Published online Nov 28, 2006. doi: 10.3748/wjg.v12.i44.7210
Revised: August 28, 2006
Accepted: October 6, 2006
Published online: November 28, 2006
A 53-year-old male patient with a large hydatid cyst of the left hemidiaphragm and smaller secondary cysts located in the left thoracic cavity and upper left abdominal quadrant presented with two progressively enlarging lipoma-like masses in the left hypochondrium and under the left scapulae respectively. Total excision of all the cysts was performed through a bilateral subcostal incision, with the left hemidiaphragm near totally excised and replaced by a synthetic bilayer mesh.
- Citation: Marinis A, Fragulidis G, Karapanos K, Konstantinidis C, Brestas P, Vassiliou J, Smyrniotis V. Subcutaneous extension of a large diaphragmatic hydatid cyst. World J Gastroenterol 2006; 12(44): 7210-7212
- URL: https://www.wjgnet.com/1007-9327/full/v12/i44/7210.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i44.7210
Hydatid disease is a parasitosis, known as hydatidosis or echinococcosis caused by the larval stage of the Echinococcus granulosus tapeworm. The disease was first described by Hippocrates as “cysts full of water” in a man’s liver and by Aristotle in human lungs and liver[1]. The disease remains a considerable public health problem in endemic countries, including the Mediterranean and Middle East countries, New Zealand, Australia, South Africa and South American countries. The primary hosts are members of the Canidae family (dogs, wolves and coyotes); the intermediate hosts are sheep, cattle and deer[2]. Humans are accidental intermediates in the biologic cycle of taenia echinococcus granulosus, more frequently by direct contact with dogs than by ingestion of food or water contaminated with their feces[3]. The most commonly involved organs are the liver and lungs. Extrapulmonary intrathoracic location of a cyst involving the mediastinum, pleura, pericardium, chest wall and diaphragm is rare[4] and even rarer is the subcutaneous extension of echinococcus. Herein, we report a 53-year-old man with a primary large hydatid cyst of the diaphragm and smaller secondary hydatid cysts of the abdomen and thorax protruding subcutaneously.
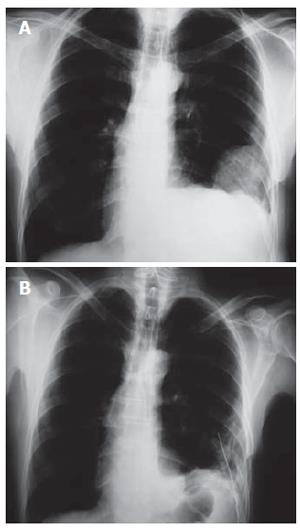
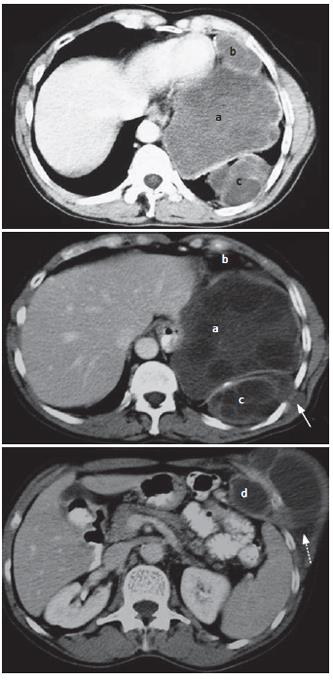
A 53-year-old farmer with a past medical history of two car accidents at 16 and 18 years of age, which resulted in a left hemothorax evacuated with a chest tube in the first one and a fracture of the left femur internally fixated in the second one, was admitted to our surgical department. The patient’s main complaint was the presence of a small soft lump in the left hypochondrium 15 years ago that was gradually increasing in size. A similar lump protruding under the left scapulae 1 mo before his admission presented without any symptoms indicating absence of compression of adjacent organs. Diminished breath sounds in the lower left hemithorax, the presence of a small (3-5 cm) subcutaneous lump between the posterior segments of the 7th and 8th ribs and a larger (13-15 cm) soft-tissue subcutaneous mass in the left hypochondrium were the clinical findings. Chest radiograph showed a left-sided opacity with scarce microcalcifications (Figure 1A). Pulmonary functional tests were normal. Thoraco-abdominal CT scan (Figure 2) revealed a hydatid cyst (14 cm in diameter) located in the left hemidiaphragm extending simultaneously to the thoracic cavity and the upper abdomen (cyst a), a cystic lesion (6 cm in diameter) in contact with the left side of the pericardium and the anterior surface of pleura anteriorly to the previous cyst (cyst b), a cystic lesion (9 cm in diameter) in the postero-lateral thoracic wall (cyst c) protruding intercostally to a small subcutaneous cyst under the scapulae (solid arrow) and an abdominal cystic lesion (13 cm in diameter, cyst d) protruding through the left costal cartilage to the left hypochondrium subcutaneously (broken arrow). CT scan showed a sand-glass appearance of the last two cysts. Laboratory tests were normal and serologic tests were positive for echinococcus granulosus (1/2048 antibodies, using enzyme-linked immunosorbent assay).
A bilateral subcostal incision was performed. Precau-tions were taken in order to avoid any spillage of cyst contents in the operation field including intact excision of all hydatid cysts and placement of sponges impregnated with hypertonic saline surrounding the involved organs. The subcutaneous hydatid cyst of the left hypochondrium was removed with its intra-abdominal portion and a partial resection of the left costal cartilage. The large hydatid cyst of the left hemidiaphragm embedded in the muscular layer was free of adhesions to the adjacent abdominal and thoracic organs. A total excision of this cyst with a nearly total excision of the left hemidiaphragm was performed. The hydatid cyst adjacent to the pericardium was completely removed. The hydatid cyst on the postero-lateral thoracic wall was removed with concomitant resection of the subscapular protrusion and the eroded posterior segment of the 9th rib. The left hemidiaphragm was replaced by a bilayer synthetic mesh (Bard Composix® Mesh 15.2 cm × 20.3 cm) and a chest tube was placed in the left thoracic cavity (Figure 1B). The patient was discharged on the 7th postoperative day and albendazole therapy was started at a dose of 400 mg bid. The postoperative course of our patient during the follow-up period (14 mo) was uneventful, with a good respiratory function.
Hydatid disease most frequently involves the liver (50%-70%) and lungs (20%-30%), which can be explained by a hypothesized novel dissemination theory via diaphragmatic lymphatic drainage proposed by Isitmangil et al[5]. However, other organs may be involved as well, such as the brain, heart, bone and muscle (10%)[6]. Subcutaneous location or extension of a hydatid cyst is even more rare[7-9]. This rare localization of echinococcosis presents as painless soft tissue tumors or lipomas and the patient usually does not seek surgical advice.
Total excision of hydatid cysts is the definitive therapy. A thorough preoperative study of the involved organs combining the findings of chest radiograph, ultrasonography, computed tomography and magnetic resonance imaging is necessary. The bilateral subcostal incision performed in this case has the advantage of a better approach to both the abdominal and thoracic lesions, without necessitating the use of standard thoracotomy which is preferred to treat intrathoracic extrapleural hydatid disease. However, repair or reconstruction of the diaphragm poses a technical challenge. If a synthetic mesh is used to close the defect, it must be properly applied and sutured under tension to avoid paradoxical movement and respiratory distress postoperatively. Moreover, septic complications related to mesh reconstruction during these procedures are rare and have not been reported in the literature.
S- Editor Wang GP L- Editor Wang XL E- Editor Lu W
| 1. | Sotiraki S, Himonas C, Korkoliakou P. Hydatidosis-echinococcosis in Greece. Acta Trop. 2003;85:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Eren S, Ulku R, Tanrikulu AC, Eren MN. Primary giant hydatid cyst of the diaphragm. Ann Thorac Cardiovasc Surg. 2004;10:118-119. [PubMed] |
| 3. | Ramos G, Orduña A, García-Yuste M. Hydatid cyst of the lung: diagnosis and treatment. World J Surg. 2001;25:46-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Ulkü R, Eren N, Cakir O, Balci A, Onat S. Extrapulmonary intrathoracic hydatid cysts. Can J Surg. 2004;47:95-98. [PubMed] |
| 5. | Isitmangil T, Toker A, Sebit S, Erdik O, Tunc H, Gorur R. A novel terminology and dissemination theory for a subgroup of intrathoracic extrapulmonary hydatid cysts. Med Hypotheses. 2003;61:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Savas L, Onlen Y, Akcali C, Aslan B, Pourbagher A, Tunc T, Ozkoc G. Hydatid disease with atypical localization: 4 cases report. Scand J Infect Dis. 2004;36:613-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | El Fortia M, Bendaoud M, Shaban A, Gharbi H, Ehtwaish F, Roberts D, Gatit A, Belaid A, Yhia A. Subcutaneous extension of a large psoas muscle Echinococcus cyst. Eur Radiol. 2000;10:870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Guiral J, Rodrigo A, Tello E. Subcutaneous echinococcosis of the knee. Lancet. 2004;363:38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Parmar H, Nagarajan G, Supe A. Subcutaneous rupture of hepatic hydatid cyst. Scand J Infect Dis. 2001;33:870-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |