Published online Oct 28, 2006. doi: 10.3748/wjg.v12.i40.6561
Revised: July 2, 2006
Accepted: August 21, 2006
Published online: October 28, 2006
A 49-year-old, previously healthy woman sought treatment for abdominal pain. Colonoscopy revealed ascending colon cancer. Computed tomography and angiography showed splenic metastasis and thrombosis extending from the splenic vein to the portal vein. She underwent right hemicolectomy, splenectomy, and distal pancreatomy. Histological findings showed no malignant cell in the splenic vein which was filled with organizing thrombus. We postulate the mechanism of splenic vein thrombosis in our case to be secondary to the extrinsic compression of the splenic vein by the splenic metastasis or by the inflammatory process produced by the splenic metastasis. In conclusion, we suggest that splenic metastasis should be added to the list of differential diagnosis which causes splenic vein thrombosis. In the absence of other sites of neoplastic disease, splenectomy seems to be the preferred therapy because it can be performed with low morbidity and harbors the potential for long-term survival.
- Citation: Hiraiwa K, Morozumi K, Miyazaki H, Sotome K, Furukawa A, Nakamaru M, Tanaka Y, Iri H. Isolated splenic vein thrombosis secondary to splenic metastasis: A case report. World J Gastroenterol 2006; 12(40): 6561-6563
- URL: https://www.wjgnet.com/1007-9327/full/v12/i40/6561.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i40.6561
Isolated splenic vein thrombosis is a rare clinical syndrome that may lead to left-sided portal hypertension. Metastasis to the spleen from solid tumors is also considered rare. When identified it usually occurs in the setting of widely disseminated diseases. We report a case of isolated splenic vein thrombosis secondary to splenic metastasis of an adenocarcinoma of the colon. The splenic lesion was detected before the resection of the primary colon lesion during a complete metastatic work-up.
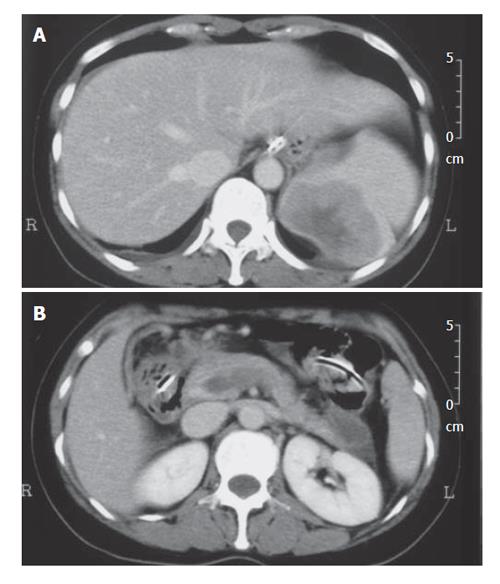
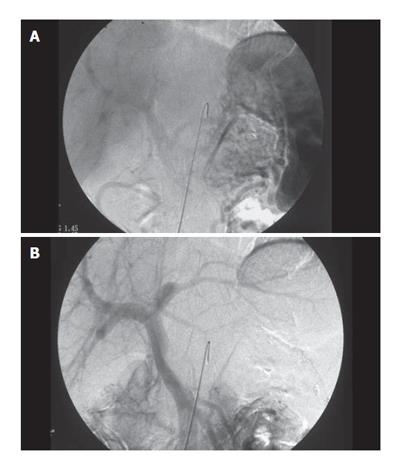
A 49-year-old woman presented complaining of abdo-minal pain in May 2003. There was no relevant medical history. Her performance status was not impaired. Physical examination revealed upper abdominal tenderness with mild guarding. Laboratory findings revealed anemia with hemoglobin of 84 g/L and hematocrit of 29.9%. Esophagogastroduodenoscopy revealed no remarkable finding. Colonoscopy revealed ascending colon cancer of 7 cm in diameter. The level of tumor markers was elevated with carcinoembryonic antigen of 36.7 μg/L and CA19-9 of 1870 kU/L. Computed tomography of the abdomen showed splenic metastasis (Figure 1A), but no metastasis in the liver. Contrast-enhanced computed tomography and angiography showed occlusion of the splenic vein, a shadow defect at the portal vein, and development of collaterals, which suggested tumor thrombosis extending from the splenic vein to the portal vein (Figures 1B, 2A, B).
We diagnosed her as having an ascending colon cancer with splenic metastasis and splenic vein tumor thrombosis (T3NXM1, Stage IV). She underwent right hemicolectomy, splenectomy, and distal pancreatomy. The tumor of the spleen was adherent to the left hemidiaphragm, so a small segment of the diaphragm was removed en bloc. The portal vein was resected at its junction with the splenic vein and reanastomosed.
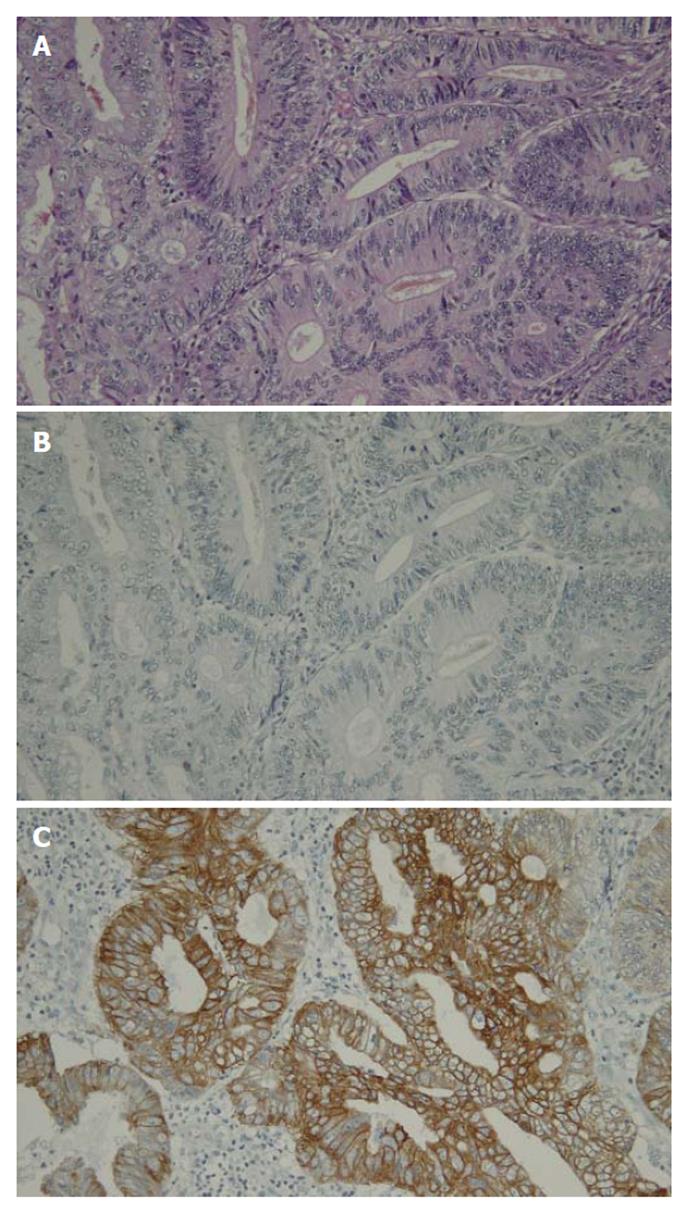
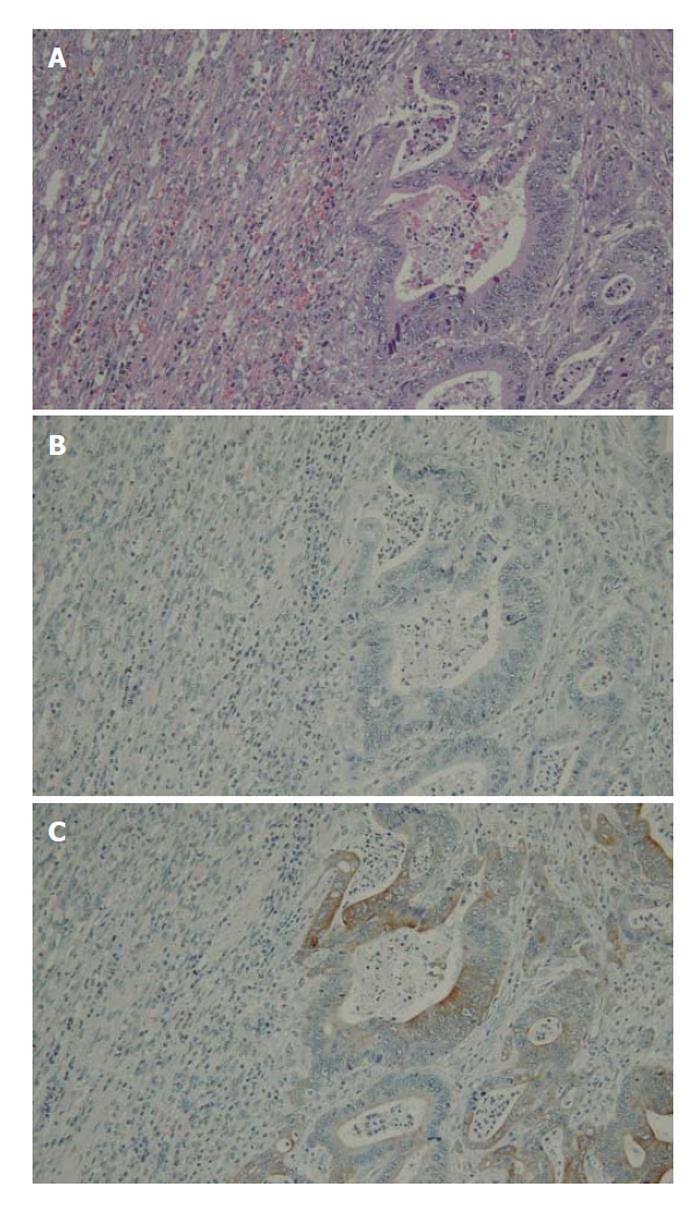
Histological findings showed a moderately diffe-rentiated adenocarcinoma of the ascending colon (Figure 3A) that invaded into serosa, with one of the five lymph nodes being positive for metastatic adenocarcinoma. The tumor of the spleen consisted of a moderately differentiated adenocarcinoma similar in histology to the tumor of the ascending colon (Figure 4A). These sections were stained with immunohistochemical reactions of antibodies to cytokeratins 7 and 20 (Figures 3B, C, 4B, C). Negative staining for cytokeratin 7 and positive staining for cytokeratin 20 was consistent with splenic metastasis of an adenocarcinoma of the colon[1].
