Published online Aug 21, 2006. doi: 10.3748/wjg.v12.i31.5081
Revised: March 9, 2006
Accepted: March 13, 2006
Published online: August 21, 2006
Tailgut cyst is a rare congenital cystic lesion arising from the remnants of the embryonic postanal gut. It occurs exclusively within the retrorectal space and rarely in the perirenal area or in the subcutaneous tissue. A prerectal and retrovesical location of tailgut cyst is extremely rare. To the best of our knowledge, only three cases have been reported in the English literature. We experienced an unusual case of tailgut cyst developed in the prerectal and retrovesical space in a 14-year-old boy. Abdominal computed tomography demonstrated a prerectal cyst which was located at the anterolateral portion to the rectum. The cyst contained yellowish inspissated mucoid material. Microscopically, the cyst was lined by squamous, columnar, cuboidal and transitional epithelia and the wall was fibrotic with dispersed smooth muscle cells. Although tailgut cyst arising in prerectal area is extremely rare, its possibility should be considered in differential diagnosis of a prerectal and retrovesical cystic mass.
- Citation: Jang SH, Jang KS, Song YS, Min KW, Han HX, Lee KG, Paik SS. Unusual prerectal location of a tailgut cyst: A case report. World J Gastroenterol 2006; 12(31): 5081-5083
- URL: https://www.wjgnet.com/1007-9327/full/v12/i31/5081.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i31.5081
Tailgut cyst, known as a retrorectal cystic hamartoma, is a rare congenital multicystic lesion arising from the remnants of the embryonic postanal gut[1-3]. It almost exclusively occurs within the retrorectal or presacral space[4] and rarely in the perirenal area[2,3,5], the subcutaneous tissue in the anorectal region[6-9] and anterior to the rectum[4,10]. The prerectal location of a tailgut cyst is extremely rare. To the best of our knowledge, only three cases have been reported in the English literature. Here we report an additional case of tailgut cyst arising in the prerectal and retrovesical space and review the relevant literature.
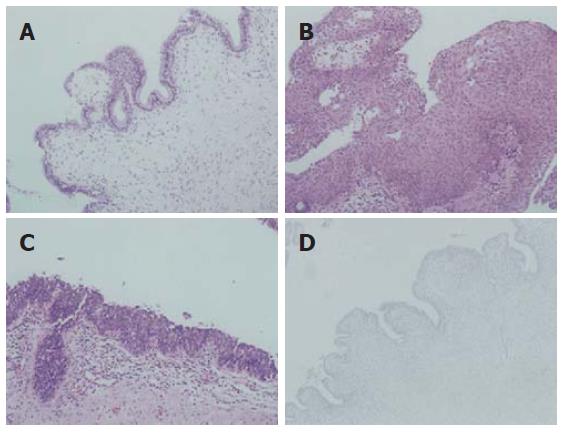
A 14-year-old boy presented with abdominal pain and dysuria for 2 d. Physical examination revealed suprapubic pain and tenderness. Routine laboratory tests including a complete blood count, electrolytes, and routine urine analysis were within normal limits. Abdominal computerized tomography demonstrated a well-demarcated oval-shaped cystic mass which was located at the prerectal and retrovesical space (Figure 1). He underwent explorative laparotomy for the definite diagnosis and treatment. Intra-operative finding showed that the cyst did not communicate with the prostate, bladder or rectum. Complete mass excision was performed. Macroscopic examination revealed an unilocular cyst measured 5 cm × 3 cm in cross diameter. The cyst showed a thickened fibrous wall and focal adhesion to the adjacent fibroadipose tissue. The cyst contained yellowish inspissated mucoid material. Microscopically, the cyst showed a variety of the lining epithelia including glandular, cuboidal, transitional and squamous epithelia (Figure 2). The cyst wall contained disorganized bundles of smooth muscle cells. The underlying stroma showed mild infiltration of chronic inflammatory cells. On immunohistochemical staining, prostate specific antigen (PSA) and neuroendocrine markers including chromogranin A were negative in the lining of the epithelial cells. The patient’s recovery remained uneventful for 10 mo postoperation.
Tailgut cyst or retrorectal hamartoma, is a rare congenital multicystic lesion and is believed to originate from the remnant of the tailgut which is a primitive gut temporarily present at the caudal portion of the embryo[2,3,8]. During its development the embryo possesses a true tail, reaching its largest diameter on the 35th d of gestation. The anus develops above the tail on the 56th d of gestation, by which time the latter has completely regressed. Remnants of the tailgut or neuroenteric cord may be the origin of tailgut cysts[3,11].
Tailgut cyst can affect at any age but predominantly middle aged women. The female to male ratio is about 3:1. Half of them are asymptomatic and are frequently found on routine physical examination[1,4]. Symptomatic patients present with abdominal pain, rectal bleeding, and rectal fullness[2]. Complete surgical excision is necessary for accurate diagnosis and treatment, and prevents complications of the tailgut cyst, including infection, recurrence, and malignant transformation[1]. Tailgut cyst is usually a well-circumscribed, soft, and multicystic or multilocated mass with adherent surrounding fibroadipose tissue. The varying-sized cysts contain clear serous or translucent mucoid fluids. Microscopically, the cysts are lined by a wide variety of epithelia varying from cyst to cyst, or even within the same cyst. Epithelia can be divided into the following types, such as the stratified squamous type, transitional and cuboidal type, stratified columnar type, ciliated pseudostratified columnar and gastric type. In most cases the cyst wall contains well-formed disorganized focal bundles of bland smooth muscle cells[2,3].
Tailgut cyst occurs almost exclusively in the retrorectal or presacral space. Infrequently, the cysts extend from the presacral space to involve the rectal wall and rarely extend laterally from the mid-line or into the postsacral space or lateral and anterior to the rectum[4], but occur rarely in the perirenal area, the subcutaneous tissue in the anorectal region and anterior to the rectum[2-10]. The prerectal location of tailgut cyst was noted in our patient. To the best of our knowledge, only three cases have been reported in the English literature[4,10].
The main differential diagnoses of the prerectal tailgut cyst include the utricle cyst in the prostate, the rectal duplication and the simple cyst in the seminal vesicle. The prostatic utricle cyst, known as mullerian duct remnant, is a midline cyst of the prostate and also occurs in the prerectal or retrovesical area. Histologically, the cyst is lined with stratified columnar or cuboidal epithelium and continuous with the utricular wall. Immunohistochemically, the cyst lining epithelial cells show immunoreactivity for PSA and the neuroendocrine cells show immunoreactivity for chromogranin A[12]. Duplication cyst is lined by epithelium similar to that of the gastrointestinal and respiratory tracts. The epithelium simulates normal mucosa of the gut. The main distinctive feature is a well-formed muscular wall overlying two layers of muscular bundles containing a nerve plexus[2,3]. The simple cyst in the seminal vesicle is an unilocular cystic lesion located at lateral to the midline in the retrovesical area. The cyst is lined with a cuboidal or flattened epithelium with a fibrous wall of variable thickness. Characteristically, the fluid within the cyst contains sperm or sperm fragments[13].
In conclusion, we report an unusual case of tailgut cyst arising in prerectal and retrovesical area in a 14-year-old boy. Although tailgut cyst arising in prerectal area is extremely rare, its possibility should be considered in differential diagnosis of a prerectal and retrovesical cystic mass.
S- Editor Wang J L- Editor Wang XL E- Editor Ma N
| 1. | Killingsworth C, Gadacz TR. Tailgut cyst (retrorectal cystic hamartoma): report of a case and review of the literature. Am Surg. 2005;71:666-673. [PubMed] |
| 2. | Sung MT, Ko SF, Niu CK, Hsieh CS, Huang HY. Perirenal tailgut cyst (cystic hamartoma). J Pediatr Surg. 2003;38:1404-1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Kang JW, Kim SH, Kim KW, Moon SK, Kim CJ, Chi JG. Unusual perirenal location of a tailgut cyst. Korean J Radiol. 2002;3:267-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Hjermstad BM, Helwig EB. Tailgut cysts. Report of 53 cases. Am J Clin Pathol. 1988;89:139-147. [PubMed] |
| 5. | Mills SE, Walker AN, Stallings RG, Allen MS Jr. Retrorectal cystic hamartoma. Report of three cases, including one with a perirenal component. Arch Pathol Lab Med. 1984;108:737-740. [PubMed] |
| 6. | Sidoni A, Bucciarelli E. Ciliated cyst of the perineal skin. Am J Dermatopathol. 1997;19:93-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Rafindadi AH, Shehu SM, Ameh EA. Retrorectal cystic harmatoma (tailgut cyst) in an infant: case report. East Afr Med J. 1998;75:726-727. [PubMed] |
| 8. | Murao K, Fukui Y, Numoto S, Urano Y. Tailgut cyst as a subcutaneous tumor at the coccygeal region. Am J Dermatopathol. 2003;25:275-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Song DE, Park JK, Hur B, Ro JY. Carcinoid tumor arising in a tailgut cyst of the anorectal junction with distant metastasis: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:578-580. [PubMed] |
| 10. | Gips M, Melki Y, Wolloch Y. Cysts of the tailgut. Two cases. Eur J Surg. 1994;160:459-460. [PubMed] |
| 11. | Levert LM, Van Rooyen W, Van Den Bergen HA. Cysts of the tailgut. Eur J Surg. 1996;162:149-152. [PubMed] |
| 12. | Kato H, Komiyama I, Maejima T, Nishizawa O. Histopathological study of the müllerian duct remnant: clarification of disease categories and terminology. J Urol. 2002;167:133-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Petersen RO. Urologic pathology, 2nd ed. Philadelphia: Lippincott 1992; 648-651. |