Published online Jan 21, 2006. doi: 10.3748/wjg.v12.i3.431
Revised: June 29, 2005
Accepted: July 28, 2005
Published online: January 21, 2006
AIM: To evaluate the efficacy of hilar duct oriented hepatectomy for intractable hepatolithiasis, the ventral hilum exposure (VHE) method that has been applied by the authors.
METHODS: From June 1994 to June 2004 for a period of 10 years, 153 patients who had Tsunoda type III or IV hepatolithiasis, received hepatectomy at our institution. Among these patients, 128 who underwent hepatectomy by the VHE method were the subjects for the study. We analyzed the risk of this procedure, residual rate of intra-hepatic stones, and stone recurrent rates.
RESULTS: The average age was 54.2 years, and the male to female ratio was 1:1.7. The average follow-up period was 25.6 mo (6-114 mo). There was no post-operative severe complication or mortality after the operation. The rate of residual stones was 5.4% and the rate of recurrent stones was 4.2%.
CONCLUSION: VHE is a safe surgical procedure and provides favorable treatment results of intractable hepatolithiasis. Especially, this procedure has advantage in that intra-hepatic bile duct stricture may be confirmed and corrected directly during surgery.
- Citation: Kim BW, Wang HJ, Kim WH, Kim MW. Favorable outcomes of hilar duct oriented hepatic resection for high grade Tsunoda type hepatolithiasis. World J Gastroenterol 2006; 12(3): 431-436
- URL: https://www.wjgnet.com/1007-9327/full/v12/i3/431.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i3.431
Although hepatolithiasis is a benign condition, the clinical progression of this disease not only often limits a patient’s social activities, sometimes to an extreme degree, but also may lead to liver parenchymal destruction due to recurrent cholangitis or even septic death if adequate treatment is not provided. Moreover, cholangiocarcinoma is found in approximately 5-10% of patients with hepatolithiasis[1,2]. The incidence of hepatolithiasis in the Korean population has been reported as 15% of all biliary tract stones, which is relatively higher than the data reported in Western populations[3].
In clinical practice, however, the treatment results are less favorable when compared to those of extrahepatic bile duct stones. The reason for this is the stricture of the intra-hepatic duct as a major cause of hepatolithiasis[4,5], which is commonly intractable because of the anatomical characteristics. It has been known that the most important aspects in the treatment of hepatolithiasis is the complete removal of all intra-hepatic stones and resolution of accompanied intra-hepatic duct stricture, in order to reduce the incidence of post-operative cholangitis and stone recurrence[6].
Recent developments in endoscopic techniques have also been shown to result in favorable outcomes[7]. Such advances have led to the shifting of surgical practice from uniform surgery to a combination of surgery and endoscopy for the treatment of hepatolithiasis[8,9]. But the endoscopic approach for hepatolithiasis is not always successful due to various intra-hepatic duct anatomies and cannot solve concomitant liver atrophy or latent cholangiocarcinoma.
The authors of this study implemented a surgical approach for hepatolithiasis according to the Tsunoda classification of hepatolithiasis, which describes the intra-hepatic duct in terms of dilatation and strictures, and is as follows: type I, no marked dilatation or strictures of intra-hepatic bile ducts; type II, diffuse dilatation of the intra-hepatic biliary tree without intra-hepatic duct strictures and frequently a stricture of the distal common bile duct; type III, unilateral solitary or multiple cystic intra-hepatic dilatation, frequently accompanied by stenosis of the left or right intra-hepatic bile ducts; and type IV, the same attributes as type III but with bilateral involvement of hepatic lobes[10]. The authors’ policy of treatments in hepatolithiasis is according to Tsunoda type, that is, the type I or II is treated with endoscopic approach and the type III or IV is with surgical approach.
From June 1994 to June 2004, a retrospective review was undertaken of 153 patients who received partial hepatectomy for hepatolithiasis at our institution, among whom, 128 patients underwent hilar duct oriented hepatectomy (ventral hilum exposure method, VHE). We analyzed the surgical risk of VHE method, residual rate of intra-hepatic stones, stone recurrent rates, and those patients with concomitant cholangiocarcinoma were also investigated.
The definition of hepatolithiasis was according to the description by Couinaud in which a gallstone is present in the proximal portion of the confluence of the common hepatic duct. The presence of residual or recurrent hepatolithiasis after surgery were assessed by ultrasonography (US), computerized tomography (CT) scans, cholangiograms by endoscopic retrograde cholangiopancreaticography (ERCP) and/or percutaneous transhepatic cholangiography (PTC). The postoperative follow-up comprised of US every 3 mo and CT scan every 6 mo for the first three years, and then once a year thereafter, or when abnormal symptoms suspicious of cholangitis or residual or recurrent hepatolithiasis were present. If the residual or recurrent stones were suspected by US or CT scan, the PTC and/or ERCP were introduced.
Recurrent hepatolithiasis was defined as stones recurring after 2 years of initial therapy. Operative mortality and hospital mortality was defined as death of a patient within 30 d of surgery, and death before discharge from the hospital after surgery, respectively.
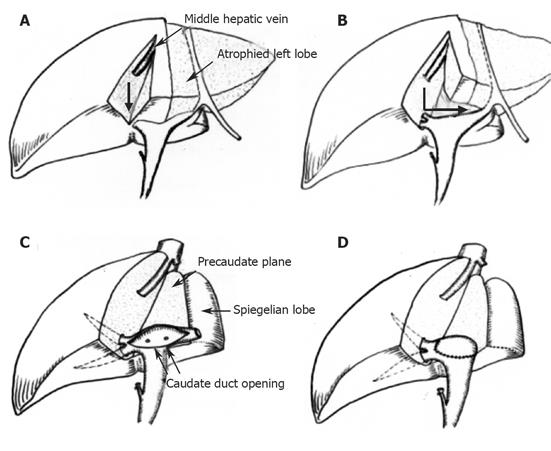
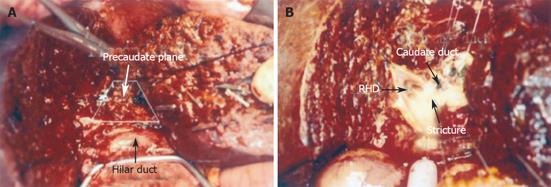
The goal of VHE is total exposure of the hilar bile duct. In case of left lobectomy, first the course of middle hepatic vein and the distribution of intra-hepatic stones are confirmed by intra-operative US, then the gallbladder is removed. A sagittal liver parenchyma dissection (hepatotomy) along the Cantlie’s line or midline of the GB bed is done until reaching the right hilar Glisson’s sheath. Then the sagittal dissection plane is rotated 90° to the left along the coronal plane or pre-caudate plane[11]. The preservation of the middle hepatic vein during sagittal hepatotomy is optional. Managed thus, long segment of the ventral portion of hilar Glisson’s sheath can be separated from dorsal part of the segment IVb liver parenchyma (Figures 1A and 1B). Without exception in our experience, the hepatic hilar bile duct is situated at the extreme antero-superior aspect in the hilar Glisson’s pedicle that can be confirmed by needle puncture aspiration of bile, and then the anterior wall of the hilar bile duct can be opened safely along its direction without the need of dissection of hilar Glisson’s sheath (Figures 1C and 1D).
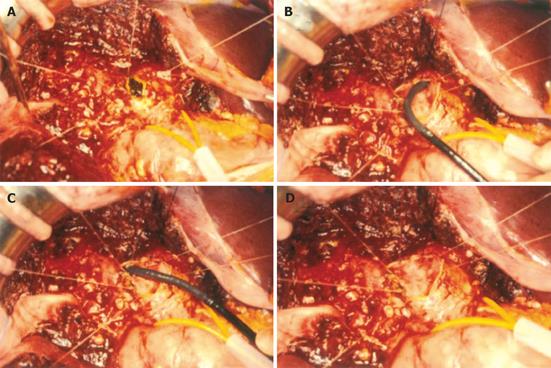
In this way, direct visualization of the openings of the second order branches of the intra-hepatic bile duct allows pronounced accuracy of intra-operative cholangioscopy in each of the intra-hepatic duct branches, and precise evaluation of the distribution of intra-hepatic stones and hilar stricture, and plastic reconstruction of the strictured hilar hepatic duct. Plastic reconstruction of intra-hepatic duct results in avoidance of a hepatico-jejunostomy in almost every patient, and also primary closure of the bile duct incision site maintains the physiologic anatomy of the intra-hepatic bile duct. The VHE procedure also resulted in easier confirmation of the common bile duct status, and none of the patients who received this therapy required a T-tube choledochostomy (Figures 2 and 3).
