Published online Feb 14, 2006. doi: 10.3748/wjg.v12.i6.979
Revised: June 15, 2005
Accepted: July 8, 2005
Published online: February 14, 2006
We report here a very rare case of intestinal Behcet’s disease with pyoderma gangrenosum. A 16-year-old woman who was diagnosed with intestinal Behcet’s disease by the presence of cutaneous pathergy together with two major criteria (oral and genital aphthoses) and one minor criterion (gastrointestinal manifestations), was referred to our hospital with a left lower leg ulcer and abdominal pain in September 1989. Colonoscopy demonstrated flare-up colitis involving the entire colon. Her lower leg lesion was a painful destructive ulcer with an irregular margin and a ragged overhanging edge. Based on these clinical and laboratory findings, we diagnosed her cutaneous ulcer as pyoderma gangrenosum developing with exacerbated intestinal Behcet’s disease. Her cutaneous and intestinal lesions were poorly controlled though she received oral prednisolone treatment for a month. Because of aggravated abdominal symptoms with peritoneal irritation, we performed total colectomy in November 1989. The resected specimen was histologically compatible with intestinal Behcet’s disease showing severe inflammation with deep ulcerations and neutrophil accumulation. Subsequently, pyoderma gangrenosum rapidly improved. This clinical course may suggest the close relationship between pyoderma gangrenosum and intestinal Behcet’s disease.
- Citation: Nakamura T, Yagi H, Kurachi K, Suzuki S, Konno H. Intestinal Behcet’s disease with pyoderma gangrenosum: A case report. World J Gastroenterol 2006; 12(6): 979-981
- URL: https://www.wjgnet.com/1007-9327/full/v12/i6/979.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i6.979
Behcet's disease is a multi-system inflammatory disorder of unknown origin, characterized by recurrent oral and genital ulcerations, ocular and cutaneous lesions, arthritis and vascular disease. Cases of Behcet’s disease cluster along the ancient Silk Road, which extends from eastern Asia to the Mediterranean basin[1-3]. It is often difficult to distinguish Behcet’s disease from other inflammatory bowel diseases. Pyoderma gangrenosum is an idiopathic ulcerative skin disease. Because the histological findings of pyoderma gangrenosum are nonspecific and no laboratory confirmation exists, the diagnosis is based primarily on its clinical manifestations. Though this skin lesion is known to be associated with inflammatory bowel diseases, such as ulcerative colitis and Crohn’s disease, pyoderma gangrenosum is very rare in Behcet’s disease patients. We present a patient with extensive pyoderma gangrenosum whose skin lesions were resolved after surgical removal of the inflamed intestinal lesions.
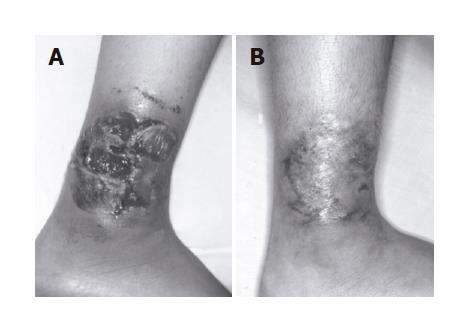
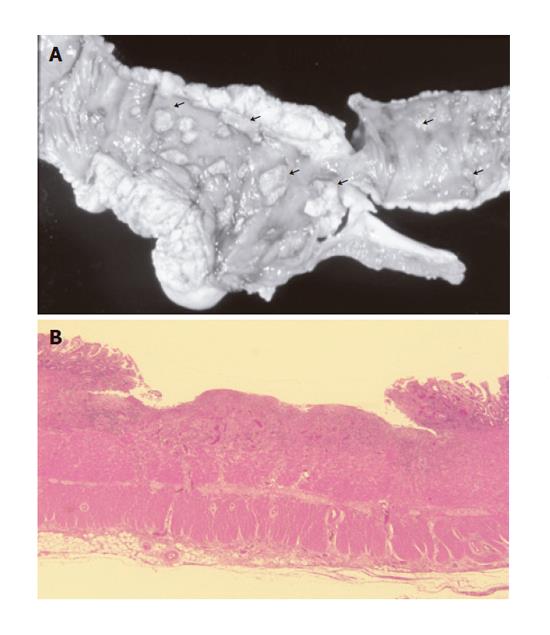
A 16-year-old woman was referred to our hospital in September 1989 due to painful ulceration on the left foot and lower abdominal pain. She was diagnosed with intestinal Behcet’s disease by the presence of cutaneous pathergy together with two major criteria (oral and genital aphthoses) and one minor criterion (gastrointestinal manifestations) in 1984. Her lower leg lesion was a painful destructive ulcer with an irregular margin and a ragged overhanging edge (Figure 1A). She was negative for repeated bacterial, fungal and viral cultures. Colonoscopy demonstrated flare-up colitis involving the entire colon. Based on these clinical and laboratory findings, her skin lesion was considered pyoderma gangrenosum developing with aggravation of her intestinal Behcet’s disease. She was treated with prednisolone (20 mg orally per day) for a month, but the skin lesion was poorly controlled. In November 1989, she complained of severe abdominal pain and melena. Laboratory data showed a white blood cell count of 14900/mm3, serum C-reactive protein of 4.5 mg/dL and hemoglobin of 12.3 g/dL. Because her abdominal symptoms were aggravated with peritoneal irritation, we performed a total colectomy with partial ilealectomy and ileo-rectal anastomosis. The resected specimen revealed severe inflammation with punched-out ulcerations of the colon and ileum (Figure 2A). Microscopic findings showed active colitis with neutrophil accumulation around the ulcer beds. Subsequently her abdominal symptoms gradually improved. Surprisingly, intractable ulceration of the left foot disappeared without scarring within two weeks after the surgery (Figure 1B). She was discharged with an uneventful postoperative course. Relapse of pyoderma gangrenosum has not been observed for 10 years after surgery.
Intestinal Behcet’s disease has been categorized in a family with inflammatory bowel disease, and causes abdominal pain, diarrhea, melena and even perforation. The ileocecal region is the most commonly affected part of the gastrointestinal tract, but the distal colon may also be involved. It is often difficult to distinguish Behcet’s disease from the other inflammatory bowel diseases because of the similar extra-intestinal manifestations including oral aphthosis, uveitis and arthritis. Genital ulceration and positive pathergy test are the extra-intestinal features of Behcet’s disease alone, which are not seen in the other inflammatory bowel diseases. Our patient was diagnosed as Behcet’s disease by the presence of cutaneous pathergy together with two major criteria (recurrent oral and genital aphthoses) and one minor criterion (gastrointestinal manifestations)[4].
In Behcet’s disease, multiple cutaneous lesions, such as erythema nodosum, folliculitis and pustules are seen, but pyoderma gangrenosum is very rare. Pyoderma gangrenosum in the present case did not respond to oral corticosteroids but was improved soon after the resection of inflamed intestinal lesions. Since the first report by Munro and Cox in 1988[5], four cases of pyoderma gangrenosum associated with
Behcet’s disease have been reported in English literature[6-8] (Table 1). Behcet’s disease always precedes the onset of pyoderma gangrenosum. These patients are treated with corticosteroids, immunosuppressants or thalidomide. It was reported that cases of pyoderma gangrenosum had no improvement after surgical removal of the intestinal lesions[9]. Pyoderma gangrenosum usually responds to systemic corticosteroids and may also be rapidly improved by surgical resection of the associated diseases, such as ulcerative colitis and Crohn’s disease. Therefore, the activity of pyoderma gangrenosum is closely related to the activity of associated diseases. In the present case, pyoderma gangrenosum rapidly improved after total colectomy. The skin manifestations of Behcet’s disease are classified as neutrophilic vascular reaction[10]. The pathergy test is useful for evaluating skin irritability and is a diagnostic criterion of Behcet’s disease. However, this test can also be positive in other diseases such as Sweet’s syndrome and pyoderma gangrenosum. Pyoderma gangrenosum is a form of cutaneous vasculitis[11] and accumulation of neutrophils and mononuclear cells is observed at the reaction site. In both Behcet’s disease and pyoderma gangrenosum, primary pustular lesions can occur and neither of them has a characteristic histological appearance. They may belong to the category of the neutrophilic dermatoses.
Though the relationship between Behcet’s disease and pyoderma gangrenosum is not referred in diagnostic criteria of Behcet’s disease, the occurrence of pyoderma gangrenosum may be highly relevant with the pathogenesis of Behcet’s disease.
We are grateful to Professors Shozo Baba and Keiji Iwatsuki for their excellent comments on the manuscript.
S- Editor Guo SY L- Editor Elsevier HK E- Editor Kong LH
| 1. | Kastner DL. Intermittent and periodic arthritic syndromes. Arthritis and allied conditions: a textbook of rheumatology. 13th ed. Vol. 1. Baltimore: Williams & Wilkins 1997; 1279-1306. |
| 2. | Kaklamani VG, Vaiopoulos G, Kaklamanis PG. Behcet's Disease. Semin Arthritis Rheum. 1998;27:197-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 266] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 3. | Mizuki N, Inoko H, Ohno S. Pathogenic gene responsible for the predisposition of Behçet's disease. Int Rev Immunol. 1997;14:33-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet. 1990;335:1078-1080. [PubMed] |
| 5. | Munro CS, Cox NH. Pyoderma gangrenosum associated with Behçet's syndrome--response to thalidomide. Clin Exp Dermatol. 1988;13:408-410. [PubMed] |
| 6. | Lilford RJ, Tindall VR, Batchelor AG. Post-surgical pyoderma gangrenosum of the vaginal vault associated with ulcerative colitis and Behcet's disease; a case report. Eur J Obstet Gynecol Reprod Biol. 1989;31:93-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Rustin MH, Gilkes JJ, Robinson TW. Pyoderma gangrenosum associated with Behcet's disease: treatment with thalidomide. J Am Acad Dermatol. 1990;23:941-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Armas JB, Davies J, Davis M, Lovell C, McHugh N. Atypical Behçet's disease with peripheral erosive arthropathy and pyoderma gangrenosum. Clin Exp Rheumatol. 1992;10:177-180. [PubMed] |
| 9. | Levitt MD, Ritchie JK, Lennard-Jones JE, Phillips RK. Pyoderma gangrenosum in inflammatory bowel disease. Br J Surg. 1991;78:676-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 52] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | James DW, Walker JR, Smith MJ. Abnormal polymorphonuclear leucocyte chemotaxis in Behçet's syndrome. Ann Rheum Dis. 1979;38:219-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |