Published online Jul 14, 2006. doi: 10.3748/wjg.v12.i26.4264
Revised: March 16, 2006
Accepted: March 27, 2006
Published online: July 14, 2006
Splenic arteriovenous fistula (SAVF) accounts for an unusual but well-documented treatable cause of portal hypertension[1-4]. A case of a 50-year-old multiparous female who developed suddenly portal hypertension due to SAVF formation is presented. The patient suffered from repeated episodes of haematemesis and melaena during the past twelve days and thus was emergently admitted to hospital for management. Clinical and laboratory investigations established the diagnosis of portal hypertension in the absence of liver parenchymal disease. Endoscopy revealed multiple esophageal bleeding varices. Abdominal computed tomography (CT) and transfemoral celiac arteriography documented the presence of a tortuous and aneurysmatic splenic artery and premature filling of an enlarged splenic vein, findings highly suggestive of an SAVF. The aforementioned vascular abnormality was successfully treated with percutaneous transcatheter embolization. Neither recurrence nor other complications were observed.
- Citation: Siablis D, Papathanassiou ZG, Karnabatidis D, Christeas N, Katsanos K, Vagianos C. Splenic arteriovenous fistula and sudden onset of portal hypertension as complications of a ruptured splenic artery aneurysm: Successful treatment with transcatheter arterial embolization. A case study and review of the literature. World J Gastroenterol 2006; 12(26): 4264-4266
- URL: https://www.wjgnet.com/1007-9327/full/v12/i26/4264.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i26.4264
Splenic arteriovenous fistulas (SAVF) represent a rare pathological entity that should be suspected especially in cases of acute portal hypertension not related to chronic liver disease[1-4]. They may be either asymptomatic or lead rapidly to the development of portal hypertension, with a clinical picture of gastro-intestinal bleeding, diarrhea, ascites or unfavorable heart failure due to hyperdynamic blood flow state[1-4].
In this report an uncommon case of portal hypertension affecting a multiparous female is discussed. Rupture of a splenic artery aneurysm (SAA) into the splenic vein and formation of a fistulous tract between them consist the underlying pathology. The authors emphasize the positive impact of transcatheter arterial embolization as an effective alternative to surgical intervention in the management of such vascular malformations.
A 50-year-old female was referred to our institution for management of an intermittent but intense epigastric pain and a feeling of gastric fullness that were associated with repeated episodes of haematemesis and melaena during the past twelve days. No history of abdominal (accidental or iatrogenic) trauma was reported. On the other hand, it was notable the fact that the patient had delivered successfully four labors between the ages of 26-40 years old.
Upon admission the patient’s abdomen was distended and tender. The liver was not palpable and no signs of jaundice were observed. Abdominal auscultation revealed a systolic bruit located at the left flank. Ascites was also depicted. Full blood cell count exhibited markedly decreased values of hematocrit and hemoglobin. Coagulation studies and liver and renal function tests were not affected. Serological markers of hepatitis A, B, C, D were negative and no antibodies were detected. Urgent endoscopy showed multiple bleeding esophageal varices. The stomach was found full of blood and the gastric mucosa was red irritated and edematous; findings consistent with mild portal gastritis. The endoscopic variceal ligation that immediately followed only controlled the bleeding temporarily.
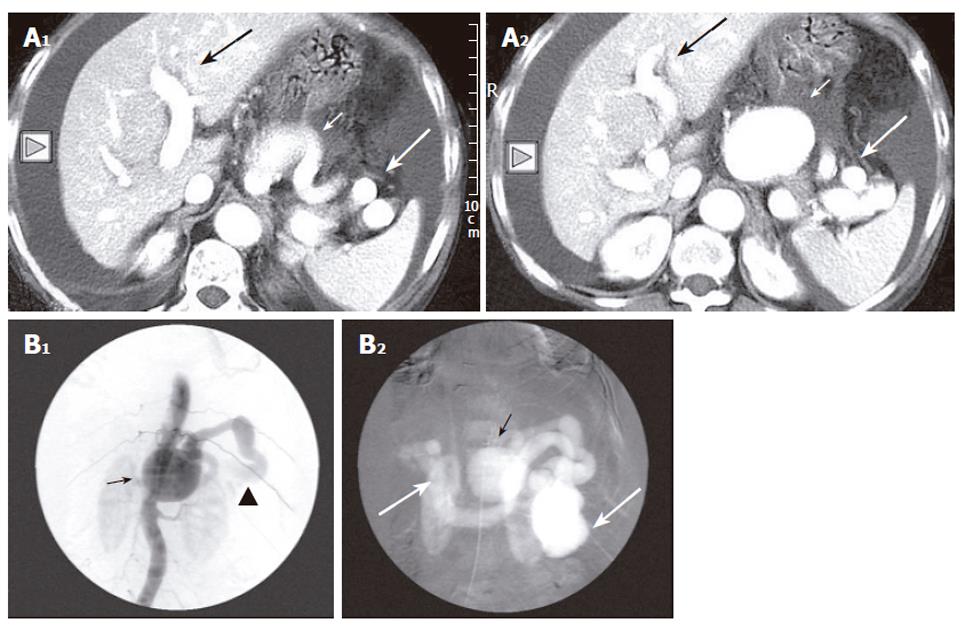
Contrast enhanced CT scan of the upper abdomen demonstrated an aneurysmal dilated tortuous splenic artery of maximum diameter of 52 mm, an engorged splenic vein along with simultaneous opacification of the splenic vessels as well during the arterial phase (Figure 1A). Ascites was also confirmed. The aforementioned imaging features strongly supported the case of an SAA that was connected to the splenic vein through a fistula and caused an abrupt elevation of the portal pressure. Celiac and splenic arteriographies were carried out and showed a dilated splenic artery with a large aneurysm combined with premature portal and splenic vein filling and marked opacification of the splenoportal axis (Figure 1B).
