Published online Sep 21, 2006. doi: 10.3748/wjg.v12.i35.5733
Revised: May 15, 2006
Accepted: May 24, 2006
Published online: September 21, 2006
A 41-year old alchoholic male with a history of chronic pancreatitis was admitted for nausea, vomiting and weight loss. Angiogram was performed and demonstrated an aneurysmal sac with a narrow neck originating from the inferior aspect of the distal portion of the proper hepatic artery. The origin of the pseudoaneurysm was covered with a 5 mm × 2.5 cm Viabahn cover stent (Gore). A repeat angiogram showed some leak and a second stent (6 mm × 2.3 cm) was deployed and overlapped with the first stent by 3 mm. Contrast was injected and a repeat angiogram demonstrated complete exclusion of the aneurysm. A repeat computerized axial tomography (CAT) scan of the abdomen after 24 h showed successful stenting. The patient had an uneventful post-operative course.
- Citation: Singh CS, Giri K, Gupta R, Aladdin M, Sawhney H. Successful management of hepatic artery pseudoaneurysm complicating chronic pancreatitis by stenting. World J Gastroenterol 2006; 12(35): 5733-5734
- URL: https://www.wjgnet.com/1007-9327/full/v12/i35/5733.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i35.5733
Hepatic artery pseudoaneurysm (HAP) is a serious complication of acute or chronic surgical injury to the hepatic artery. It is also seen following blunt and penetrating abdominal injury as well as in patients with chronic pancreatitis and after orthotopic liver transplantation[1]. Transcatheter embolization has been considered the treatment of choice but we report a case of HAP successfully treated by stenting of the pseudoaneurysm.
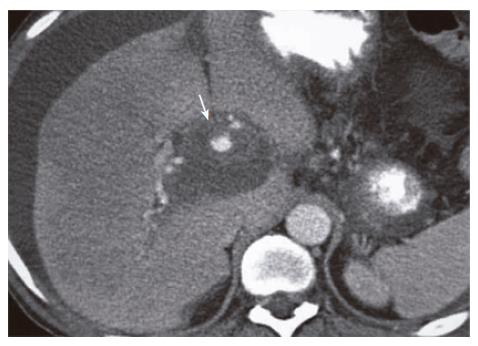
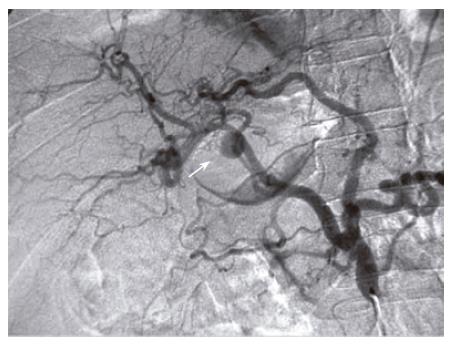
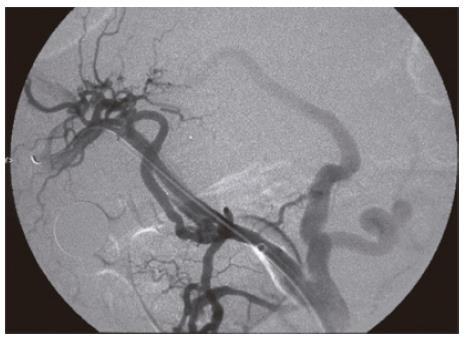
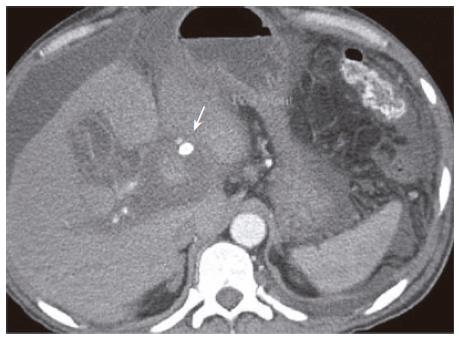
A 41-year old male with a history of chronic alchohol consumption and chronic recurrent pancreatitis presented to the emergency department with abdominal pain, nausea and weight loss. Physical examination revealed remarkable ascites. No bruit was present. Serum upper gastrointestinal (GI) endoscopy revealed grade 1 esophageal varices. Abdominal ultrasonography (USG) demonstrated dilated pancreatic ducts. Abdominal MRI/MRA showed a lesion in the porta hepatis measuring 5 cm × 5 cm. Contrast-enhanced CAT scan of the abdomen showed a 6 cm × 6 cm pseudoaneurysm of the proper hepatic artery (Figure 1). Stenting of the pseudoaneurysm was done. The technique could selectively catheterize the proper hepatic artery by using a 5 French RC-1 catheter (Angiodynamic-Queensbury-NY). Angiogram was performed and demonstrated an aneurysmal sac with a narrow neck originating from the inferior aspect of the distal portion of the proper hepatic artery (Figure 2). The origin of the pseudoaneurysm was covered with a 5 mm × 2.5 cm Viabahn cover stent (Gore). A repeat angiogram showed some leak and a second stent (6 mm × 2.3 cm) was deployed and overlapped with the first stent by 3 mm. Contrast was injected and a repeat angiogram demonstrated complete exclusion of the aneurysm (Figure 3). A repeat computerized axial tomography (CAT) scan of the abdomen after 24 h showed successful stenting (Figure 4). The patient had an uneventful post-operative course.
