Published online Oct 28, 2006. doi: 10.3748/wjg.v12.i40.6559
Revised: August 12, 2006
Accepted: September 11, 2006
Published online: October 28, 2006
Gallbladder tuberculosis (GT) is an extremely rare disease, and very few cases have been reported in the literature. The first case of GT was described in 1870 by Gaucher. A correct preoperative diagnosis of GT is unusual, and it is frequently confused with various gallbladder diseases. We present a new case of a patient who underwent surgery with the preoperative diagnosis of gallbladder cancer after a false positive positron emission tomography scan in the diagnostic work-up.
- Citation: Ramia J, Muffak K, Fernández A, Villar J, Garrote D, Ferron J. Gallbladder tuberculosis: False-positive PET diagnosis of gallbladder cancer. World J Gastroenterol 2006; 12(40): 6559-6560
- URL: https://www.wjgnet.com/1007-9327/full/v12/i40/6559.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i40.6559
Abdominal tuberculosis is common in developing countries but gallbladder tuberculosis (GT) is an extremely rare disease[1,2], and very few cases have been reported in the literature[1]. The first case of GT was described in 1870 by Gaucher.
A correct preoperative diagnosis of GT is unusual, and it is frequently confused with various gallbladder diseases. We present a new case of a patient who underwent surgery with the preoperative diagnosis of gallbladder cancer after a false positive positron emission tomography (PET) scan in the diagnostic work-up.
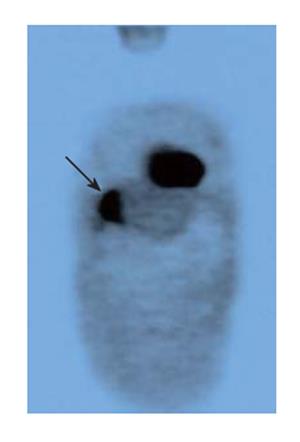
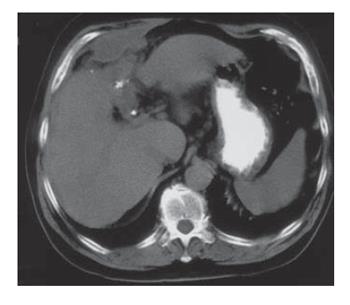
A 64-year-old man was admitted to our department for abdominal pain and jaundice. Abdominal examination revealed a palpable mass in right hypochondrium. Laboratory tests were normal. A gallbladder mass was observed on ultrasound. A computed tomography (CT) scan showed a thickened gallbladder wall with possible infiltration of liver parenchyma and duodenum, and we proposed a diagnosis of advanced neoplasm of gallbladder (Figure 1). A PET scan showed a hypermetabolic area in the right liver lobe in the usual location of the gallbladder, infiltrating the liver parenchyma (Figure 2) and reaffirming our suspected diagnosis of advanced neoplasm of gallbladder.
We performed a subcostal laparotomy and observed a very large tumor that involved gallbladder and duodenum. A biopsy of the gallbladder wall was taken, and the histologic perioperative study reported gallbladder tuberculosis with no signs of malignancy. We then performed a cholecystectomy and observed the presence of cholecistoduodenal fistulae, so that we closed the duodenum. An exhaustive examination of the abdominal cavity revealed no other foci of tubercular infection. The definitive histologic study showed granulomatous reaction with the presence of multinucleated giant cells and caseum necrosis compatible with GT.
The postoperative course was uneventful. A Mantoux test was positive. Other techniques (chest X-ray, bronchoscopy) showed no tubercular infection in other organs. Antitubercular drugs were prescribed for six months.
The gallbladder is highly resistant to tubercular infection, and the presence of cholelitiasis and cystic duct obstruction is essential for the development of GT[1,2]. About 70% of GT cases are accompanied by gallstones[2]. Four types of GT have been described, according to whether only the gallbladder is involved or there is generalized tuberculosis and whether the gallbladder mucosa is histologically involved[1]. GT often occurs together with other intra-abdominal tuberculoses, usually in women over 30 years of age[2]. However, in the present case it was restricted to the gallbladder, because the duodenum was only locally involved. The route of infection may be peritoneal, hematogenous or lymphatic[2]. Histologically, the lesion may be in the form of a localized ulceration or there may be typical tuberculosis nodules in the wall of varied size and numbers.
A wide spectrum of symptoms have been described in patients with GT, including abdominal pain in right hypochondrium, weight loss, fever, anorexia, diarrhea, nausea, vomiting and a palpable abdominal mass[2]. Anemia, elevated ESR and positive tuberculin test are usually found in laboratory examinations.
The correct diagnosis of GT is difficult, and it is usually made after a cholecystectomy[1]. Ultrasound and CT may show an enlarged gallbladder, a thickened gallbladder wall, soft tissue masses, or nodular lesions, although neither ultrasound nor CT lesions are specific[2]. The diagnosis of tuberculosis in other abdominal organs (liver, spleen, lymph nodes or peritoneum) is very helpful for diagnosing GT.
The differential diagnosis of GT includes acute and chronic cholecystitis, polypoid lesions and gallbladder carcinoma[2]. The presence of a mass that fills the gallbladder associated with cholelitiasis is indistinguishable from carcinoma of the gallbladder[1]. Moreover, both GT and carcinoma can give rise to regional lymph nodes. The presence of liver metastasis or liver infiltration suggests the presence of a gallbladder carcinoma. On the other hand, lung lesions or mesenteric thickening is frequent in patients with tubercular infection.
PET is a very accurate diagnostic method for cancer. PET can image the metabolic differences between normal and malignant cells using tumor-seeking tracers[3]. According to some authors, it is difficult to distinguish patients with lung cancer from those with pulmonary tuberculosis due to the high uptake rate of patients with active tuberculosis[3,4]. This is because an increased glycolysis of macrophages, cells present in tubercular infection, results in a high FDG uptake value[3]. 11C-choline tracer is more accurate than 18F-fluorodeoxyglucose for making the differential diagnosis between tubercular infection and cancer[3].
There has been little experience with PET as a diagnostic tool in gallbladder cancer but the first published reports are fairly encouraging, showing a sensitivity of 75%[5,6]. At our department, a prospective trial is in progress to establish the sensitivity of PET scan in patients with suspicion of gallbladder cancer based on CT scan. The present patient was included in this trial and the results obtained appeared to confirm the suspected diagnosis of gallbladder cancer. To our knowledge, this is the first case of a false positive PET scan in a gallbladder cancer due to GT. There is one previous report of pancreatic tuberculosis that was misdiagnosed as pancreatic cancer after a positive PET scan[7].
Tuberculosis was common in Spain in the past but is now an uncommon finding in immunocompetent patients, and the GT diagnosis was therefore unexpected. In the countries with a high rate of tuberculosis infection, the possibility of a tuberculosis infection should be considered in patients suspected of a hepatobiliary cancer (liver, pancreas or gallbladder) with a positive PET if the patient has a positive Mantoux test or a history of tuberculosis.
S- Editor Wang GP L- Editor Ma JY E- Editor Ma WH
| 1. | Jain R, Sawhney S, Bhargava D, Berry M. Gallbladder tuberculosis: sonographic appearance. J Clin Ultrasound. 1995;23:327-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Yu R, Liu Y. Gallbladder tuberculosis: case report. Chin Med J (Engl). 2002;115:1259-1261. [PubMed] |
| 3. | Hara T, Kosaka N, Suzuki T, Kudo K, Niino H. Uptake rates of 18F-fluorodeoxyglucose and 11C-choline in lung cancer and pulmonary tuberculosis: a positron emission tomography study. Chest. 2003;124:893-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 102] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Goo JM, Im JG, Do KH, Yeo JS, Seo JB, Kim HY, Chung JK. Pulmonary tuberculoma evaluated by means of FDG PET: findings in 10 cases. Radiology. 2000;216:117-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 246] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 5. | Koh T, Taniguchi H, Yamaguchi A, Kunishima S, Yamagishi H. Differential diagnosis of gallbladder cancer using positron emission tomography with fluorine-18-labeled fluoro-deoxyglucose (FDG-PET). J Surg Oncol. 2003;84:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 75] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Rodríguez-Fernández A, Gómez-Río M, Llamas-Elvira JM, Ortega-Lozano S, Ferrón-Orihuela JA, Ramia-Angel JM, Mansilla-Roselló A, Martínez-del-Valle MD, Ramos-Font C. Positron-emission tomography with fluorine-18-fluoro-2-deoxy-D-glucose for gallbladder cancer diagnosis. Am J Surg. 2004;188:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 7. | Sanabe N, Ikematsu Y, Nishiwaki Y, Kida H, Murohisa G, Ozawa T, Hasegawa S, Okawada T, Toritsuka T, Waki S. Pancreatic tuberculosis. J Hepatobiliary Pancreat Surg. 2002;9:515-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |