Published online Sep 7, 2006. doi: 10.3748/wjg.v12.i33.5393
Revised: February 8, 2005
Accepted: February 21, 2005
Published online: September 7, 2006
We report the case of a 65-year old male patient who initially presented with recurrent episodes of upper abdominal pain, lack of appetite and weight loss. Abdominal ultrasound indicated enlarged intrahepatic bile ducts, abdominal CT scan and ERC were performed and bile duct carcinoma (Klatskin Type III b) was diagnosed. The tumor was located in the segments 2,3,4 and 1 with possible invasion of the left intrahepatic portal vein. Both the segments 2 and 3 of the liver were atrophic and displayed a cholestatic bile duct system. Preoperatively an intraductal stent was placed in the left bile duct using ERC to drain the left hepatic lobe. A specimen of the ascites present preoperatively displayed no malignant cells. After evaluation of the preoperatively obtained data left hepatic resection was planned. Following laparotomy we found local peritoneal carcinosis in the ligamentum hepatoduodenale with lymphatic nodules that tested positive for cholangiocellular carcinoma in online pathological examination. In the course of further exploration of the abdomen a solid tumor was detected in the sigmoid colon. Regarding the advanced stage of the neoplasm it was decided to cancel hemihepatectomy and perform sigmoid resection only in order to guarantee uncomplicated intestinal passage. The sigmoid colon was removed by a typical resection technique with end-to-end anastomosis. Histological examination of the resected sigmoid revealed transmural manifestation of a malignant neoplastic process with both a tubular and a solid growth pattern in conformity with metastasis of a Klatskin tumor. The mucosal layer showed no neoplastic alteration. Peritoneal carcinosis is a common phenomenon in the dissemination pattern of advanced-stage Klatskin tumors, yet to our knowledge this is the first case of intramural colonic growth following peritoneal metastasis.
- Citation: Schmeding M, Neumann U, Neuhaus P. Colonic metastasis of Klatskin tumor: Case report and discussion of the current literature. World J Gastroenterol 2006; 12(33): 5393-5395
- URL: https://www.wjgnet.com/1007-9327/full/v12/i33/5393.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i33.5393
Bile duct tumors are rare neoplasms with an incidence of 0.5-1/100 000[1]. Predisposing factors include mainly PSC with a thirty-fold increased risk as well as choledochal cysts and parasitic infections (clonarchis sinensis, opisthordis viverrini et felineus)[1,2]. These tumors usually present with clinical symptoms such as upper right abdominal pain, weight loss or jaundice at a rather advanced stage when the process has already grown to a rather significant extent. The tumor type and localisation are categorized according to the Bismuth criteria[3]. After quite a sceptical approach towards surgical therapy for Klatskin tumors until the early 1990s, during the last years surgical results have demonstrated that even patients with a locally advanced stage of proximal bile duct carcinoma without distant metastasis profit from surgical resection[3,4,5]. Today 5-year survival rates from 10% to 40% are reported with even higher survival rates in specialized centers[6,7,8].
We report the case of a 65-year old male patient who had experienced episodes of upper abdominal pain for several months. When presentation at our institution he did not develop jaundice, bilirubin was 0.6 mg/dL after stent-placement in the left hepatic duct prior to admittance to our institution.
Due to lack of appetite he had lost five kilograms over the last four months. Laboratory values at admission time were as follows: total bilirubin 0.6 mg/dL, conj. 0.4 mg/dL, AST 75 U/L, ALT 39 U/L, gGT 63 U/L, AP 82 U/L, lipase 210 U/L, amylase 278 U/L, leokozytes 9.29/nL, thrombozytes 206/nL, Hb 11.5 g/dL, TPZ 83%, INR 1.15 CEA 2.6 μg/L, AFP 29 μL/L, CA 19-9 803 U/mL.
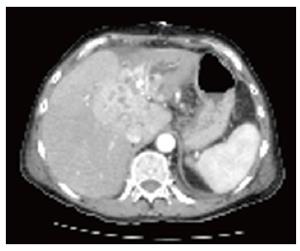
Clinical examination revealed a man of reduced physical fitness considering his age and upper right abdominal pain at palpation. After abdominal ultrasound indicating enlarged intrahepatic bile ducts a CT scan was performed demonstrating a mass of hypervascularized tissue in the central liver hilus within the segments 2, 3, 4 and 1. Enlarged lymphatic nodes in the hepato-duodenal ligament could also be detected. The left intrahepatic bile duct system proximal of the tumor was markedly enlarged with signs of massive cholestasis.
CT scan showed Klatskin tumor Typ III b growth with intrahepatic bile duct enlargement, cholestasis and atrophy of the left hepatic lobe (Figure 1).