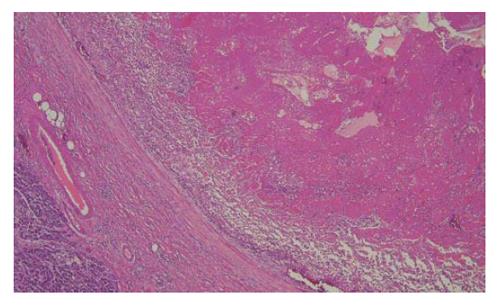
On the contrary to the preoperative diagnosis, no malignant cell was recognized in the splenic vein which was filled with organizing thrombus (Figure 5).
The postoperative course was uneventful. Two years and three months later, the patient is alive and well except for a nodule in the Douglas fossa which seems to be metastasis.
Isolated splenic vein thrombosis is a rare clinical syndrome that causes left-sided portal hypertension. It may lead to bleeding from gastric varices. The majority of splenic vein thrombosis are the result of pancreatic pathologies, including acute and chronic pancreatitis, pancreatic pseudocyst, pancreatic tumor and abscesses[2]. Other reported causes are traumas, umbilical vein catheterizations, lymphomas and sarcomas, retroperitoneal fibrosis, gastric surgeries, splenic artery aneurysms, myeloproliferative diseases, hereditary thrombocythemia[3], renal diseases including renal cell carcinomas[4] and benign renal cysts[5], and tuberculous lymphadenitis[6]. Our case did not have these diseases, and so we postulate the mechanism of splenic vein thrombosis in our case to be secondary to the extrinsic compression of the splenic vein by the splenic metastasis or by the inflammatory process produced by the splenic metastasis. To our knowledge, there has been no report of isolated splenic vein thrombosis secondary to splenic metastasis.
Carcinoma of the colon frequently metastasizes to the liver but only occasionally involves the spleen. The spleen is considered an unfavourable site for the development of metastases but the reason for this is not fully understood. Metastatic carcinoma that involves the spleen is usually a manifestation of widely disseminated disease involving multiple organs. Berge conducted an autopsy study on 7246 patients with various types of malignant tumors[7]. Splenic metastases were found in 21 out of the 1019 (2%) patients with colorectal carcinoma, but all were associated with involvement of other organs as well.
There are no long-term follow-up data of splenectomy for metastasis from colon cancer. Our patient underwent splenectomy, as it would deem to provide the only chance for long-term survival.
In conclusion, we suggest that metastatic tumor of the spleen should be added to the list of differential diagnosis which causes splenic vein thrombosis. Splenic metastasis from adenocarcinoma of the colon is a rare finding. In the absence of other sites of neoplastic disease, splenectomy seems to be the preferred therapy because it can be performed with low morbidity and harbors the potential for long-term survival.
S- Editor Wang GP L- Editor Ma JY E- Editor Ma WH
| 1. | Tot T. Cytokeratins 20 and 7 as biomarkers: usefulness in discriminating primary from metastatic adenocarcinoma. Eur J Cancer. 2002;38:758-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 183] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 2. | Smith TA, Brand EJ. Pancreatic cancer presenting as bleeding gastric varices. J Clin Gastroenterol. 2001;32:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Glynn MJ. Isolated splenic vein thrombosis. Arch Surg. 1986;121:723-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Hasan A, Ahmed M. Isolated splenic vein occlusion: a report of two cases. J Pak Med Assoc. 1982;32:79-80. [PubMed] |
| 5. | Koehler RE. Case: splenic vein obstruction due to metastatic hypernephroma. Gastrointest Radiol. 1981;6:365-370. [PubMed] |
| 6. | Takeuchi H, Suzuki M, Unno M, Kakita T, Matsuno S, Nakura H. Splenic vein occlusion secondary to tuberculous lymphadenitis at the splenic hilum: report of a case. Surg Today. 2000;30:383-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Berge T. Splenic metastases. Frequencies and patterns. Acta Pathol Microbiol Scand. 1974;82:499-506. [PubMed] |