CASE REPORT
A 35-year-old female was hospitalized for abdominal pain, bloating, and vomiting. Plain X-ray pictures exhibited bowel obstruction for which she underwent emergency surgery. On the second postoperative day, she started to complain about dull right upper quadrant abdominal pain and bloating. Abdominal CT scans revealed very large cystic lesion with an inhomogeneous fluid content. The cyst occupied the whole right lobe of the liver compressing the surrounding organs and dislocating the left lobe of the liver towards the left hypochondrium (Figure 1). Additionally, several more cysts of various sizes were seen in the whole abdomen. This radio-morphology raised the possibility of a hydatid disease (caused by ruptured hydatid cyst) confirmed through positive echinococcus IgG serology (ELISA). Interestingly, no hypereosinophilia could be detected through repeated blood tests.
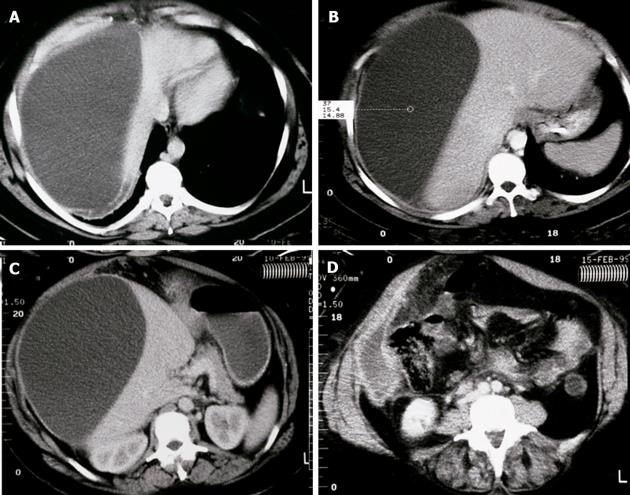
Figure 1 Abdominal CT scan.
A: Axial CT scan shows the large inhomo-geneous cystic fluid collection occupying the whole right lobe of the liver; B: CT scan of the cystic lesion on the level of spleen; C: the largest cystic lesion compresses the left lobe of the liver dislocating the nearby organs; D: cystic collection was seen also in the pararenal spaces and extended into the small pelvis.
Mebendazole (200 mg/d for 3 d) was administered in order to prevent anaphylactic reactions and the dissemination of the disease. After obtaining written consent from the patient, the site of the puncture was defined to the X–XI intercostal space. The procedure was performed under ultrasound guidance (Diasonics Master Series VST) and the patient was closely monitored for any sign of anaphylaxis. The cyst that was punctured on its free surface with an 18 gauge needle contained a dense whitish fluid. Samples were taken for parasitological examinations. Because of the huge size of the cyst, an 8F pigtail catheter (polyurethane drainage catheter, COOK) with 32 side holes was introduced into the cyst. After aspiration of 6 200 mL of the cystic fluid (Figure 2), 150 mL of 15% hypertonic saline was injected into the cyst cavity. Twenty minutes later, the catheter was attached to a vacuum tube and left for suction drainage. This cycle (hypertonic 15% saline injection and 20 min later reaspiration) was repeated daily with 40 mL 15% sterile saline. The initial procedure lasted for 30 min. At the end of the flushing series, absolute alcohol of 30 mL was injected and removed after 20 min during the last 5 days. During the procedure the patient remained symptomless and no anaphylactic reaction could be observed. Ultrasonographically, the cyst decreased in size gradually with only a 7.6 mm subcapsular fluid collection remaining under the right diaphragm. The total time of percutaneous drainage took 43 d.
Figure 2 A: The aspirated fluid (6 200 mL); B: drainage catheter with sucking bottle.
Under light microscopy, the aspirated cystic fluid showed clear evidence of hydatid scolices verifying the presumed diagnosis of echinococcosis. After 6 weeks of percutaneous drainage the catheter was removed. Abdominal CT scans exhibited total disappearance of the cyst. Subsequently, the patient was discharged and reported no symptom relapses on the follow-up period of 1 year.