We did not perform VHE in cases where the hepatolithiasis was situated in the third branch or the more periphery of the intra-hepatic bile duct, when parenchymal destruction of the liver was observed in the periphery, and when no stricture was present up to the second order branches of the hilar bile duct. These patients were managed with conventional liver parenchyma resection (Table 1).
The average age of patients who received VHE surgery was 54.2 years, and the male to female ratio was 1:1.7. All 128 patients who underwent VHE surgery were Tsunoda type III or IV (98 patients were Tsunoda type III, and 30 were type IV). The type of stone in all the 153 patients who received surgery was pigment stone, and hilar duct stricture was confirmed in 90 of 128 patients who had VHE surgery (70%). In the remaining 38 patients without hilar ductal stricture, strictures were observed in the second order branches.
The average follow-up period of 128 patients after VHE for hepatolithiasis was 25.6 months (range; 6-114 mo). The number of patients with residual stones after VHE hepatectomy was 7/128 (5.4%), and residual stones were found in 4/98 patients with Tsunoda type III (4.1%) and in 3/30 with type IV (10%). Among them, there were six patients in whom residual stone removal by PTCS was performed who had symptoms such as cholangitis. And the remaining four asymptomatic patients were being followed up only with observation to date.
We could follow-up 48 patients with CT scan and US for more than two years after complete stone removal by the VHE method. The range of the follow-up period of these 48 patients was 26-116 mo, with an average of 60.4 mo. Among them, only two patients had recurrent stones, showing a recurrence rate of 4.2% (2/48). Both of these patients were Tsunoda type III at the time of surgery (Table 2). And these two recurrent patients developed cholangitis, and one died of sepsis as a result of the cholangitis. Among the 46 patients who were followed up for more than 2 years without recurrent stones, 2 developed acalculous cholangitis as the complication and were managed by conservative treatment. One patient was diagnosed with cholangiocarcinoma 3 years after surgery without evidence of stone recurrence (Table 3).
| Tsunoda type | Number of residualstone (%) | Number of recurrentstone (%) |
| III | 4/98 (4.1) | 2/39 (5.1) |
| IV | 3/30 (10) | 0/9 (0) |
| Total | 7/128 (5.4) | 2/48 (4.2) |
| Long-term results | Number of cases (%) |
| Free of symptoms and no recurrent stones | 43 (89.6) |
| Recurrent stones with cholangitis | 2 (4.2) |
| Cholangitis without recurrent stones | 2 (4.2) |
| Cholangiocarcinoma | 1 (2.1) |
Among the total of 153 patients who received hepatectomy for hepatolithiasis, there were 17 cases of cholangiocarcinoma (11%), and six of these patients were of advanced state of unresectable disease during laparotomy. There were also three patients with in situ cholangiocarcinoma after confirmation of pathology. And only three patients were pre-operatively determined to be with cholangio-carcinoma among the total of 17 cases of concomitant cholangiocarcinoma.
There was no case of operative mortality or hospital mortality in all patients who were studied. Post-VHE complications occurred in 33/128 patients (25.7%), and consisted of wound infections (20 patients, the most common complication), pulmonary complications such as pleural effusion or pneumonia (nine patients), bile leakage (four patients), and one case each of post-operative minor intra-abdominal hemorrhage, intraperitoneal abscess, and gastrointestinal bleeding. All of the complicated cases were successfully managed conservatively.
Recent therapy by the combination of endoscopy and surgery for the treatment of hepatolithiasis has allowed overcoming the limitations of each modality and therefore has led to marked enhancement of treatment results. Another reason for the increased treatment success may be due to the more accurate pre-operative evaluation of intra-hepatic bile duct strictures and distribution of intra-hepatic stones.
