Published online Feb 7, 2006. doi: 10.3748/wjg.v12.i5.791
Revised: May 29, 2005
Accepted: July 20, 2005
Published online: February 7, 2006
AIM: To evaluate the omeprazole maintenance therapy in patients with recurrent ulcer bleeding after surgery for duodenal ulcer.
METHODS: We studied 15 consecutive patients with recurrent ulcer bleeding after surgery for duodenal ulcer. Omeprazole (20 mg/d) maintenance therapy was given after ulcer healing. In addition to clinical follow-up, ambulatory 24-h gastric pH assay was performed before and during omeprazole therapy in those patients and controls with previous duodenal ulcer surgery but no ulcer recurrence.
RESULTS: All the 15 ulcers were healed after being treated with omeprazole (40 mg/d) for 2 mo. Eleven patients with two (1-9) episodes of recurrent ulcer bleeding completed the follow-up (43, 12-72 mo). None of them had a bleeding episode while on omeprazole. One patient discontinued the therapy and had recurrent bleeding. The median 24-h fraction time of gastric pH <4 in patients was 80, 46-95%, and was reduced to 32, 13-70% by omeprazole (P = 0.002).
CONCLUSION: Long-term maintenance therapy with omeprazole (20 mg/day) is effective in preventing recurrent ulcer bleeding.
- Citation: Demertzis K, Polymeros D, Emmanuel T, Triantafyllou K, Tassios P, Ladas SD. Omeprazole maintenance therapy prevents recurrent ulcer bleeding after surgery for duodenal ulcer. World J Gastroenterol 2006; 12(5): 791-795
- URL: https://www.wjgnet.com/1007-9327/full/v12/i5/791.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i5.791
H pylori eradication therapy and the use of potent proton pump inhibitors (PPIs) have dramatically reduced the need for surgical therapy of peptic ulcer disease. Still, about 10 % of duodenal ulcer patients undergo emergency surgical therapy for acute ulcer bleeding[1]. However, recurrent ulcer is not uncommon as it occurs in 10-15 % of patients after vagotomy and drainage and in 2-5 % of patients after gastric resection[2]. This may be complicated by life threatening acute recurrent ulcer bleeding in certain patients, requiring hospitalization.
Several studies have investigated the rate of ulcer recurrence after duodenal ulcer surgery[2,3] and the completeness of vagotomy[4,5], but only a few studies have evaluated the anastomotic ulcer healing rates after being treated with H2 receptor antagonists (H2RA)[6,7] or PPI[8] therapy. Studies have shown that H pylori infection of the gastric mucosa is not related to ulcer recurrence after gastric surgery[4,9,10]. Furthermore, it has been shown that 28 % of anastomotic ulcers recur within 6 wk after discontinuing cimetidine therapy[7], and 33% relapse within a year while on cimetidine maintenance therapy[6].
These patients are often treated with a second operation[1]. However, to the best of our knowledge, there are no studies investigating the long-term outcome of patients with recurrent post-surgical ulcer and whether maintenance acid suppression therapy with PPIs may prevent recurrent ulceration and/or re-bleeding. Therefore, the present prospective open label study was conducted to investigate gastric pH profile and the effect of omeprazole maintenance therapy in patients presented with recurrent ulcer bleeding after duodenal ulcer surgical therapy.
Over a 7-year period, this prospective open label study included 15 consecutive male patients admitted to our department due to recurrent acute ulcer bleeding. All patients underwent gastric surgery for duodenal ulcer disease at least 2 years ago.
In each case, emergency endoscopy was performed to confirm recurrent ulcer bleeding. The finding of an ulcer was considered as the bleeding cause if active bleeding or stigmata of recent hemorrhage were noted in the absence of other lesions. The recurrent ulcers were peristomal or duodenal in location. At the same time, detailed history was obtained about the indication and time of past gastric operation and the number of hospital admissions with hematemesis or melena after gastric surgery. History specifically included questions about the use of H2RA, PPIs or non-steroidal anti-inflammatory drugs (NSAIDs)[11], smoking and alcohol abuse. In all the patients fasting serum gastrin and salicylate concentrations were determined to exclude Zollinger–Ellison syndrome and recent consumption of non-steroidal antiinflam-matory drugs. Patients who were on non-steroidal anti-inflammatory drugs were excluded. During endoscopy, multiple gastric mucosal biopsies were obtained to investigate H pylori infection.
All patients were initially treated with intravenous omeprazole (20 mg every 12 h) and then orally after discharge from the hospital. H pylori eradication therapy was not used to prevent ulcer recurrence[10,12], but H pylori was eradicated in two patients because of severe H pylori gastritis. Follow-up endoscopy was scheduled at 2 mo, while on oral omeprazole (40 mg/d) to confirm ulcer healing. Thereafter, the patients were instructed to receive oral omeprazole (20 mg/d) maintenance therapy, to avoid the use of any non-steroidal anti-inflammatory drugs and to have follow-up every 6 mo as outpatients.
Twenty-four-hour gastric pH studies were performed in the following groups on omeprazole therapy (20 mg/d) but not on antisecretory therapy: patients with first or second degree reflux esophagitis (Los Angeles classification) (“normal” controls); patients with duodenal ulcer; controls who underwent vagotomy and pyloroplasty or gastrojejunostomy for duodenal ulcer but had no ulcer recurrence; controls who had Billroth II partial gastrectomy and patients who had recurrent anastomotic ulcer bleeding after gastric surgery for duodenal ulcer. In the latter group of patients (test group), 24-h gastric pH studies were performed while on omeprazole (40 mg/d, 20 mg/d). Omeprazole was then discontinued and the patients were treated with ranitidine 150 mg twice daily for 2 d, followed by a 2-d washout period before the pH study in patients not on antisecretory therapy. The duodenal ulcer group included patients admitted to our department for acute ulcer bleeding and volunteered to have 24-h pH studies. The vagotomy and gastrectomy control groups included patients who attended the outpatient clinic for various epigastric symptoms and volunteered to participate in the study after having a negative gastroscopy.
Gastric ambulatory pH monitoring was performed using a monocrystalline antimony pH catheter. The electrode was passed transnasally into the stomach, 10-15 cm below the detectable esophagogastric junction by endoscopy. The catheter was connected to a portable pH-recording device (Digitrapper Mk III, Synectics Medical AB, Stockholm, Sweden). Recorded data were uploaded into the "EsopHogram Analysis Software” for analysis and review. During the 24-h pH studies, patients were encouraged to keep up their usual activities and diet in order to maximize the diagnostic yield of the test. The 24-h fraction (%) time when the gastric pH was below 4 was calculated.
All patients and volunteers gave oral consent after being informed of the purpose of the study by the investigator. The study protocol was approved by the Ethics Committee on Human Studies, Department of Internal Medicine, Medical School of the Athens University. The trial was conducted according to the declarations of Helsinki.
We used non-parametric statistics [“Statgraphics-Plus” version 4 for Windows (Manugistics Inc., Rockville, USA)], because of the small number of observations included in each group. Results were presented as median with ranges. We used the non-parametric Mann-Whitney (Wilcoxon) two-sided U-test and the Kruskal-Wallis t-test for two and multiple-sample comparison analysis, respectively[13]. P < 0.05 was considered statistically significant.
Over a 7-year period, 15 consecutive male patients with recurrent ulcer bleeding after surgery for duodenal ulcer were admitted to our department because of acute bleeding episode. Serum gastrin was normal and salicylates were not detected in the serum in any of the 15 patients during their hospitalization. In addition, all patients denied the use of non-aspirin, non-steroidal anti-inflammatory drugs after thorough interrogation.
Ulcer in all the 15 patients was healed after treatment with omeprazole (40 mg/d) for 2 mo. However, four of them did not consent to gastric pH studies and were lost to clinical follow-up within the first year from entering the study. Therefore, data were presented for 11 patients (Table 1).
| Case | Age(yr) | Smokingstatus | H. pyloristatus | Type ofoperation | Yearssince operation | Bleedingepisodes after Surgery | Follow-up(mo) |
| 1 | 62 | Never | Positive1 | TV+D2 | 5, 23 | 3 | 72 |
| 2 | 60 | Ex-smoker | Positive | TV+D | 6 | 8 | 62 |
| 3 | 61 | Smoker | Positive1 | BII | 2 | 1 | 61 |
| 4 | 66 | Never | Negative | BII+V2 | 4, 33 | 2 | 56 |
| 5 | 49 | Smoker | Positive | TV+D | 7 | 1 | 52 |
| 6 | 70 | Ex-smoker | Negative | BII | 18 | 2 | 43 |
| 7 | 64 | Never | Negative | BII | 3 | 2 | 35 |
| 8 | 59 | Ex-smoker | Negative | BII | 16 | 4 | 32 |
| 9 | 66 | Smoker | Negative | TV+D | 7 | 5 | 28 |
| 10 | 52 | Ex-smoker | Positive | TV+D | 5 | 2 | 18 |
| 11 | 48 | Ex-smoker | Negative | TV+P | 13 | 9 | 12 |
Two out of the eleven patients had a history of two gastric operations because of recurrent ulcer bleeding. The time of recurrent ulcer bleeding after gastric surgery was 6 years, averaged 2-18 years. The number of hospital admissions because of post surgical ulcer bleeding was 2, averaged 1-9. At study entry, 3/11 patients were smokers and 5/11 were H pylori-positive. H pylori was successfully eradicated in two of these five patients upon admission to the study. One of the H pylori-negative patients had successful triple eradication therapy at another hospital a year ago.
No recurrent ulcer or re-bleeding occurred during the maintenance therapy (omeprazole 20 mg/d) over the follow-up period (43 mo, averaged 12-72 mo). One patient discontinued treatment and had recurrent bleeding 8 mo after stopping omeprazole. Currently, he was symptom-free on omeprazole maintenance therapy. There were no significant adverse events related to treatment.
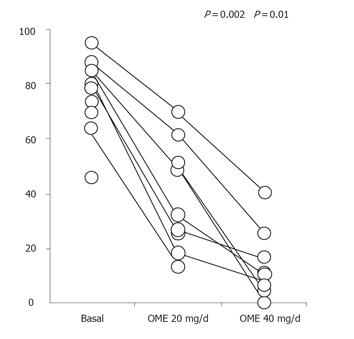
Results of the 24-h intragastric pH monitoring studies are shown in Table 2. The “normal” control group included 10 patients with first or second degree reflux esophagitis, who were matched for age, sex and H pylori status with the recurrent post-surgical ulcer patients. They were selected from a pool of patients with reflux esophagitis on 24-h esophageal-gastric pH monitoring. The duodenal ulcer control group included seven patients hospitalized because of duodenal ulcer bleeding. The vagotomy control group included seven patients who had truncal vagotomy and drainage for duodenal ulcer. The gastrectomy control group included seven patients who had partial gastrectomy (Billroth II) for duodenal ulcer. Volunteers of the vagotomy and gastrectomy control groups studied at least 2 years postoperatively had no postoperative ulcer recurrence. The test group included ten of the eleven patients who had truncal vagotomy (n = 5) or Billroth II gastrectomy (n = 5) and recurrent anastomotic ulcer bleeding. Intolerance to nasogastric pH probe was not studied in another patient who had vagotomy and drainage. There were three failures out of 30 24-h gastric pH recordings in the test group, as shown by missing values in Figure 1. One of the vagotomy controls refused to have the 24-h pH study on omeprazole.
| Groups studied | Numberofpatients | Age(yr) | H pylori(+) | Treatment-free(baseline) | Omeprazole20 mg/d | Pvalue |
| Normal controls | 10 | 60, 47 – 73 | 2/9 | 87.7, 71.3 – 98.5 | 34.6, 4.3 – 72.7 | <0.001 |
| Duodenal ulcer controls | 7 | 61, 38 – 71 | 7/7 | 92.3, 86.6 – 98.8 | 45.2, 25.8 – 72.0 | 0.002 |
| Vagotomy controls2 | 7 | 54, 41 – 72 | 2/6 | 72.8, 34.0 – 87.3 | 17.8, 6.5 – 35.1 | 0.005 |
| Gastrectomy controls | 7 | 66, 46 – 72 | 1/7 | 6.2, 4.6 – 39.6 | ND1 | |
| Vagotomy patients | 5 | 57, 49 – 72 | 3/5 | 84.9, 79.1– 95.2 | 49.4, 18.3 – 69.9 | 0.012 |
| Gastrectomy patients | 5 | 68, 61 – 72 | 0/5 | 69.8, 45.8 | – 85.2 28.8, 13.3 – 51.3 | 0.037 |
The 24-h gastric pH measurements of the groups studied during treatment-free period are shown in Table 2. There was a statistically significant difference in the 24-h fraction time of gastric pH < 4 among the six groups (T = 29.10, P < 0.001), with the lowest values recorded in the Billroth II gastrectomy control group. Patients who had vagotomy and recurrent ulcer bleeding had a significantly different (higher) 24-h fraction time of gastric pH < 4 as compared to vagotomy controls (U = 32, P = 0.023). This difference was also significant when bleeding patients after gastrectomy were compared to those of the gastrectomy control group (U = 35, P = 0.006).
Gastric pH studies were performed in the control and patient (test) groups on omeprazole (20 mg/d). Billroth II gastrectomy control group did not undergo this study because of the low fraction time of gastric pH <4 recorded during treatment-free gastric pH monitoring. Omeprazole therapy (20 mg/d) significantly reduced the 24-h fraction time of gastric pH < 4 in both control and patient groups (Table 2).
Eight out of the ten patients underwent all (baseline 20 mg/day and 40 mg/day omeprazole) 24-h gastric pH studies. One additional patient underwent only baseline, and another patient both baseline and omeprazole (20 mg/day) 24-h gastric pH studies. Individual data are shown in Figure 1. The 24-h fraction time of gastric pH < 4 (80, 46 - 95%) was significantly reduced by omeprazole (20 mg/d) to 32, 13 - 70% (U = 6, P = 0.002) and by omeprazole (40 mg/d) to 11, 1- 40% (omeprazole 20 mg/day vs 40 mg/day, U = 9, P = 0.01).
The data of the present study showed that recurrent ulcers after gastric surgery for duodenal ulcer can heal after 2 months of 40 mg/day omeprazole therapy. Even more important, none of our patients had a re-bleeding episode while on omeprazole maintenance therapy over a 3.5-year follow-up period.
A large review is available on the complications associated with ulcer recurrence following gastric surgery including 130 studies published on this topic over a 30-year period[14]. The authors estimated that vagotomy plus drainage is associated with a 9 % recurrence rate and a risk of hemorrhage of 1.7 %. Partial gastrectomy has a lower recurrence rate (< 1 %) but a similar risk of hemorrhage (1.3 %). Such patients with recurrent ulcer bleeding are often submitted to a second gastric operation to cure recurrent ulcer. Similarly, most of our patients had a history of two or more hospital admissions for recurrent ulcer bleeding after surgery and two of them had a second gastric operation that failed to cure recurrent ulcer. Cimetidine has been used in a few clinical trials including a small number of patients with recurrent ulcer bleeding following surgery for peptic ulcer disease[6,7,15-17]. Cimetidine heals about 85 % of ulcers within 8 weeks[17], but about 30 % of ulcers relapse within 6 months after discontinuing therapy[7,17]. Furthermore, 33 % of ulcers recur 1 year after surgery while on cimetidine maintenance therapy[6], probably because of tolerance to H2RA, which is more significant after 4 wk of therapy[18]. Finally, there is only one clinical trial using omeprazole therapy for 12 patients with recurrent ulcer after vagotomy or gastrectomy and all ulcers are healed after 8 weeks of omeprazole therapy[8], suggesting that maintenance therapy with PPIs is the only alternative for surgical intervention. Since as many as one-third of patients with anastomotic ulcer have recurrent ulcer within a year after discontinuing acid reduction therapy[6,15], an open trial of PPI maintenance treatment should be considered ethically justifiable.
The role of H pylori in recurrent peptic ulcer disease after gastric surgery has been investigated in several clinical studies[9,10,12,19], showing that H pylori does not play an important role in post surgical ulcer recurrence. Less than half of our patients with recurrent ulcer bleeding were H pylori-positive upon admission to the study. Furthermore, one of our patients who had successful H pylori eradication therapy during a previous hospitalization was admitted to our department for a new episode of anastomotic ulcer bleeding. Another patient had two gastric operations for recurrent ulcer bleeding. Upon study entry, he had successful H pylori eradication therapy, followed by omeprazole (20 mg/d) maintenance therapy. He was healthy for 2 years and then lost his follow-up. He was readmitted to another hospital for recurrent ulcer bleeding 8 mo after discontinuing PPI maintenance therapy, though he was H pylori-negative.
With regard to the underlying mechanism of ulcer recurrence, our study showed that patients with recurrent ulcer bleeding after truncal vagotomy or partial gastrectomy had a higher treatment-free 24-h intragastric acidity than controls with no ulcer recurrence after the same operation, suggesting that vagotomy may be incomplete due to a retained antrum[20,21]. Our data showed that ulcer healing therapy with omeprazole (40 mg/d) could strongly inhibit gastric acid secretion. The intragastric acidity could also be significantly reduced with oral omeprazole maintenance treatment (20 mg/d).
Other factors that may be implicated in ulcer recurrence after surgical treatment for duodenal ulcer include a decreased resistance to acid in the jejunal mucosa, the site of pyloroplasty and anastomosis, possibly due to local ischemia and scarring. Hirschowitz and Lanas[11] also showed that aspirin abusers develop intractable recurrent ulceration following gastric surgery for peptic ulcer disease. However, our patients refused to use non-steroidal anti-inflammatory drugs and their serum salicylates were negative. Zollinger-Ellison syndrome was also excluded by normal fasting serum gastrin.
In conclusion, omeprazole (20 mg/d) maintenance therapy should be the treatment of choice for patients with recurrent ulcer after gastric surgery for duodenal ulcer disease.
S- Editor Wang XL and Guo SY L- Editor Elsevier HK E- Editor Wu M
| 1. | Rockall TA. Management and outcome of patients undergoing surgery after acute upper gastrointestinal haemorrhage. Steering Group for the National Audit of Acute Upper Gastrointestinal Haemorrhage. J R Soc Med. 1998;91:518-523. [PubMed] |
| 2. | McFadden DW, Zinner MJ. Reoperation for recurrent peptic ulcer disease. Surg Clin North Am. 1991;71:77-92. [PubMed] |
| 3. | Emås S, Eriksson B. Twelve-year follow-up of a prospective, randomized trial of selective vagotomy with pyloroplasty and selective proximal vagotomy with and without pyloroplasty for the treatment of duodenal, pyloric, and prepyloric ulcers. Am J Surg. 1992;164:4-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Peetsalu M, Maaroos HI, Peetsalu A. Completeness of vagotomy, Helicobacter pylori colonization and recurrent ulcer 9 and 14 years after operation in duodenal ulcer patients. Eur J Gastroenterol Hepatol. 1998;10:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Gobet B, Malikova E, Mignon M, Vatier J. Gastric secretory investigation of recurrent ulcer after surgery for duodenal ulcer. Hepatogastroenterology. 1991;38:522-527. [PubMed] |
| 6. | Berstad A, Aadland E, Bjerke K. Cimetidine treatment of recurrent ulcer after proximal gastric vagotomy. Scand J Gastroenterol. 1981;16:891-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Stage JG, Henriksen FW, Kehlet H. Cimetidine treatment of recurrent ulcer. Scand J Gastroenterol. 1979;14:977-979. [PubMed] |
| 8. | Sugiyama M, Katamura H. [Recurrent peptic ulcer after gastric surgery]. Nihon Rinsho. 1992;50:144-153. [PubMed] |
| 9. | Lee YT, Sung JJ, Choi CL, Chan FK, Ng EK, Ching JY, Leung WK, Chung SC. Ulcer recurrence after gastric surgery: is Helicobacter pylori the culprit. Am J Gastroenterol. 1998;93:928-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Sito E, Konturek PC, Konturek SJ, Bielański W, Stachura J. Helicobacter pylori infection after gastrectomy and vagotomy in duodenal ulcer patients. J Physiol Pharmacol. 1996;47:229-237. [PubMed] |
| 11. | Hirschowitz BI, Lanas A. Intractable upper gastrointestinal ulceration due to aspirin in patients who have undergone surgery for peptic ulcer. Gastroenterology. 1998;114:883-892. |
| 12. | Leivonen MK, Haglund CH, Nordling SF. Helicobacter pylori infection after partial gastrectomy for peptic ulcer and its role in relapsing disease. Eur J Gastroenterol Hepatol. 1997;9:371-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Armitage P, Berry G. Statistical methods in medical research. 2nd ed. London: Blackwell Sci Pub 1987; 713-722. |
| 14. | Penston JG, Boyd EJ, Wormsley KG. Complications associated with ulcer recurrence following gastric surgery for ulcer disease. Gastroenterol Jpn. 1992;27:129-141. [PubMed] |
| 15. | Festen HP, Lamers CB, Driessen WM, Van Tongeren JH. Cimetidine in anastomotic ulceration after partial gastrectomy. Gastroenterology. 1979;77:83-85. [PubMed] |
| 16. | Gugler R, Lindstaedt H, Miederer S, Möckel W, Rohner HG, Schmitz H, Székessy T. Cimetidine for anastomotic ulcers after partial gastrectomy. A randomized controlled trial. N Engl J Med. 1979;301:1077-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Koo J, Lam SK, Ong GB. Cimetidine versus surgery for recurrent ulcer after gastric surgery. Ann Surg. 1982;195:406-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Nwokolo CU, Smith JT, Gavey C, Sawyerr A, Pounder RE. Tolerance during 29 days of conventional dosing with cimetidine, nizatidine, famotidine or ranitidine. Aliment Pharmacol Ther. 1990;4 Suppl 1:29-45. [PubMed] |
| 19. | Martin IG, Diament RH, Dixon MF, Axon AT, Johnston D. Helicobacter pylori and recurrent ulceration after highly selective vagotomy. Eur J Gastroenterol Hepatol. 1995;7:207-209. [PubMed] |
| 20. | Cohen F, Valleur P, Serra J, Brisset D, Chiche L, Hautefeuille P. Relationship between gastric acid secretion and the rate of recurrent ulcer after parietal cell vagotomy. Ann Surg. 1993;217:253-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Feldman M, Richardson CT, Fordtran JS. Experience with sham feeding as a test for vagotomy. Gastroenterology. 1980;79:792-795. [PubMed] |