DISCUSSION
Echinococcus granulosus is a small, 5-mm-long tapeworm being responsible for unilocular hydatid cyst disease. Human infection by E. granulosus occurs most commonly in sheep- and cattle-raising areas where dogs assist in herding; the infection is more frequent in Eastern Europe, the Mediterranean, Australia, New Zealand, Chile, Argentina, and Africa. Human beings are usually infected as intermediate hosts when they ingest egg-contaminated food or water. Over 50% of all human E. granulosus infections involve the liver[1]. Additional common sites for hydatid cysts are the lungs, spleen, kidneys, heart, bones, and brain[2].
Since hydatid cysts grow at a rate of about 1–5 cm/year, a long latent period is typical. The symptoms of hydatid disease are related primarily to the mass effect of the slowly enlarging cyst: right upper quadrant pain from the stretching hepatic capsule, jaundice from compression of the bile duct, or portal hypertension from portal vein obstruction. Following a presumably long latency, our patient presented with symptoms related to bowel obstruction caused by the space-occupying effect of the giant hydatid cyst. CT scans and ultrasonography are very useful for revealing well-defined cysts with thick or thin walls which correspond to our case as well[2]. The 6.2-L large cyst of our case is the largest hydatid cyst published in the literature. The visualization of daughter cysts within the larger cyst and the mural calcification helps to distinguish E. granulosus infection from carcinomas, bacterial or amebic liver abscesses, or hemangiomas[3]. Either spontaneously or as a result of a complication to surgery, free peritoneal rupture of the cyst can lead to fatal anaphylaxis. On the long term, leakage of the cyst may cause an intense antigenic response, resulting in eosinophilia, bronchial spasm, or anaphylactic shock.
Open surgical drainage of the hydatid cysts has been the preferred method of therapy. Several surgical techniques have been applied for the treatment of hydatid disease: simple-closure tube drainage, marsupialization, cystectomy, total pericystectomy, hepatic resection, and cavity management (omentoplasty, internal drainage)[4]. Among them, total pericystectomy was found to be the most effective method at reducing recurrence and improving resolution of the hepatic defect. The mortality rate after surgery ranges from 0% to 6.3%, while the rate of postoperative complications varies between 12.5% and 80%[4]. Jabbour et al [5] suggested that surgery should be the treatment of choice for large, multiple, complicated, and recurrent hydatid cysts of the liver.
The percutaneous treatment has been used in many hospitals as the alternative method to surgery[6]. A prospective randomized trial of 50 patients found that percutaneous drainage and hypertonic saline irrigation of the cysts combined with albendazole is as effective as surgical drainage, with fewer complications and shorter durations of hospitalization[7]. A long-term follow-up study has also confirmed the effectiveness of percutaneous drainage with mortality and morbidity rates more favorably than those of conventional surgical approaches[8]. The generally accepted and safe technique for percutaneous drainage is called PAIR that stands for puncture, aspiration of cyst, injection of hypertonic saline and absolute alcohol, and reaspiration[9]. Hypertonic saline exerts a scolicidal effect and prevents the formation of daughter cysts through the irrigation of the germinative layer[10]. Absolute alcohol is the agent of sclerotherapy against the wall of the hydatid cyst. Formerly, the percutaneous drainage of the hydatid cyst was deemed to be a hazardous procedure due to the potential risk of anaphylaxis and dissemination[11]. Filice and Brunetti[12], however, observed no anaphylactic reaction or peritoneal dissemination having applied the PAIR technique for 231 cysts in 163 patients. In agreement with this report, Haddad et al [13] experienced only minor complications including pain, mild fever, pleural effusion, and transient hypernatremia in their series. In a 6-9 year follow-up involving ultrasonography, CT scans, and serology tests, no local recurrence or spread of the disease were found[13]. Pelaez et al [14] successfully treated 55 hydatid cysts in the liver in 34 patients with the combination of PAIR technique and albendazole prophylaxis. They reported only urticaria and subcapsular hematoma as minor complications and the mean hospitalization duration was 1.82 d. Akhan et al [4,8]. reported good accuracy rate and low complication rate in the percutaneous treatment of hydatid disease. Using the percutaneous drainage treatment combined with mebendazole prophylaxis in our patient, we could successfully manage the largest hydatid cyst ever reported. The applied drainage method seems to be useful for the treatment of huge hydatid cysts and has also been recommended as an effective and safe therapeutic choice.
In summary, this patient has demonstrated that percutaneous drainage is the appropriate and feasible alternative to surgery in treating hydatid cysts even of this giant size with a low risk of severe complications.