Many favorable results have been reported in the literature with regard to endoscopy in the management of hepatolithiasis[7,12]. In our institutional experience, analysis of endoscopic treatment results of 106 patients with hepatolithiasis has shown that the overall residual stone rate was 16%, but this rate was higher in patients with Tsunoda types III and IV (24% and 30%, respectively). We thought that this result was from the intra-hepatic stricture and the sharp angled branches of the intra-hepatic bile duct anatomy[13,14]. And it is well known that there are major limitations of endoscopic hepatolithiasis, such as parenchymal destruction of the liver, liver abscess formation, and a 5-10% incidence of cholangiocarcinoma that occurs in patients with hepatolithiasis[1,2,15,16]. Our study revealed a slightly higher rate (11%) of patients found with cholangiocarcinoma, compared to previous reports from other institutions, and the reason for this is thought to be due to the fact that patients who received surgery in our institution were those with parenchymal destruction and intra-hepatic bile duct stricture, and also because a larger number of patients were with long-standing, advanced hepatolithiasis. Another serious problem in patients with hepatolithiasis accompanied by the presence of cholangiocarcinoma is that the latter disease is not easily detected in the pre-operative evaluation, and thus may be missed during endoscopic treatment of hepatolithiasis[2,17]. This was also our finding in this study.
Endoscopic treatment of hepatolithiasis is considered to be relatively safe[18]. However, to endoscopically remove all stones completely and to resolve stricture of the intra-hepatic bile duct, the procedure is conducted on an average of 3 to 4 times at 1-2 wk intervals, restricting the patients’ activities over a long period of time, even though the procedure entails less physical and psychological burden for the patient than surgical operation.
In Korea as well as in most Asian populations, pigment stones are the most common, while cholesterol stones are predominant in Western populations. This was also the case in our study in which all patients who received surgery were with pigment stones. In contrast to cholesterol stones, pigment stones demonstrate different clinicopathologic features of the intra-hepatic bile duct. Most cholesterol hepatolithiasis are usually located in the peripheral intra-hepatic ducts, accompanied by a lesser incidence of cholangitis, there is less wall thickening of the stone-containing duct, and the presenting symptoms are usually mild. However, pigment stones are frequently accompanied by hilar duct stricture and hilar duct stones, show severe wall thickening of the stone-bearing duct, and the symptoms are more severe due to a higher incidence of cholangitis[19]. According to our knowledge of previously reported literature, we have not been able to find any reports with regard to the rate of hilar duct stricture in hepatolithiasis patients due to pigment stone. We, however, were able to observe in our study that hilar stricture was present in 90 of 153 (59%) patients. Therefore, it is the opinion of the authors that during surgery for pigment stone hepatolithiasis, resection of the stone bearing liver parenchyma and removal of stones only is inadequate because the possibly accompanied hilar strictures will make recurrent diseases, and which must be appropriately corrected during surgery.
The VHE procedure adopted and analyzed by the authors of this study has been established as a safe method in a previous report of the pre-caudate plane of the para-caval portion of the caudate lobe[11]. Anatomically, the pre-caudate plane may be described as a plane bounded inferiorly by the hilar Glisson’s pedicle, superiorly by the dorsal portion of origin of the middle hepatic vein, the left side by the ligamentum venosum, and the right side by the imaginary line of the second order branching point of the right Glisson’s pedicle and the dorsal portion of origin of the right hepatic vein[11,20].
According to the experience of the authors of this study, we did not observe any postoperative incidence of severe hemorrhage of the resection plane or hypoxic damage of the caudate lobe during hepatotomy along the pre-caudate plane for left lobectomy or extended right lobectomy of the liver.
This VHE method also permitted facilitated understanding of individual hilar bile duct anatomy, the openings of second order branches from the hilar bile duct by completely exposing the ventral hilar Glisson’s pedicle and then incising along the hilar bile duct. It also allowed increased accuracy of the intra-operative choledochoscopy, complete removal of intra-hepatic stones without difficulty under direct visualization, and easier stricture-plasty of the constricted hilar bile duct.
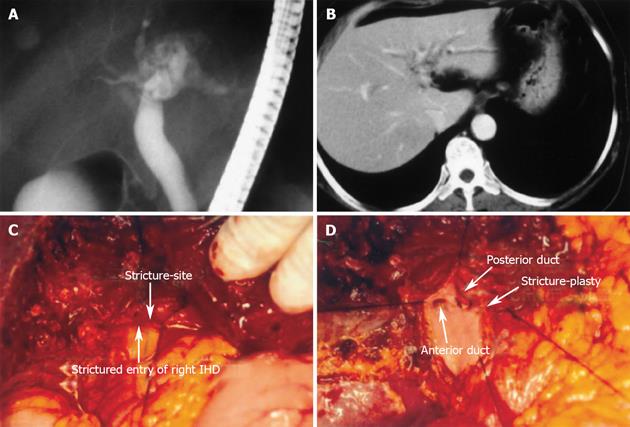
Our experience showed that the opening of hilar bile duct along its direction will allow visualization of 3 or 4 openings of the second order branches of the intra-hepatic bile duct, which emerge beginning from the right side in the following order; the anterior segmental branch, the posterior segmental branch (or common duct opening of right anterior and posterior hepatic duct), and 2 caudate branches. In many instances, the order and the number of caudate branches varied from patient to patient, and the order frequently presented as anterior segmental branch, caudate branch, posterior branch, and then the caudate branch. When hilar bile duct stricture is present, the stricture site may exist anywhere in the openings of the second order branches, thus necessitating adequate exposure of the hilar bile duct for direct visualization of the inside of the hilar bile duct for preservation of each second order branches during stricture-plasty (Figure 4).
Whenever possible, the authors did not perform a bilioenterostomy after hepatectomy but attempted to conserve the anatomy of the bile duct physiologically. This was because according to two studies by Kusano et al[21] and Jan et al[22], incidence of cholangitis was high after bilioenterostomy.
In this study, the 5.4% rate of residual stones and 4.2% of recurrent stones after VHE surgery for hepatolithiasis were much better results than historical control datas of conventional hepatectomy that showed residual stone rate about 10% and recurrent stone rate about 12-29.6%[22-25], and this may be attributed to the high efficacy of the VHE procedure in correcting the bile duct stricture. Moreover, as the patients who underwent VHE for hepatolithiasis in this study were all high grade Tsunoda type which is difficult to remove by endoscopic methods, the effectiveness of the proposed VHE method is further stressed. We also emphasize the complication rate of VHE which was comparable with that of conventional hepatectomy.
In conclusion, we present in this study the VHE method that allows accurate assessment of the pathologic anatomy of the intra-hepatic bile duct during hepatectomy for hepatolithiasis. We also suggest from our observed data that this procedure will decrease the residual stone rate and long term recurrent stone rate after surgery without serious complications. We recommend this procedure for surgical treatment of intractable hepatolithiasis.
S- Editor Guo SY L- Editor Elsevier HK E- Editor Kong LH
| 1. | Chen MF, Jan YY, Wang CS, Hwang TL, Jeng LB, Chen SC, Chen TJ. A reappraisal of cholangiocarcinoma in patient with hepatolithiasis. Cancer. 1993;71:2461-2465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Kubo S, Kinoshita H, Hirohashi K, Hamba H. Hepatolithiasis associated with cholangiocarcinoma. World J Surg. 1995;19:637-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 108] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Park YH, Park SJ, Jang JY, Ahn YJ, Park YC, Yoon YB, Kim SW. Changing patterns of gallstone disease in Korea. World J Surg. 2004;28:206-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Cetta F, Lombardo F, Cariati A. The role of the content (decreased level of apolipoprotein A1) and of the container (bile duct stricture, sectorial dilatation of the ducts determining bile stasis) in the pathogenesis of hepatolithiasis, either pigment or cholesterol. Hepatology. 1994;19:1539-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Nakanuma Y, Yamaguchi K, Ohta G, Terada T. Pathologic features of hepatolithiasis in Japan. Hum Pathol. 1988;19:1181-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 82] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Hwang JH, Yoon YB, Kim YT, Cheon JH, Jeong JB. Risk factors for recurrent cholangitis after initial hepatolithiasis treatment. J Clin Gastroenterol. 2004;38:364-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Maetani I, Ishiguro J, Ogawa S, Sato M, Igarashi Y, Sakai Y. Percutaneous choledochoscopic treatment of intrahepatic stones, including management of associated biliary stenoses. Endoscopy. 1999;31:456-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Uchiyama K, Onishi H, Tani M, Kinoshita H, Ueno M, Yamaue H. Indication and procedure for treatment of hepatolithiasis. Arch Surg. 2002;137:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Cheung MT, Wai SH, Kwok PC. Percutaneous transhepatic choledochoscopic removal of intrahepatic stones. Br J Surg. 2003;90:1409-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Tsunoda T, Tsuchiya R, Harada N, Yoshino R, Noda T, Izawa K, Yamaguchi T, Yamamoto K. Long-term results of surgical treatment for intrahepatic stones. Jpn J Surg. 1985;15:455-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 11. | Kwon D, Murakami G, Hata F, Wang HJ, Chung MS, Hirata K. Location of the ventral margin of the paracaval portion of the caudate lobe of the human liver with special reference to the configuration of hepatic portal vein branches. Clin Anat. 2002;15:387-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Sheen-Chen SM, Cheng YF, Chou FF, Lee TY. Ductal dilatation and stenting make routine hepatectomy unnecessary for left hepatolithiasis with intrahepatic biliary stricture. Surgery. 1995;117:32-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Hwang MH, Tsai CC, Mo LR, Yang CT, Yeh YH, Yau MP, Yueh SK. Percutaneous choledochoscopic biliary tract stone removal: experience in 645 consecutive patients. Eur J Radiol. 1993;17:184-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Cheng YF, Lee TY, Sheen-Chen SM, Huang TL, Chen TY. Treatment of complicated hepatolithiasis with intrahepatic biliary stricture by ductal dilatation and stenting: long-term results. World J Surg. 2000;24:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Su CH, Shyr YM, Lui WY, P'Eng FK. Hepatolithiasis associated with cholangiocarcinoma. Br J Surg. 1997;84:969-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 86] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Chijiiwa K, Ohtani K, Noshiro H, Yamasaki T, Shimizu S, Yamaguchi K, Tanaka M. Cholangiocellular carcinoma depending on the kind of intrahepatic calculi in patients with hepatolithiasis. Hepatogastroenterology. 2002;49:96-99. [PubMed] |
| 17. | Kim YT, Byun JS, Kim J, Jang YH, Lee WJ, Ryu JK, Kim SW, Yoon YB, Kim CY. Factors predicting concurrent cholangiocarcinomas associated with hepatolithiasis. Hepatogastroenterology. 2003;50:8-12. [PubMed] |
| 18. | Simon T, Fink AS, Zuckerman AM. Experience with percutaneous transhepatic cholangioscopy (PTCS) in the management of biliary tract disease. Surg Endosc. 1999;13:1199-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Kondo S, Nimura Y, Hayakawa N, Kamiya J, Nagino M, Miyachi M, Kanai M. A clinicopathologic study of primary cholesterol hepatolithiasis. Hepatogastroenterology. 1995;42:478-486. [PubMed] |
| 20. | Kitagawa S, Murakami G, Hata F, Hirata K. Configuration of the right portion of the caudate lobe with special reference to identification of its right margin. Clin Anat. 2000;13:321-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Kusano T, Isa TT, Muto Y, Otsubo M, Yasaka T, Furukawa M. Long-term results of hepaticojejunostomy for hepatolithiasis. Am Surg. 2001;67:442-446. [PubMed] |
| 22. | Jan YY, Chen MF, Wang CS, Jeng LB, Hwang TL, Chen SC. Surgical treatment of hepatolithiasis: long-term results. Surgery. 1996;120:509-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Sato M, Watanabe Y, Horiuchi S, Nakata Y, Sato N, Kashu Y, Kimura S. Long-term results of hepatic resection for hepatolithiasis. HPB Surg. 1995;9:37-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Chijiiwa K, Kameoka N, Komura M, Yamasaki T, Noshiro H, Nakano K. Hepatic resection for hepatolithiasis and long-term results. J Am Coll Surg. 1995;180:43-48. [PubMed] |
| 25. | Fan ST, Lai EC, Wong J. Hepatic resection for hepatolithiasis. Arch Surg. 1993;128:1070-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 54] [Article Influence: 1.7] [Reference Citation Analysis (0)] |