen JG, Tytgat GN, Huibregtse K. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet. 1997;349:1124-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 274] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 15. | Minami A, Okuyama T, Hirose S. Small Sphincterotomy Combined with Papillary Dilation with Large Balloon Permits Retrieval of Large Stones Without Crushing Them. Gastrointest Endosc. 2004;59:AB200. [DOI] [Full Text] |
| 16. | Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 146] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Mac Mathuna P, Siegenberg D, Gibbons D, Gorin D, O'Brien M, Afdhal NA, Chuttani R. The acute and long-term effect of balloon sphincteroplasty on papillary structure in pigs. Gastrointest Endosc. 1996;44:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 212] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 19. | Vlavianos P, Chopra K, Mandalia S, Anderson M, Thompson J, Westaby D. Endoscopic balloon dilatation versus endoscopic sphincterotomy for the removal of bile duct stones: a prospective randomised trial. Gut. 2003;52:1165-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 89] [Article Influence: 4.0] [Reference Citation Analysis (0)] |