INTRODUCTION
Oesophageal ulcers occur mainly as a result of gastro-oesophageal reflux disease (GERD). However, pill-induced oesophageal ulcers are a fairly common event and more than 1000 cases have been reported in the literature[1]. The lesion is mainly due to entrapment of the pill and/or its chemical composition thereof. In fact, the risk factors for damage to the oesophageal mucosa include patient factors, such as advanced age, institutionalized condition, pre-existing oesophageal or swallowing disorders (GERD and hiatal hernia, dysphagia, achalasia, oesophageal strictures, etc) and cardiomegaly; drugs and their formulation factors, such as antibiotics and antivirals, non-steroidal anti-inflammatory drugs (NSAIDs) and many other chemicals including alendronate and potassium chloride; situational and administration factors, such as associated use of alco-hol, insufficient liquid bolus, recumbent position[2]. To our knowledge, no oesophageal lesions induced directly by homeopathic medications have been reported so far.
CASE REPORT
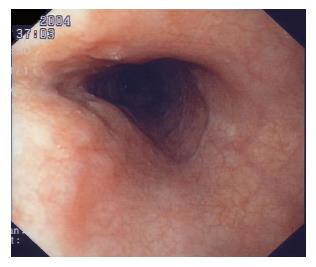
A 35-year old female came to our attention due to 3 d. standing chest pain, dysphagia and mild fever (37.5°C). No previous history of oesophageal disorders or gastro-oesophageal reflux symptoms or alcohol use was reported. The patient appeared to have pain. Physical examination revealed no change in blood pressure, respiratory or heart frequency. Routine chest X-ray and ECG were normal, laboratory tests were in the normal range, except for complete blood cell count which revealed an increase in relative neutrophils (76%). However, the patient was hospitalized and, the next day, an upper endoscopy was performed which revealed a longitudinal flat ulcer with regular margins covered with fibrin, located in the middle third of the oesophagus, with no macroscopic signs of oesophagitis (Figure 1). Indeed, the oesophageal junction as well as the gastric and duodenal mucosa appeared macroscopically normal. A more detailed investigation of the case history revealed that, during the three days prior to the onset of symptoms, the patient took homeopathic medication prescribed by a physician with the intent to treat a state of mild anxiety. From the first assumption of the pill she experienced a kind of oesophageal organ sensation and/or a very mild dysphagia.
Figure 1 Flat longitudinal ulcer covered with fibrin, located in middle third of the oesophagus.
The pill composition includes the following eight different herb components: magnolia officinalis cortex, scutellaria baiacalensis, ligusticum wallichii, escholzia californica, poria pararadicis sclerotium, ziziphus spinosa, polygala tenuifolia alba, biota semen.
The patient was put on a liquid diet and treated with 40 mg/d omeprazole i.v. and oral liquid sucralfate twice daily for 2 d. A clear improvement in symptoms was obtained within 24 h of treatment. The patient was discharged from the hospital after 64 h with a very mild residual dysphagia, but complete disappearance of the retrosternal chest pain. After three weeks, during which the patient was taking only 40 mg/d oral dose of omeprazole, upper endoscopy was repeated which revealed complete healing of the oesophageal ulcer (Figure 2).
Figure 2 Endoscopy after three weeks showing complete healing of mucosa.
DISCUSSION
Drug-induced oesophageal ulcer has been reported in 22.7% of patients with oesophageal ulcer, mostly localized in the middle third of the oesophagus, with a mean dimension of almost 2.9 cm[2]. Age range of patients, reported in most studies is 56-66 years, whereas, drug-induced oesophageal ulcers in young healthy individual are rare[2-5]. In the present case, also due to the absence of any oesophageal motility symptom in her history, all the most common patient-related risk factors could be excluded[6] and only drug formulation factors appeared to be the only determinant factors for inducing the oesophageal mucosa injury[7-11]. Drug composition and their formulation may affect oe-sophageal mucosa in many ways, all resulting in local mucosa alterations. Acidic chemicals and drugs with a fast dissolution rate can expose the mucosa to an increased risk of damage. The formulation of capsules have been reported to be more sticky than tablets[9], dosage and dimension may also be considered as possible risk factors[10,11]. Many types of drugs such as NSAIDs, bisphosphonates, potassium chloride, ferrous sulfate, nifedipine and antibiotics such as tetracyclines, erythromycin, amoxicillin, clavulanate, have been reported to be potentially dangerous for the oesophageal mucosa, particularly alendronate, in elderly patients[8,12,13]. Moreover, agents such as quinidine, anti-psychotics, clozapine and botilium toxin can induce swallow-ing dysfunction and dyskinesia, enhancing pill entrapment and mucosal lesions[2].
Administration factors, such as concomitant alcohol ingestion, recumbent position, frequent doses of a multiple medication and prolonged contact of the drug with the mucosa although the mucosa injury mechanisms may be considered important[2] were not present or not taken into account as determinant factors in the present case. A very small amount of water swallowed with any kind of pill, is sufficient to produce oesophageal injury, often with further associated factors. However, it was not the case in this patient, who reported that ingestion of the pill with a relative high dimension was accompanied with ache after drinking almost 200 mL of water. However, we cannot exclude that the relevant size of the pill (Figure 3) would have needed more water to avoid its entrapment in the mid-oesophagus.
Figure 3 Homeopathic pill dimension (2.
3 cm in length and 0.4 cm in width).
It is important, in the present case, to bear in mind the particular composition of the pill that includes eight different components with unspecified concentration. We looked at each specific component of the pill and no data on their potential effects on gastrointestinal mucosa have been reported in the consulted literature. Specifically, for the scutellaria baiacalensis, hepatic toxicity has been associated with therapeutic ingestion and neurologic side-effects after overdose assumption. For the Ligusticum wallichii, from which three different alkaloids have been isolated, an associated uterus contraction effect in experimental animals could suggest a potential motility interference also in human muscle layers[14,15]. However, the effects of their combination on the gastrointestinal mucosa in one pill are quite impossible to predict.
In conclusion, the potential individual or combined effects of these substances, as many other alternative remedies, on the oesophageal mucosa, are largely unknown, thus a direct aggressive effect of any single or combina-tion of the supposed innocuous herb-derived substances cannot be excluded. The present case reveals that pill entra-pment can occur even in the oesophagus of healthy young individuals and that oesophageal mucosal ulcer can be triggered by substances generally thought by the prescriber, not to have any aggressive side-effects on the gastrointestinal mucosa.