Hepatic artery pseudoaneurysms are rare. However, rupture is common and occurs in 76% of patients. The mortality of patients requiring operative intervention is 75%[1]. Psudoaneurysm formation in pancreatitis is thought to occur because of autodigestion of pancreatic enzymes, especially elastase, liberated due to pancreatitis. Although angiography remains the gold standard for detection of pancreatitis, USG and CAT scan are often diagnostic and may provide an early mechanism for identifying patients with pseudoaneurysms occurring consequently to pancreatitis[2]. Otherwise diagnosis is usually made late in the course of disease when severe or even fatal hemorrhage has occurred.Transcatheter embolization is the standard of care.
Literature search revealed one case report of a 60-year old female with HAP as a complication of surgical treatment of Klatskin tumor treated with a coronary stent-graft via transfemoral approach[3]. Two other cases have been reported, one being stenting of HAP secondary to liver transplantation following unsuccessful coil embolization[4] and the other being stenting of HAP secondary to therapeutic management of a choledochol cholangiocarcenoma, following failed arterial embolization[5]. In our case HAP developed as a complication of chronic alchoholic pancreatitis with symptoms of abdominal pain. Early diagnosis with CAT scan followed by stenting resulted in complete occlusion of the pseudoaneurysm.
The long-term data regarding the use of this or other stent-grafts in the visceral vessels are extremely limited, and consequently we cannot recommend stent-grafts as the primary treatment option for visceral artery pseudoaneurysms. However, we expect that, with continued follow-up of cases such as these, further refinements in stent-graft design, greater availability, and increased operator experience, these devices will become an increasingly valuable therapeutic option. Early diagnosis and intervention with stenting, which is a reasonable alternative to embolization, can result in excellent long-term outcome.
S- Editor Wang J L- Editor Wang XL E- Editor Bi L
| 1. | Finley DS, Hinojosa MW, Paya M, Imagawa DK. Hepatic artery pseudoaneurysm: a report of seven cases and a review of the literature. Surg Today. 2005;35:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Tessier DJ, Fowl RJ, Stone WM, McKusick MA, Abbas MA, Sarr MG, Nagorney DM, Cherry KJ, Gloviczki P. Iatrogenic hepatic artery pseudoaneurysms: an uncommon complication after hepatic, biliary, and pancreatic procedures. Ann Vasc Surg. 2003;17:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Venturini M, Angeli E, Salvioni M, De Cobelli F, Trentin C, Carlucci M, Staudacher C, Del Maschio A. Hemorrhage from a right hepatic artery pseudoaneurysm: endovascular treatment with a coronary stent-graft. J Endovasc Ther. 2002;9:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Maleux G, Pirenne J, Aerts R, Nevens F. Case report: hepatic artery pseudoaneurysm after liver transplantation: definitive treatment with a stent-graft after failed coil embolisation. Br J Radiol. 2005;78:453-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Paci E, Antico E, Candelari R, Alborino S, Marmorale C, Landi E. Pseudoaneurysm of the common hepatic artery: treatment with a stent-graft. Cardiovasc Intervent Radiol. 2000;23:472-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |