Published online Nov 14, 2006. doi: 10.3748/wjg.v12.i42.6751
Revised: September 15, 2006
Accepted: September 21, 2006
Published online: November 14, 2006
In the past, Crohn’s disease (CD) has been understood primarily as an immunologic disorder characterized by an abnormal T-cell response. Recent in vitro and in vivo data suggests that CD may instead be precipitated by innate immune dysfunction resulting from a combination of genetic and environmental factors. Some reports have demonstrated a defective immune response in a variety of other cellular components, including neutrophils, monocytes and dendritic cells. Recent studies of granulocyte-macrophage colony-stimulating factor (GM-CSF) in CD, aiming to stimulate the innate immune system with the conception that an innate immune defect underlies the development of the disease, have been demonstrated a clinical benefit and reinforce this evolving understanding of the disease.
- Citation: Yamamoto-Furusho JK, Korzenik JR. Crohn’s disease: Innate immunodeficiency? World J Gastroenterol 2006; 12(42): 6751-6755
- URL: https://www.wjgnet.com/1007-9327/full/v12/i42/6751.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i42.6751
Over a period of many years Crohn’s Disease (CD) has been thought to result predominantly from excessive activation of type 1 helper T cells (TH1) with a characteristic cytokine profile including elevated interferon-γ and IL-2. However the pathways by which T cells became activated have remained an unsolved dilemma. Collectively recent studies using cell and animal models as well as studies of individuals with CD suggest that an aberrant innate immune response to luminal bacteria may be a critical initiating step in the development of the disease. These studies suggest that in at least some individuals with CD, innate immune responses are paradoxically impaired compared to normal controls.
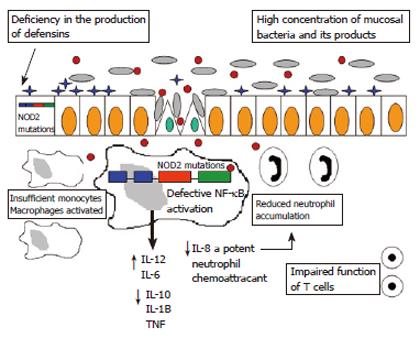
Improved, albeit still incomplete, understanding of the function of NOD2/CARD15 have been particularly key to an appreciation of the importance of innate immune dysfunction in CD. NOD2 is expressed constitutively in macrophages, neutrophils and dendritic cells[1], as well as in Paneth and epithelial cells[2]. NOD2 is a cytoplasmic protein that serves as a microbial sensor, and its leucine-rich repeat (LRR) domain is required for recognition of muramyl dipeptide (MDP), a fragment of peptidoglycan present in bacterial cell walls. The ligand MDP ultimately leads to activation of the transcription nuclear factor (NF-κB), and induction of proinflammatory cytokines[3,4]. Membrane recruitment of NOD2 is essential for NF-κB activation after the recognition of MDP in intestinal epithelial cells and is mediated by a motif comprising two leucine residues and a tryptophan in the COOH-terminal domain of NOD2[5]. Evidence that NOD2 may function as an antibacterial factor in intestinal epithelial cells was demonstrated in Caco-2 cells stably expressing wild type NOD2 when infected with Salmonella typhimurium. This protective effect was lost in cells expressing a most common mutant NOD2 associated with CD (3020insC)[6].
Specific mutations of the NOD2 gene have been definitively associated with increased susceptibility to ileal Crohn’s disease in Western (but not Asian) populations: Arg702Trp, Gly908Arg, and leu1007fsinsC (a frameshift mutation that truncates the carboxy terminal 33 aminoacids)[7,8]. Heterozygous carriage of the risk alleles confers a 2-4 fold increased risk, and homozygotes or compound heterozygotes have a 20-40 fold increased risk [9]. More than 90% of all CD associated mutations are located in the LRR domain, suggesting that these may affect the function of NOD2 with respect to bacterial recognition and signaling. Transient transfection experiments indicate that CD-associated NOD2 mutants no longer activate NF-κB in response to MDP[3,10], which suggests that defective NF-κB activation facilitates infection of the lamina propia by enteric bacteria.
Abbott DW et al[11] demonstrated that NOD2 activation leads to ubiquitinylation of NEMO, a key component of the NF-κB signaling complex. They showed that NOD2-dependent ubiquitinylation of NEMO is dependent on the scaffolding protein kinase RIP2. Crohn’s disease-associated mutants of NOD2 exhibited a decreased ability to bind RIP2, and this decreased ability to bind RIP2 correlates with a decreased ability to ubiquitinylate NEMO.
NOD2 mutants produce selective functional defects in leukocytes of patients with CD as shown by van Heel et al[12] who analyzed cytokine expression of peripheral blood mononuclear cells after exposure to MDP. In PBMC from CD patients the NOD2 ligand induced little TNFα and IL-1β, but strong IL-8 secretion. Futhermore, monocytes isolated from CD patients carrying the 1007fs (3020insC) mutation were reported to exhibit defects in the production of the proinflammatory cytokines, TNFα, IL-6 and IL-8, as well as the anti-inflammatory cytokine IL-10[13]. Dendritic cells derived from CD patients homozygous for leu1007fsinsC also fail to up-regulate the costimulatory molecules CD80 and CD86 in response to MDP and lack production of cytokines such as TNF-α, IL-12 and IL-10[14].
Intersection between TLR and NOD2 pathways is suggested by reports of synergistic induction of proinflammatory cytokines such as TNFα and IL-1β upon costimulation with MDP and specific TLR ligands[15,16]. MDP also substantially upregulated secretion of TNFα and IL-1β induced by ligands to five different TLR ligands, TLRs 2, 4, 5, 7 and 9: (Pam3CysSerLys4, LPS, Flagellin, MALP-2 and R-848, respectively). Of note, these effects were observed in the presence of the most common NOD2 mutants associated with CD. In studies using mice lacking NOD2, Watanabe et al[17] observed reduced responses to MDP, but enhanced responses to the TLR2 ligand, peptidoglycan e.g. increases in IL-12. They interpreted these findings to suggest that the NOD2 signaling pathways normally downregulate the TLR2 pathways. In their model, loss of function mutation of NOD2 together with TLR2 signals delivered by other bacterial products could result in enhanced cytokine responses to commensal bacteria by macrophages. These findings suggest that interaction between NOD2 and specific TLR pathways may represent an important modulatory mechanism of innate immune responses which is altered in some patients with CD.
However, controversy remains about the role of NOD2 and the interactions between NOD and TLR signaling pathways. While these results suggest that this NOD2 mutation may have enhanced responsiveness to bacterial peptidoglycan, interpretation of the significance of these findings remains controversial, because transient transfection assays using the CD-associated NOD2 mutants, as described above, have consistently shown defective cytokine responses to MDP and decreased activation of NF-κB[18]. In contrast to Watanabe et al Kobayashi and colleagues[19] did not find upregulation of TLR responses following disruption of NOD2. Kobayashi et al did find that mutations in NOD2 in mice affect the expression of small antibacterial proteins called cryptidins (α-defensins in humans) by intestinal epithelial cells. This data is consistent with the notion that NOD2 regulates the production of antibacterial peptides in Paneth cells in the intestinal crypts, and that this may contribute to local control of pathogenic bacteria (Figure 1).
In general, α-defensins (1-3, 5 and 6) are induced in the colonic mucosa of CD and UC patients. However, NOD2 mutations in CD patients are associated with diminished mucosal α-defensin expression[20]. Decreased β-defensin 1 and the lack of induction of both inducible antimicrobial peptides β-defensins 2 and 3 in CD could result in enhanced bacterial survival and perhaps invasion[21].
Neutrophils act as a first line defense at the mucosal-microbial interface by killing and digesting bacteria within phagocytic vacuoles. Neutrophil-mediated clearance of mucosal microbes would prevent activation and recruitment of monocytes/macrophages. Several defects have been described in patients with CD, including impairment in migration of neutrophils[22]; complement dysfunction that produces impaired neutrophil recruitment[23]; decrease of phagocytic and bactericidal neutrophil function[24] and deficient superoxide generation in neutrophils[25].
A number of genetic syndromes with well described defects of the innate immune system may also provide insights into pathophysiology relevant to CD. Patients with glycogen storage disease (GSD) Ib[26,27], chronic granulomatous disease (CGD)[28], Chediak Higashi syndrome[29], Hermansky-Pudlak syndrome[30] leukocyte adhesion deficiency[31], Turner’s syndrome[32], and congenital[33], cyclic[34] and autoimmune[35] neutropenias can all manifest features of CD or CD-like phenotype[36]. Each of these syndromes comprises a quantitative or qualitative deficiency in the function of neutrophils, monocytes, or macrophages, suggesting that varied functional cellular deficiencies can result in a common intestinal phenotype of CD.
The finding that two murine lines with disruption of either CCAAT/enhancer binding protein (CEBP)-ε[37] and a cell-type specific disruption of the Stat3 gene in neutrophils and macrophages[38] develops enterocolitis, support the role of the neutrophil and the macrophage in the development of CD. Stat-3 disrupted mice show an immune response skewed toward Th-1 activity, demonstrating that neutrophil and macrophage dysfunction may eventuate in a Th-1 phenotype.
Thus a variety of studies and clinical insights have suggested that CD may result from an impaired mucosal innate immune response. In the context of these earlier findings, a recent study by Marks et al[39] support the hypothesis that the mucosal innate immune system plays a central role early in the development of CD. Marks et al[39] found a significantly decreased production of IL-8 and IL-1β (45% and 50% reduction respectively) from macrophages of patients with CD. This defect in the production of these cytokines was independent of the presence of NOD2 mutations and helps to clarify the controversy generated by Li et al[40] who reported that the presence of NOD2 mutations showed no induction (Leu1007finsC) or modest induction (Gly908Arg and Arg702Trp) of IL-8 and IL-1β). Macrophages from CD patients produce less IL-8 in response to pro-inflammatory agonists, suggesting that these cells may influence the acute inflammatory response. Impaired secretion of IL-8 appears to result in a failure of neutrophil migration. This finding was confirmed by normalizing neutrophil efflux after augmentation of endogenous IL-8 secretion by topical MDP. The authors suggest that in CD, reduced or delayed recruitment of neutrophils to sites where bacteria penetrate the intestinal wall may result in the persistence of bacteria and other debris in the tissue and lead to the chronic inflammation typical of this disease.
The data of Marks et al[39] suggests that CD patients possess a generalized impaired innate immune response as reflected by diminished response to intradermal injection of killed bacteria as well as trauma of the skin or the intestine. When killed bacteria were injected into the forearms of CD patients, there was less blood flow to the injection site than non-CD patients. They also found that CD patients had reduced neutrophil accumulation and interleukin-8 (IL-8) production at sites of tissue trauma in the intestine and skin. This study supports the idea that CD may in some way be associated with relative inability to mount an acute inflammatory response compared to normal individuals.
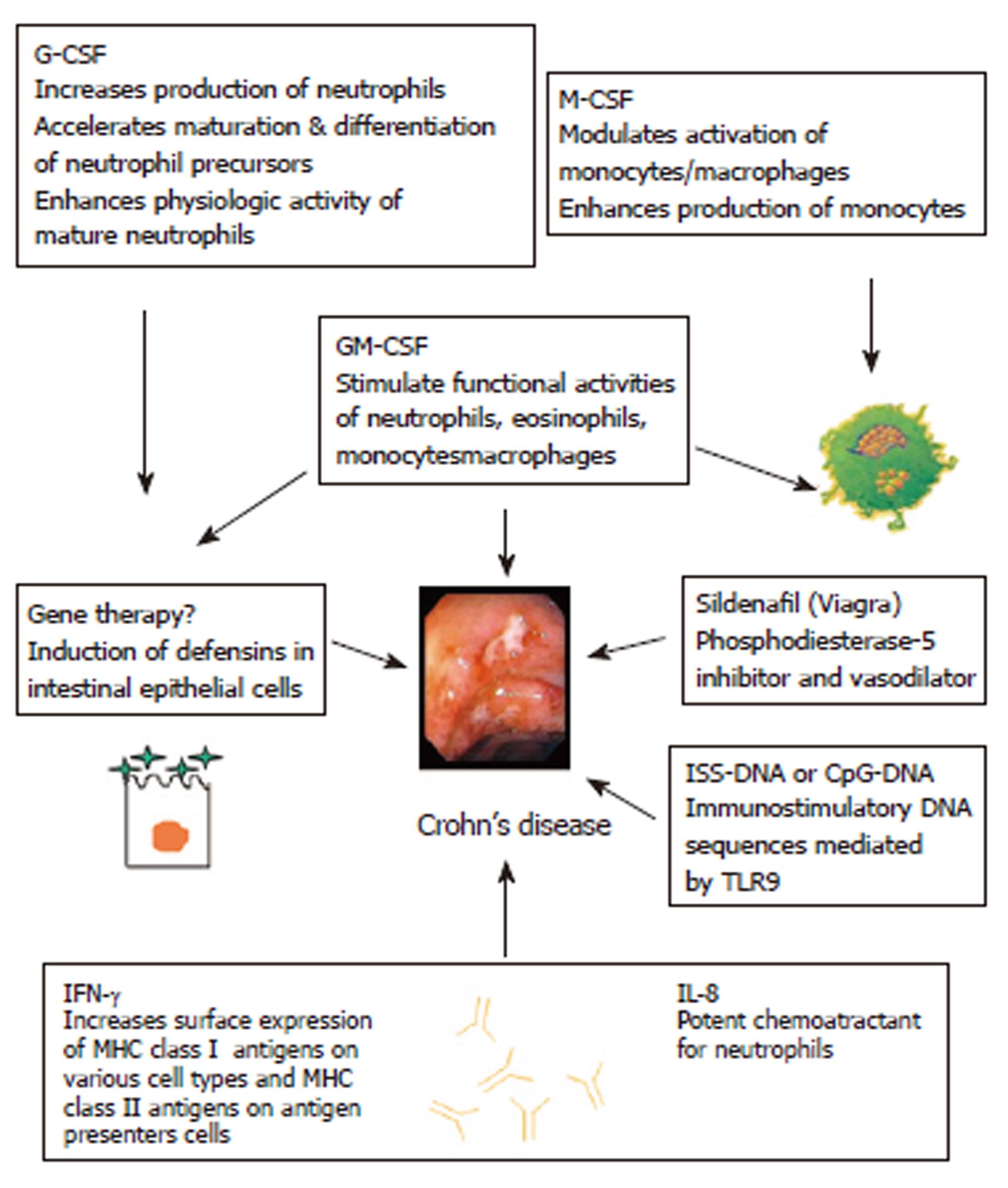
Marks et al[39] suggest the provocative notion that IL-8 either by direct enteral administration or through synthesis by genetically modified gut organisms might have therapeutic value. Similarly, they propose that if diminished recruitment of neutrophils is a backdrop to CD, agents that increase blood flow such as long-acting phosphodiesterase-5 inhibitors might be useful in healing or preventing lesions in CD. In support of this possibility, they report that oral administration of sildenafil markedly increased blood flow to sites of bacterial injection in CD patients.
Recent reports suggest that agents which act to enhance innate immune defenses can indeed confer therapeutic benefit. The endogenous growth factor granulocyte-macrophage colony-stimulating factor (GM-CSF) performs important functions in both the phagocytic and epithelial components of intestinal early innate immune defense. GM-CSF is expressed by both CD4+ T cells and Paneth cells in the intestine, and its receptors have been recently demonstrated to be present on intestinal epithelial cells which proliferate in response to GM-CSF in vitro[41,42]. Within the immune system, GM-CSF increases phagocytic cell function through its effects on oxidative burst, phagocytosis, and intracellular bacterial killing[43].
In the context of the evolving concepts of CD pathophysiology, these observations provided the rationale for clinical trials of granulocyte colony stimulating factor (G-CSF, specifically filgrastim) and GM-CSF (sargramostim). Both pilot studies suggested a benefit[44,45], though GM-CSF appeared more effective. A recent randomized controlled trial of 124 patients found a significant benefit in response at 100-point decrease in CDAI and in remission. The response was sustained for a mean of 8-10 wk after discontinuation of therapy[46]. While mechanistic studies were not included in the trial, recent translational studies[47] have demonstrated that GM-CSF can reverse several neutrophil impairments in cells obtained from individuals with CD (Figure 2).
In summary, mucosal innate immunodeficiency characterized by impaired dysfunction of neutrophils, monocytes and dendritic cells as well as intestinal epithelium play a critical early role in the development of CD. These defects may arise from a variety of genetic defects which are presumably worsened by environmental factors to culminate in decreased cytokine production and insufficient bacterial killing. Persistence of microbial derived stimuli subsequently leads to T cell activation, accounting for the T cell driven nature of the established disease. This concept would provide insight into why immunosuppression may be effective in some individuals by limiting the secondary, chronic T-cell response, while immune stimulation, possibly with GM-CSF, may also prove to be effective as a general strategy particularly in acute and early phases of the disease. A better understanding of the early initiating events in CD may result in even better therapeutic approaches that enhance the innate immune system.
We thank Daniel K Podolsky MD for his support and helpful comments to this manuscript.
S- Editor Wang J L- Editor Alpini GD E- Editor Ma WH
| 1. | Ogura Y, Inohara N, Benito A, Chen FF, Yamaoka S, Nunez G. Nod2, a Nod1/Apaf-1 family member that is restricted to monocytes and activates NF-kappaB. J Biol Chem. 2001;276:4812-4818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1034] [Cited by in RCA: 1041] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 2. | Ogura Y, Lala S, Xin W, Smith E, Dowds TA, Chen FF, Zimmermann E, Tretiakova M, Cho JH, Hart J. Expression of NOD2 in Paneth cells: a possible link to Crohn's ileitis. Gut. 2003;52:1591-1597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 326] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 3. | Inohara N, Ogura Y, Fontalba A, Gutierrez O, Pons F, Crespo J, Fukase K, Inamura S, Kusumoto S, Hashimoto M. Host recognition of bacterial muramyl dipeptide mediated through NOD2. Implications for Crohn's disease. J Biol Chem. 2003;278:5509-5512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1255] [Cited by in RCA: 1252] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 4. | Girardin SE, Boneca IG, Viala J, Chamaillard M, Labigne A, Thomas G, Philpott DJ, Sansonetti PJ. Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem. 2003;278:8869-8872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1755] [Cited by in RCA: 1772] [Article Influence: 80.5] [Reference Citation Analysis (0)] |
| 5. | Barnich N, Aguirre JE, Reinecker HC, Xavier R, Podolsky DK. Membrane recruitment of NOD2 in intestinal epithelial cells is essential for nuclear factor-{kappa}B activation in muramyl dipeptide recognition. J Cell Biol. 2005;170:21-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 237] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 6. | Hisamatsu T, Suzuki M, Reinecker HC, Nadeau WJ, McCormick BA, Podolsky DK. CARD15/NOD2 functions as an antibacterial factor in human intestinal epithelial cells. Gastroenterology. 2003;124:993-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 429] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 7. | Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, Britton H, Moran T, Karaliuskas R, Duerr RH. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001;411:603-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3555] [Cited by in RCA: 3478] [Article Influence: 144.9] [Reference Citation Analysis (1)] |
| 8. | Hugot JP, Chamaillard M, Zouali H, Lesage S, Cézard JP, Belaiche J, Almer S, Tysk C, O'Morain CA, Gassull M. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature. 2001;411:599-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4223] [Cited by in RCA: 3905] [Article Influence: 162.7] [Reference Citation Analysis (0)] |
| 9. | Cuthbert AP, Fisher SA, Mirza MM, King K, Hampe J, Croucher PJ, Mascheretti S, Sanderson J, Forbes A, Mansfield J. The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease. Gastroenterology. 2002;122:867-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 469] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 10. | Girardin SE, Travassos LH, Hervé M, Blanot D, Boneca IG, Philpott DJ, Sansonetti PJ, Mengin-Lecreulx D. Peptidoglycan molecular requirements allowing detection by Nod1 and Nod2. J Biol Chem. 2003;278:41702-41708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 489] [Cited by in RCA: 520] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 11. | Abbott DW, Wilkins A, Asara JM, Cantley LC. The Crohn's disease protein, NOD2, requires RIP2 in order to induce ubiquitinylation of a novel site on NEMO. Curr Biol. 2004;14:2217-2227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 291] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 12. | van Heel DA, Ghosh S, Butler M, Hunt KA, Lundberg AM, Ahmad T, McGovern DP, Onnie C, Negoro K, Goldthorpe S. Muramyl dipeptide and toll-like receptor sensitivity in NOD2-associated Crohn's disease. Lancet. 2005;365:1794-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 242] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 13. | Netea MG, Ferwerda G, de Jong DJ, Jansen T, Jacobs L, Kramer M, Naber TH, Drenth JP, Girardin SE, Kullberg BJ. Nucleotide-binding oligomerization domain-2 modulates specific TLR pathways for the induction of cytokine release. J Immunol. 2005;174:6518-6523. [PubMed] |
| 14. | Kramer M, Netea MG, de Jong DJ, Kullberg BJ, Adema GJ. Impaired dendritic cell function in Crohn's disease patients with NOD2 3020insC mutation. J Leukoc Biol. 2006;79:860-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Strober W, Murray PJ, Kitani A, Watanabe T. Signalling pathways and molecular interactions of NOD1 and NOD2. Nat Rev Immunol. 2006;6:9-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 601] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 16. | Netea MG, Kullberg BJ, de Jong DJ, Franke B, Sprong T, Naber TH, Drenth JP, Van der Meer JW. NOD2 mediates anti-inflammatory signals induced by TLR2 ligands: implications for Crohn's disease. Eur J Immunol. 2004;34:2052-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 164] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 17. | Watanabe T, Kitani A, Murray PJ, Strober W. NOD2 is a negative regulator of Toll-like receptor 2-mediated T helper type 1 responses. Nat Immunol. 2004;5:800-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 615] [Cited by in RCA: 603] [Article Influence: 28.7] [Reference Citation Analysis (0)] |
| 18. | Maeda S, Hsu LC, Liu H, Bankston LA, Iimura M, Kagnoff MF, Eckmann L, Karin M. Nod2 mutation in Crohn's disease potentiates NF-kappaB activity and IL-1beta processing. Science. 2005;307:734-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 583] [Cited by in RCA: 584] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 19. | Kobayashi KS, Chamaillard M, Ogura Y, Henegariu O, Inohara N, Nuñez G, Flavell RA. Nod2-dependent regulation of innate and adaptive immunity in the intestinal tract. Science. 2005;307:731-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1334] [Cited by in RCA: 1327] [Article Influence: 66.4] [Reference Citation Analysis (2)] |
| 20. | Wehkamp J, Harder J, Weichenthal M, Schwab M, Schäffeler E, Schlee M, Herrlinger KR, Stallmach A, Noack F, Fritz P. NOD2 (CARD15) mutations in Crohn's disease are associated with diminished mucosal alpha-defensin expression. Gut. 2004;53:1658-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 592] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 21. | Fellermann K, Wehkamp J, Herrlinger KR, Stange EF. Crohn's disease: a defensin deficiency syndrome. Eur J Gastroenterol Hepatol. 2003;15:627-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Segal AW, Loewi G. Neutrophil dysfunction in Crohn's disease. Lancet. 1976;2:219-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 131] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Elmgreen J. Complement and function of neutrophils in chronic inflammatory bowel disease. Dan Med Bull. 1986;33:222-228. [PubMed] |
| 24. | Wandall JH. Function of exudative neutrophilic granulocytes in patients with Crohn's disease or ulcerative colitis. Scand J Gastroenterol. 1985;20:1151-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Curran FT, Allan RN, Keighley MR. Superoxide production by Crohn's disease neutrophils. Gut. 1991;32:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Roe TF, Thomas DW, Gilsanz V, Isaacs H Jr, Atkinson JB. Inflammatory bowel disease in glycogen storage disease type Ib. J Pediatr. 1986;109:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Sanderson IR, Bisset WM, Milla PJ, Leonard JV. Chronic inflammatory bowel disease in glycogen storage disease type 1B. J Inherit Metab Dis. 1991;14:771-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Werlin SL, Chusid MJ, Caya J, Oechler HW. Colitis in chronic granulomatous disease. Gastroenterology. 1982;82:328-331. [PubMed] |
| 29. | Ishii E, Matui T, Iida M, Inamitu T, Ueda K. Chediak-Higashi syndrome with intestinal complication. Report of a case. J Clin Gastroenterol. 1987;9:556-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Grucela AL, Patel P, Goldstein E, Palmon R, Sachar DB, Steinhagen RM. Granulomatous enterocolitis associated with Hermansky-Pudlak syndrome. Am J Gastroenterol. 2006;101:2090-2095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | D'Agata ID, Paradis K, Chad Z, Bonny Y, Seidman E. Leucocyte adhesion deficiency presenting as a chronic ileocolitis. Gut. 1996;39:605-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 55] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Knudtzon J, Svane S. Turner's syndrome associated with chronic inflammatory bowel disease. A case report and review of the literature. Acta Med Scand. 1988;223:375-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Vannier JP, Arnaud-Battandier F, Ricour C, Schmitz J, Buriot D, Griscelli C, Rey J. [Chronic neutropenia and Crohn's disease in childhood. Report of 2 cases ]. Arch Fr Pediatr. 1982;39:367-370. [PubMed] |
| 34. | Lamport RD, Katz S, Eskreis D. Crohn's disease associated with cyclic neutropenia. Am J Gastroenterol. 1992;87:1638-1642. [PubMed] |
| 35. | Stevens C, Peppercorn MA, Grand RJ. Crohn's disease associated with autoimmune neutropenia. J Clin Gastroenterol. 1991;13:328-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Korzenik JR, Dieckgraefe BK. Is Crohn's disease an immunodeficiency A hypothesis suggesting possible early events in the pathogenesis of Crohn's disease. Dig Dis Sci. 2000;45:1121-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 37. | Yamanaka R, Barlow C, Lekstrom-Himes J, Castilla LH, Liu PP, Eckhaus M, Decker T, Wynshaw-Boris A, Xanthopoulos KG. Impaired granulopoiesis, myelodysplasia, and early lethality in CCAAT/enhancer binding protein epsilon-deficient mice. Proc Natl Acad Sci USA. 1997;94:13187-13192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 302] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 38. | Takeda K, Clausen BE, Kaisho T, Tsujimura T, Terada N, Förster I, Akira S. Enhanced Th1 activity and development of chronic enterocolitis in mice devoid of Stat3 in macrophages and neutrophils. Immunity. 1999;10:39-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 943] [Cited by in RCA: 942] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 39. | Marks DJ, Harbord MW, MacAllister R, Rahman FZ, Young J, Al-Lazikani B, Lees W, Novelli M, Bloom S, Segal AW. Defective acute inflammation in Crohn's disease: a clinical investigation. Lancet. 2006;367:668-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 287] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 40. | Li J, Moran T, Swanson E, Julian C, Harris J, Bonen DK, Hedl M, Nicolae DL, Abraham C, Cho JH. Regulation of IL-8 and IL-1beta expression in Crohn's disease associated NOD2/CARD15 mutations. Hum Mol Genet. 2004;13:1715-1725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 218] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 41. | Fukuzawa H, Sawada M, Kayahara T, Morita-Fujisawa Y, Suzuki K, Seno H, Takaishi S, Chiba T. Identification of GM-CSF in Paneth cells using single-cell RT-PCR. Biochem Biophys Res Commun. 2003;312:897-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Ramsay RG, Micallef SJ, Williams B, Lightowler S, Vincan E, Heath JK, Mantamadiotis T, Bertoncello I. Colony-stimulating factor-1 promotes clonogenic growth of normal murine colonic crypt epithelial cells in vitro. J Interferon Cytokine Res. 2004;24:416-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Armitage JO. Emerging applications of recombinant human granulocyte-macrophage colony-stimulating factor. Blood. 1998;92:4491-4508. [PubMed] |
| 44. | Dieckgraefe BK, Korzenik JR. Treatment of active Crohn's disease with recombinant human granulocyte-macrophage colony-stimulating factor. Lancet. 2002;360:1478-1480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 131] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 45. | Korzenik JR, Dieckgraefe BK. An open-labelled study of granulocyte colony-stimulating factor in the treatment of active Crohn's disease. Aliment Pharmacol Ther. 2005;21:391-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 46. | Korzenik JR, Dieckgraefe BK, Valentine JF, Hausman DF, Gilbert MJ. Sargramostim for active Crohn's disease. N Engl J Med. 2005;352:2193-2201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 247] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 47. | Biagioni C, Favilli F, Catarzi S, Marcucci T, Fazi M, Tonelli F, Vincenzini MT, Iantomasi T. Redox state and O2*- production in neutrophils of Crohn's disease patients. Exp Biol Med (Maywood). 2006;231:186-195. [PubMed] |