INTRODUCTION
Hematemesis of ruptured high flow gastric varices from intratumoral arterioportal shunt is a critical condition. The transjugular intrahepatic portosystemic shunt (TIPS)[1-2] and percutaneous transhepatic obliteration (PTO) are contraindications for portal hypertension accompanied with a marked intratumoral arterioportal shunt. Balloon-occluded retrograde obliteration (BRTO)[3-8] also has never been reported as a treatment of high flow gastric varices with an intratumoral arterioportal shunt because stagnation of the sclerosing agent cannot be obtained. Endoscopic intravariceal sclerotherapy is applicable for the ruptured gastric varices. However, it might induce rebleeding at the puncture site as a complication.
We report a case in which BRTO combined with temporary balloon occlusion of a hepatic artery for bleeding gastric varices accompanied by the intratumoral arterioportal shunt was effective in thrombosing the varices resulting in a lifesaving outcome.
CASE REPORT
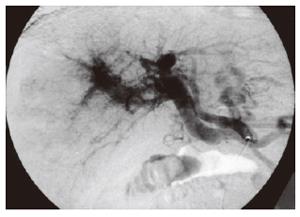
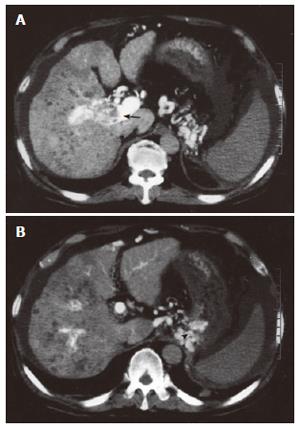
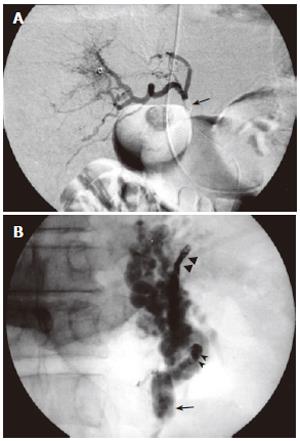
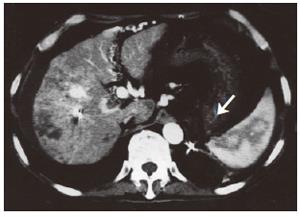
A 69-year old man with hepatocellular carcinoma (HCC) was referred to our hospital to undergo transcatheter arterial anticancer drug infusion and radiation therapy for tumor thrombi in the right portal vein visualized on contrast-enhanced CT. Angiography was performed to delineate the extent of the tumor thrombi and to infuse anticancer drugs from the proper hepatic artery. Celiac arteriography using a 4F catheter (RC2; Medikidt, Tokyo, Japan) showed a hypervascular tumor stain in the right lobe and a marked intratumoral arterioportal shunt accompanied with reflux into the main portal vein and gastric varices (Figure 1). Then, the 4F catheter was advanced to the proper hepatic artery and computed tomography during hepatic arteriography (CTHA) at 5 mm slices with injection of contrast agent (Iopamidol, 140 mgI; Daiichi, Tokyo) at a speed of 2 mL for a total volume of 60 mL. The CTHA showed HCC with the tumor thrombi in the right branch of the portal vein (Figure 2A) and a marked intratumoral arterioportal shunt with reflux into the main portal vein and gastric varices (Figure 2B). Anticancer drugs (10 mg mitomycin C and 40 mg farmorubicin) were infused from the proper hepatic artery. Ten days later, massive hematemesis occurred in the patient. Blood tests showed severe anemia and liver dysfunction (RBC/Hb/Hct 168/5.4/16.1, sGOT/sGPT/ T.B 549/103/1.3). There was hesitation to perform an endoscopic intravariceal sclerotherapy because of apprehension of rebleeding by the direct puncture of the high flow varices. Then, endovascular intervention was selected. First, a 14 mm diameter balloon catheter (Selecon 7F Straight MP catheter; Clinical Supply, Gifu, Japan) through a 7F sheath (J Sheath; Medikidt, Tokyo, Japan) was inserted from the right jugular vein and advanced into the outflow pathway of a gastrorenal (GR) shunt. The GR shunt was occluded by the inflated balloon and a retrograde injection of contrast agent was performed. However, the contrast agent was dispersed to the left inferior phrenic vein (IPV) and other flow tracts rapidly, and gastric varices were not visualized. Then, the left IPV and other flow tracts were embolized with micro-spring coils (Trufill; Cordis, Miami, FL and Tornade coil. Cook) through a 3 F microcatheter (Micropherette, Cook). After embolization of their tracts, however, the gastric varices remained unopacified by balloon-occluded retrograde venography. High blood flow through the arterioportal shunt was the main cause. In the absence of stagnation of the contrast agent, complete thrombolization of the gastric varices was impossible by BRTO and the complications due to massive systemic leakage of ethanolamine oleate (EO) as a sclerosing agent were also feared. In order to stagnate the blood flow of GR shunt, temporary balloon occlusion of the proper hepatic artery was performed using a 9 mm balloon catheter (Selecon, 5F Straight, Clinical Supply) (Figure 3A). Under temporary balloon occlusion of the proper hepatic artery, the outflow pathway of the GR shunt was reclosed by inflating the 14 mm diameter balloon. It led to the visualization of the stagnant gastric varices with balloon-occluded retrograde venography. Five percent EO solution, which is a mixture of 10% EO (Oldamin; Grelan Pharmaceutical, Tokyo, Japan) and the same dose of a nonionic contrast medium (Iopamiron 370 mgI/dL; Schering Osaka, Japan), were slowly injected into the GR shunt during the dual balloon occlusion after venous drip infusion of human haptoglobin (Mitsubishi Pharma, Osaka, Japan) at a total volume of 4000 units. The gastric varices were filled with 30 mL of 5% EO solution (Figure 3B). The balloon catheter in the proper hepatic artery was deflated and removed after one hour. Patency of the proper hepatic artery was confirmed by contrast agent injection from the catheter before removal. The balloon occlusion of the GR shunt was maintained for 24 h. Contrast-enhanced CT performed on the following day showed thrombosed gastric varices (Figure 4). Following BRTO, blood pressure and other vital signs stabilized, and progression of anemia was halted. Worsening of hepatic function was not recognized (sGOT/sGPT/T.B 108/73/1.3). After that, the patient could undergo radiation therapy for the portal tumor thrombi.
Figure 1 Celiac arteriography showing a marked arterioportal shunt with tumorous thread and streak sign and massive reverse flow to the main trunk of the portal vein.
Figure 2 CT during proper hepatic arteriography showing tumor thrombi (arrow) in the right portal vein (A) and gastric varices (arrowhead) (B).
Figure 3 BRTO combined with temporary balloon occlusion of the hepatic artery.
A: Proper hepatic arteriography through the balloon catheter during balloon occlusion (arrow); B: Balloon-occluded retrograde venography (arrow) after embolization of the left inferior phrenic vein and the retroperitoneal vein with micro-spring coils (arrowheads) showing the stagnant gastrorenal shunt and gastric varices. A 5% ethanolamine oleate mixture (30 mL) was then injected during dual balloon occlusion.
Figure 4 Contrast-enhanced CT showing thrombosed gastric varices (white arrow) on the following day.
DISCUSSION
Kanagawa et al[3] first introduced BRTO as an effective therapy for gastric varices in 1990. BRTO is performed by injecting a sclerosing agent from the balloon catheter through the outflow pathway of the gastro-renal shunt during balloon occlusion[3,4]. The success rate of gastric varix sclerosis reaches 85%-100%[3-8]. Five percent ethanolamine oleate iopamidol (EOI) is usually used as the sclerosing agent with retrograde injection. Massive systemic leakage of ethanolamine oleate causes various complications such as acute respiratory distress syndrome[9,10], acute renal disorder[11] and disseminated intravascular coagulation[12]. Though human haptoglobin[11,13] has been used to prevent such complications, leakage into the systemic circulation must be minimized. In cases of multiple outflow tracts such as inferior phrenic vein, pericardiophrenic vein, and other outflows, embolization of these outflow tracts with micro-spring coils is performed to reduce the injection volume of EO and prevent systemic leakage[8].
In our case, BRTO alone was anticipated to lead to inadequate occlusion of the outflow tract and massive systemic leakage of EOI because of high blood flow from the intratumoral arterioportal shunt. According to the classification of the degree of progression of gastric varices[6], the high flow gastric varices in which the GR shunt cannot be occluded with the balloon catheter alone, belong to the highest grade 5. In patients with the most progressive gastric varices, partial splenic embolization and PTO of the coronary vein as a main inflow route are required to reduce the blood flow into varices before BRTO[6]. However, no description about the procedure to treat gastric varices accompanied with a marked intratumoral arterioportal shunt is available. Transcatheter embolization is an effective treatment for variceal bleeding due to portal hypertension caused by arterioportal fistulae[14-16]. In cases of portal tumor thrombi, however, transcatheter embolization of the hepatic artery with gelatin sponge particles, metallic coils and other permanent embolic materials to reduce the arterial flow into varices can cause a large liver infarction and hepatic failure[17]. Temporary occlusion of the proper hepatic artery using a balloon catheter to reduce blood flow through the arterioportal shunt prevents liver infarction, minimizes systemic leakage of EO and permits complete thrombosis of the gastric varices by concurrent BRTO. Temporary balloon-occluded proper hepatic arterial infusion of anticancer drugs can be performed for HCC with portal tumor thrombi and is a safe procedure because short-term ischemia has little effect on hepatic function[18]. In this case, there was no deterioration of liver function after BRTO during temporary balloon occlusion of the hepatic artery. There is no previous report describing the feasibility of BRTO during temporary balloon occlusion of the hepatic artery for hemorrhagic gastric varices with a marked intratumoral arterioportal shunt.
In conclusion, BRTO combined with temporary occlusion of a proper hepatic artery is a safe and useful method for the treatment of ruptured high flow gastric varices with a marked intratumoral arterioportal shunt.