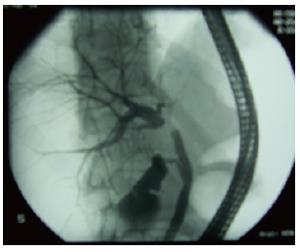
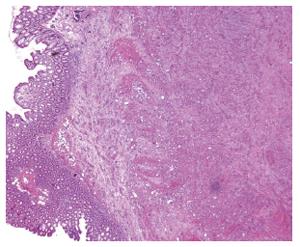
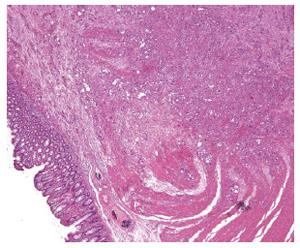
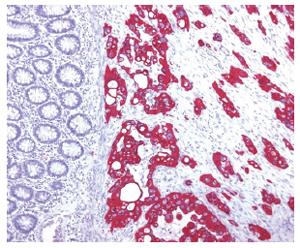
An endoscopic retrograde cholangiography (ERC) was then conducted to examine the detailed bile duct anatomy. This displayed good filling of the right intrahepatic bile duct system whereas the left system could not be displayed due to tumorous stenosis in the distal part of the ductus hepaticus sinister reaching into the ductus hepaticus communis (Figure 2). After careful preoperative evaluation the patient was subjected to surgical resection. At the start of the surgical procedure multiple positive lymphatic nodules were detected in the hepatoduodenal ligament. While further exploring the peritoneal cavity for potential additional manifestations of the tumor a solid mass could be found in the sigmoid colon. As this was a preoperatively unknown process which appeared highly suspicious to be of neoplastic origin, it was decided to resect this segment of the colon. Sigmoid resection was performed using the standard no-touch technique. The resected sigmoid colon was then subjected to histological examination: Histomorphology and immune-histochemistry revealed an intramural colonic metastasis of a badly differentiated adenocarcinoma of the bile duct displaying solid as well as tubular segments of growth with a large number of mitotic cells. No neoplastic alteration of the colon mucosa could be detected.
A separately growing sigmoid neoplasm of colonic origin could be ruled out (Figures 3 and 4). Histological examination of the resected colonic neoplasm revealed intramural metastasis of adenocarcinoma infiltrating the muscular and submucosal layers (Figure 5). Immune-histological staining showed adenocarcinoma of the non-intestinal klatskinoide type.
As far as our clinical experience and the extensive literature research are concerned, this is the first case ever reported of colonic metastasis of Klatskin type bile duct carcinoma.
Lymphatic metastasis of Klatskin tumors into lymph nodes along the hepatoduodenal ligament is a common and well-known phenomenon as is intrahepatic dissemination to areas distant from the original tumor location[1,3,6]. In more advanced stages of the disease we have also found peritoneal carcinosis and lung metastasis. Intestinal dissemination of a Klatskin tumor has not been reported up to date.
As careful pathological inspection-revealed colonic metastatis is not merely due to peritoneal carcinosis spreading to the serosa of the sigmoid colon but originates within the intestinal wall.
In the advanced stage of bile duct carcinoma, peritoneal carcinosis leads to spreading of neoplastic cells within the abdominal cavity and consecutive tumor growth in multiple and various locations. Furthermore dissemination of cancer cells during surgery for bile duct carcinoma can lead to tumor cell spreading followed by metastasis in surgical scars[9,10]. Whereas these phenomena lead to malignant cell growth originating from the serosal layer where metastatic cells are initially implanted, our case describes the continuing growth of disseminated bile duct carcinoma cells into and within the intestinal wall of the sigmoid colon.
While this case remains unique up to date, it may suggest to include colonoscopy in the preoperative staging procedures in selected cases.
S- Editor Wang J L- Editor Wang XL E- Editor Ma WH
| 1. | Nagorney DM, McPherson GA. Carcinoma of the gallbladder and extrahepatic bile ducts. Semin Oncol. 1988;15:106-115. [PubMed] |
| 2. | Rosen CB, Nagorney DM, Wiesner RH, Coffey RJ Jr, LaRusso NF. Cholangiocarcinoma complicating primary sclerosing cholangitis. Ann Surg. 1991;213:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 231] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992;215:31-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 512] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 4. | Pichlmayr R, Lamesch P, Weimann A, Tusch G, Ringe B. Surgical treatment of cholangiocellular carcinoma. World J Surg. 1995;19:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 92] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Pichlmayr R, Weimann A, Klempnauer J, Oldhafer KJ, Maschek H, Tusch G, Ringe B. Surgical treatment in proximal bile duct cancer. A single-center experience. Ann Surg. 1996;224:628-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 211] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer. 1995;75:171-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 7. | Gores GJ. Cholangiocarcinoma: current concepts and insights. Hepatology. 2003;37:961-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 198] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 8. | Launois B, Terblanche J, Lakehal M, Catheline JM, Bardaxoglou E, Landen S, Campion JP, Sutherland F, Meunier B. Proximal bile duct cancer: high resectability rate and 5-year survival. Ann Surg. 1999;230:266-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | ten Hoopen-Neumann H, Gerhards MF, van Gulik TM, Bosma A, Verbeek PC, Gouma DJ. Occurrence of implantation metastases after resection of Klatskin tumors. Dig Surg. 1999;16:209-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Washburn WK, Lewis WD, Jenkins RL. Aggressive surgical resection for cholangiocarcinoma. Arch Surg. 1995;130:270-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 128] [Article Influence: 4.3] [Reference Citation Analysis (0)] |