Published online Jul 28, 2006. doi: 10.3748/wjg.v12.i28.4593
Revised: April 12, 2006
Accepted: April 24, 2006
Published online: July 28, 2006
A 62-year-old man with progressive thickening of the gallbladder wall visited our outpatient clinic. The biliary amylase level in the common bile duct was 19 900 IU/L and that of the gallbladder was 127 000 IU/L, although endoscopic retrograde cholangiopancreatography revealed no pancreaticobiliary maljunction. Histology demonstrated a moderately differentiated adenocar-cinoma of the gallbladder. Pancreatobiliary reflux and associated gallbladder carcinoma were confirmed in the present case, in the absence of a pancreaticobiliary maljunction. Earlier detection of the pancreatobiliary reflux and progressive thickening of the gallbladder wall might have led to an earlier resection of the gallbladder and improved this patient’s poor prognosis.
- Citation: Sai JK, Suyama M, Kubokawa Y. A case of gallbladder carcinoma associated with pancreatobiliary reflux in the absence of a pancreaticobiliary maljunction: A hint for early diagnosis of gallbladder carcinoma. World J Gastroenterol 2006; 12(28): 4593-4595
- URL: https://www.wjgnet.com/1007-9327/full/v12/i28/4593.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i28.4593
Regurgitation of pancreatic juice into the biliary tract (pancreatobiliary reflux) usually occurs in patients with pancreaticobiliary maljunction and is closely related to the occurrence of biliary malignancy[1,2]. Bile mixed with pancreatic juice is known to induce cellular proliferation and stimulate genetic alterations of the biliary tract epithelium, leading to hyperplasia, dysplasia and ultimately, carcinoma of the biliary tract mucosa[3].
Here we describe a patient with pancreatobiliary reflux in the absence of pancreaticobiliary maljunction, who showed progressive thickening of the gallbladder wall, which developed into an advanced gallbladder carcinoma.
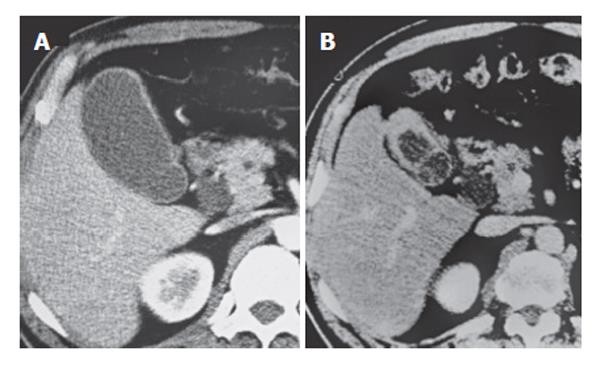
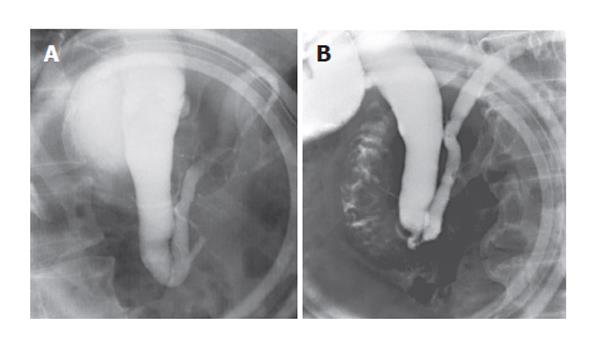
A 62-year-old man visited our outpatient clinic for further evaluation of diffuse thickening of the gallbladder wall, detected by ultrasonography, at an annual medical check-up. He had no symptoms, and the physical examination showed no abnormalities. Laboratory test results were within normal limits. The serum levels of carcinoembryonic antigen was 1.3 ng/mL and the carbohydrate antigen 19-9 level was 1.0 U/mL; that is, both were within normal limits. Computed tomography (CT) revealed diffuse thickening of the gallbladder wall and dilatation of the common bile duct to 12 mm (Figure 1A). The patient was followed, and CT was scheduled for 3 mo later. He returned 42 m later with persistent right hypochondralgia and slight tenderness in the right upper quadrant. Laboratory tests, including serum amylase and lipase, were within the normal range. The serum levels of carcinoembryonic antigen was up to 2.1 ng/mL and the carbohydrate antigen 19-9 level increased to 5.0 U/mL, but both were still within the normal limits. CT revealed progressive thickening of the gallbladder wall and carcinoma of the gallbladder was suspected (Figure 1B). Endoscopic retrograde cholangiopancreatography (ERCP) revealed no pancreaticobiliary maljunction, because the length of the common channel was 5 mm, sphincter of Oddi affected the pancreaticobiliary junction and a connection between two the ducts was not visible during the contraction phase of sphincter of Oddi
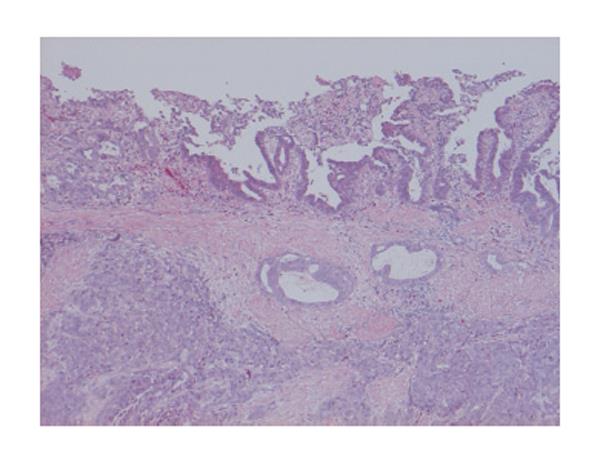
(Figure 2A, B). The biliary amylase level in the common bile duct, sampled during ERCP, was 19 900 IU/L. Extended cholecystectomy, bile duct resection, and lymph node dissection were performed. The amylase level in gallbladder bile, sampled during cholecystectomy, was 127 000 IU/L. Amylase was measured by an enzymatic method using the substrate 3-ketobutylidenβ-2-chloro-4-nitrophenyl-maltopentaoside (Diacolor Neonate; Toyobo, Osaka, Japan), and the normal range of serum amylase at our institution was 130-400 IU/L. The histopathologic diagnosis of the resected specimen was a moderately differentiated adenocarcinoma of the gallbladder’s fundus with invasion of the serosa (Figure 3).
Pancreaticobiliary maljunction is defined as an abnormal union of the pancreatic and biliary ducts that is located outside the duodenal wall, where a sphincter system is not present[1]. Thus, two ducts are always communicating, and pancreatic juice freely regurgitates into the biliary tract through this passage. Numerous clinical and experimental studies have supported a relationship between pancreatobiliary reflux and biliary cancer in patients with pancreaticobiliary maljunction. Bile mixed with pancreatic juice is known to induce hyperplasia, metaplasia, and ultimately, carcinoma of the biliary tract mucosa in patients with pancreaticobiliary maljunction[2,3]. In fact, biliary cancer is found in 15% to 67% of adult patients with pancreaticobiliary maljunction, and gallbladder carcinoma is found more often in patients with pancreaticobiliary maljunction without a congenital choledochal cyst[4,5].
Pancreatobiliary reflux also occurred in our patient, in the absence of a pancreaticobiliary maljunction that was confirmed by elevated amylase levels in the bile sampled at ERCP and cholecystectomy. It was suspected that the extremely high levels of pancreatic enzymes in the bile might have induced carcinoma of the gallbladder as seen in patients with pancreaticobiliary maljunction[4,5]. It was speculated that pancreatic juice may regurgitate into the biliary system through a common terminal ampulla that is known to exist in 60%-90% of human subjects[6]; as pressure generated in the pancreatic duct is usually greater than that observed in the biliary system, it allows for flow from the pancreas to the biliary system[7,8]. The precise mechanism of the pancreatobiliary reflux without pancreaticobiliary maljunction, and especially its relation to the dysfunction of sphincter of Oddi, should be further clarified.
One of the imaging findings that suggest mucosal changes accompanied by pancreatobiliary reflux is diffuse thickening of the gallbladder wall that might reflect cellular proliferation of the gallbladder epithelium, in patients with pancreaticobiliary maljunction[2]. In the present case, diffuse thickening of the gallbladder wall was confirmed on ultrasonography and CT, and its relation to pancreatobiliary reflux could be suggested.
In the present case, pancreatobiliary reflux and associated gallbladder carcinoma were confirmed, in the absence of pancreaticobiliary maljunction. Earlier detection of the pancreatobiliary reflux and progressive thickening of the gallbladder wall might have led to earlier resection of the gallbladder and improved this patient’s poor prognosis.
S- Editor Wang J L- Editor Lakatos PL E- Editor Liu Y
| 1. | The Japanese study group on pancreaticobiliary maljunction. Diagnostic criteria of pancreaticobiliary maljunction. J Hep Bil Panc Surg. 1994;1:219-221. [RCA] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 104] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Hanada K, Itoh M, Fujii K, Tsuchida A, Hirata M, Ishimaru S, Iwao T, Eguchi N, Kajiyama G. Pathology and cellular kinetics of gallbladder with an anomalous junction of the pancreaticobiliary duct. Am J Gastroenterol. 1996;91:1007-1011. [PubMed] |
| 3. | Tanno S, Obara T, Fujii T, Mizukami Y, Shudo R, Nishino N, Ura H, Klein-Szanto AJ, Kohgo Y. Proliferative potential and K-ras mutation in epithelial hyperplasia of the gallbladder in patients with anomalous pancreaticobiliary ductal union. Cancer. 1998;83:267-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Kimura K, Ohto M, Saisho H, Unozawa T, Tsuchiya Y, Morita M, Ebara M, Matsutani S, Okuda K. Association of gallbladder carcinoma and anomalous pancreaticobiliary ductal union. Gastroenterology. 1985;89:1258-1265. [PubMed] |
| 5. | Yamauchi S, Koga A, Matsumoto S, Tanaka M, Nakayama F. Anomalous junction of pancreaticobiliary duct without congenital choledochal cyst: a possible risk factor for gallbladder cancer. Am J Gastroenterol. 1987;82:20-24. [PubMed] |
| 6. | Hjorth E. Contributions to the knowledge of pancreatic reflux as a factor in chronic affections of the gallbladder. Acta Chir Scand. 1947;96:12-29. |
| 7. | Menguy RB, Hallenbeck GA, Bollman JL, Grindlay JH. Intraductal pressures and sphincteric resistance in canine pancreatic and biliary ducts after various stimuli. Surg Gynecol Obstet. 1958;106:306-320. [PubMed] |
| 8. | Anderson MC, Hagstrom WJ Jr. A comparison of pancreatic and biliary pressures recorded simultaneously in man. Can J Surg. 1962;5:461-470. [PubMed] |