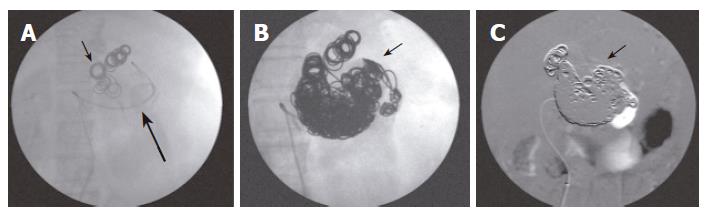
The patient’s condition remained unstable due to continuing bleeding and transcatheter embolization was scheduled. By using the transfemoral route the aneurysmal sac was accessed and subsequently detachment of adequate metallic macrocoils was performed resulting thus in full occlusion of the sac, cessation of the hyperkinetic portal flow and successful control of the gastro-intestinal bleeding (Figure 2).
The patient had an uncomplicated recovery and was discharged eight days later in stable clinical condition. At the time of this writing, 10 mo later the patient remains free of symptoms with no evidence of post-procedural recurrence or complications.
SAA was first described by Beaussier in 1770[5]. According to autopsy studies its prevalence ranges from 0.01% to 10.4%. SAAs are found incidentally on 0.78% of angiograms and in 7.1% of patients with cirrhotic portal hypertension[6]. Splenic artery accounts for the third most common abdominal vessel site that is affected by the aneurysmal disease after infra-renal aorta and iliac artery[7,8].
Splenic artery aneurysm formation relies upon structural incompetence of the connective tissue of the arterial wall to secure the integrity of the vessel lumen[5,6,8]. Associated risk factors include portal hypertension, connective tissue disorders, congenital abnormalities, trauma and infection[6]. Unlike other true visceral aneurysms atherosclerosis does not play a leading role in splenic artery aneurysmal dilatation. They are most commonly encountered among females (female to male ratio: 4/1) especially the multipara[6].
It has been postulated that increased visceral blood flow and gestational hormones during pregnancy alter pathologically the structure of the arterial wall by causing fragmentation of the elastic fibers of the media and loss of smooth muscle[6,8]. As parity increases these factors have a cumulative effect predisposing thus to aneurysmal formation[6]. Hence, the fact that this patient had four successful pregnancies can justify the progressive growth of a splenic artery aneurysm.
Splenic artery aneurysm may present as an incidental finding on imaging modalities or with abdominal pain[6]. It has been also reported a lifetime risk of rupture of 2%-10% with an associated mortality of 25%[9]. These rates increase remarkably among pregnant women whereas the estimated risk of rupture can reach up to 50% with related maternal and fetal mortality of 70% and 90% respectively[6]. The rupture may take place either into the gastrointestinal tract and peritoneal cavity or into the splenic vein resulting in splenic arteriovenous fistula development.
Splenic arteriovenous fistulas represent an unusual clinical entity that was first reported by Wiegert in the 19th century[1-4]. Their majority occurs more commonly after rupture of an SAA into the corresponding vein but their origin can be congenital, traumatic (iatrogenic or accidental) or even infectious[1-4].
Despite the fact that SAVFs may stay free of symptoms for a long period of time, the hemodynamic changes that develop owing to the arteriovenous shunt may lead to a sudden increase of portal vein pressure. In contrast, chronic liver disease follows a more time-consuming process before ending in portal hypertension[1].
The clinical profile of splenic arteriovenous fistula mainly consists of upper abdominal pain, gastro-intestinal bleeding and secretory diarrhea[1-4]. These features are attributed to the abrupt increase of the mesenteric venous pressure[1,3]. An abdominal bruit, usually of the “machinery” type, is often heard over the left flank[1,3,4] and although its presence can raise a high index of clinical suspicion, it is encountered only in 30% of cases[4].
Although abdominal ultrasound combined with the Color Doppler technology can document blood flow abnormalities, splenomegaly and exclude liver parenchymal disease, the established imaging modality in detecting SAVFs is selective celiac or splenic arteriography. The method localizes with accuracy the vascular abnormality and contributes greatly in the assessment of collateral flow pathways[10]. It is mostly recommended in cases with sudden onset of portal hypertension, abdominal bruit and absence of chronic liver disease[4]. The patient’s medical history should be always taken into account.
On the basis of a well-established diagnosis immediate intervention is rendered mandatory in order to avoid unfavorable complications that will adversely affect prognosis. Splenic artery aneurysms should be promptly treated in high risk patients with symptomatic or expanding aneurysms, women of childbearing age and also patients undergoing liver transplantation[5,11].
Traditionally surgical and or laparoscopic resection with or without splenectomy is employed in the treatment of SAAs[5-7,9-12]. However, this patient carried a substantial surgical risk owing to the continuing variceal bleeding and the high possibility of aneurysmal rupture, during surgery, due to its size and the elevated pressure in the splenoportal axis. In addition, surgical approach of SAVFs presents often with technical difficulties and potential hazards of failure because of the distal site of the lesion and the formation of adhesions and numerous portal collaterals[4]. As a result, endovascular techniques emerged as an alternative option. Aneurysmal exclusion using a stent graft was not considered as a feasible solution mostly due to the presence of the fistula and the tortuosity of the splenic artery. In this case successful control of the variceal bleeding and cessation of the hyperkinetic blood flow in the splenoportal axis were achieved by selective catheterization of the sac and detachment of adequate metallic coils that promote permanent thrombosis. Unlike surgical techniques transcatheter arterial embolization is a less invasive, relatively low-risk, rapid procedure that can be easily applied regardless of the location of the vascular malformation[4,12]. It does not necessitate splenectomy avoiding thus immunologic deficits and a lifelong risk of sepsis[13]. The aforementioned advantages of transcatheter arterial embolization over surgery support strongly its efficacy in treating safely patients with splenic artery aneurysm complicated with arteriovenous fistula[4,12,13].
S- Editor Wang J L- Editor Zhu LH E- Editor Bai SH
| 1. | Strassburg CP, Bleck JS, Rosenthal H, Meyer HJ, Gebel M, Manns MP. Diarrhea, massive ascites, and portal hypertension: rare case of a splenic arterio-venous fistula. Z Gastroenterol. 1996;34:243-249. [PubMed] |
| 2. | Galler G, Yim A, Emond JC, Kirch E, Yousefzadeh D, Baker AL. Splenic arteriovenous fistula. A rare lesion causing bleeding esophageal varices, ascites, and diarrhea. Dig Dis Sci. 1996;41:816-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | McClary RD, Finelli DS, Croker B, Davis GL. Portal hypertension secondary to a spontaneous splenic arteriovenous fistula: case report and review of the literature. Am J Gastroenterol. 1986;81:572-575. [PubMed] |
| 4. | Hung CF, Tseng JH, Lui KW, Wan YL, Tsai CC, Shem CH, Wu CS. Intractable oesophageal variceal bleeding caused by splenic arteriovenous fistula: treatment by transcatheter arterial embolization. Postgrad Med J. 1999;75:355-357. [PubMed] |
| 5. | Mattar SG, Lumsden AB. The management of splenic artery aneurysms: experience with 23 cases. Am J Surg. 1995;169:580-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 149] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Selo-Ojeme DO, Welch CC. Review: spontaneous rupture of splenic artery aneurysm in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2003;109:124-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 84] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Pulli R, Innocenti AA, Barbanti E, Dorigo W, Turini F, Gatti M, Pratesi C. Early and long-term results of surgical treatment of splenic artery aneurysms. Am J Surg. 2001;182:520-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Cressey D, Reid MF. Splenic artery aneurysm rupture in pregnancy. Int J Obstet Anesth. 1996;5:103-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Kasir D, Macierewicz J, Castillo-Rama M, Singh S, Mackinlay J. Stent-graft repair of proximal splenic artery aneurysm. Eur J Vasc Endovasc Surg. 2003;6:62-63. |
| 10. | de Perrot M, Bühler L, Deléaval J, Borisch B, Mentha G, Morel P. Management of true aneurysms of the splenic artery. Am J Surg. 1998;175:466-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Schmittling ZC, McLafferty R. Transcatheter embolization of a splenic artery aneurysm. J Vasc Surg. 2004;40:1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Kakizawa H, Toyota N, Naito A, Fukuda H, Ito K. Super-selective transcatheter arterial embolization of a traumatic splenic arteriovenous fistula. Radiat Med. 2004;22:364-367. [PubMed] |
| 13. | Maloo MK, Burrows PE, Shamberger RC. Traumatic splenic arteriovenous fistula: splenic conservation by embolization. J Trauma. 1999;47:173-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |