Published online Jul 7, 2006. doi: 10.3748/wjg.v12.i25.4109
Revised: January 7, 2006
Accepted: January 14, 2006
Published online: July 7, 2006
A middle aged, non-addict male presented with right upper abdominal pain and swelling with respiratory distress. Examination revealed central cyanosis, bipedal pitting edema with prominent epigastric and back veins. Liver was enlarged, tender, spanned 20 cm without any splenomegaly or ascites. Other systems were clinically normal. Laboratory investigations showed polymorphonuclear leucocytosis with slightly deranged liver function. Abdominal ultrasonography showed an abscess in the right lobe of the liver with compressed inferior vena cava (IVC), middle and left hepatic veins. Arterial blood gas (ABG) documented hypoxia with orthodeoxia and air-contrast echocardiography was suggestive of an intrapulmonary shunt. A diagnosis of hepato-pulmonary syndrome (HPS) was made with near normal liver function secondary to amebic liver abscess. It reversed completely following successful treatment of the liver abscess.
- Citation: Mandal SK, Chakraborty PP, Bhattacharjee R, Chowdhury SR, Majumdar S. An unusual cause of dyspnoea complicating right upper abdominal swelling. World J Gastroenterol 2006; 12(25): 4109-4111
- URL: https://www.wjgnet.com/1007-9327/full/v12/i25/4109.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i25.4109
Hepato-pulmonary syndrome (HPS) is a dreaded complication of liver disease. It consists of the triad of hepatic dysfunction and/or portal hypertension, intrapulmonary vascular dilatation, and gas exchange abnormalities (PaO2 < 70 mmHg or alveolo-arterial gradient > 20 mmHg). HPS occurs mostly in cirrhotic patients but it has also been reported in cases of non-cirrhotic portal hypertension with minimal hepatic dysfunction. Liver transplantation is the only therapeutic option of proven benefit. We present a case where a large amebic liver abscess gave rise to transient portal hypertension due to Budd-Chiari Syndrome (BCS). The hemodynamic alteration led to development of HPS with minimal hepatic dysfunction and it reversed completely after successful treatment of the abscess.
A 38-year old non-addict male presented with right upper abdominal pain and progressively increasing right upper quadrant swelling for the last 3 mo. Along with it he also noticed swelling of both feet for 2 mo and respiratory distress for last 7 d. The abdominal pain was dull aching in character. There was no definite history of radiation or any aggravating or relieving factors. The patient denied any history of nausea, vomiting, and altered bladder or bowel habits. The bipedal edema was not associated with any facial puffiness, palpitation, chest pain or oliguria. His respiratory distress was progressively increasing and was not relieved on upright posture. He also noticed yellowish discoloration of his eyes and urine along with occasional low grade fever and weight loss. His past, personal and family history was non-contributory.
General examination revealed mild pallor, icterus, and bipedal pitting edema along with the presence of central cyanosis. The patient was febrile (oral temperature 39.2°C) with a respiratory rate of 28/min.The umbilicus was central, inverted with a single prominent epigastric and back vein. The venous flow was below upwards. Liver was enlarged, firm and tender with a sharp margin and smooth surface. The hepatic span was 20 cm and there was no audible bruit or rub. He did not have splenomegaly or ascites. The chest was dull on percussion below 4th intercostal space (ICS) along midclavicular line (MCL), below 6th ICS along midaxillary line (MAL) and below 8th ICS along infrascapular region on the right side, without any mediastinal shift. Auscultation revealed diminished breath sounds with diminished vocal resonance over the above region without any added sounds.
Examination of the other systems was within normal limits.
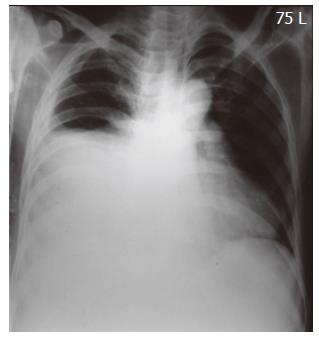
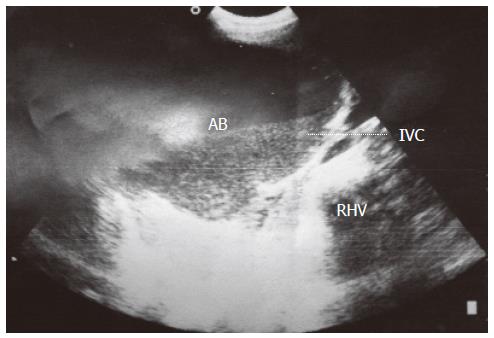
A complete blood count showed hemoglobin 11.5 mg% and total leucocyte count of 11 200/cmm with polymorphonuclear leucocytosis. The liver function test revealed bilirubin of 4.5 mg/dL (direct: 3.1 mg/dL), AST: 65 U/L, ALT: 70 U/L, ALP: 350 U/L, protein: 7.1 g/dL (Alb: 3.7 mg/dL), P-time: 15.8 s (control 13 s); other biochemical parameters were unremarkable. Chest X-ray was normal except for an elevated right dome of diaphragm (Figure 1). Ultrasonography of the abdomen unmasked an abscess in right lobe of liver (13 cm × 14 cm), with mild ascites. The portal vein was 15.5 mm with normal splenic size. The IVC was compressed and the middle and left hepatic veins were not visualized (Figure 2). Doppler study showed absent phasic variation in above veins.
The viral markers were negative and an upper GI endoscopy was unrevealing. Bacterial culture of the anchovy sauce pus on CT guided aspiration was negative.
Arterial blood gas analysis was performed with the patient both in supine position and after standing upright for 5 min. It showed hypoxemia with orthodeoxia, along with an increased alveolo-arterial gradient [Supine PaO2: 70 mmHg; Standing PaO2 (after 5 min): 59 mmHg; Standing A-a O2 gradient: 46 mmHg]. The hypoxia was partially corrected on 100% oxygen inhalation.
We performed an air contrast echocardiography. Ten milliliters of normal saline were agitated in two 10-mL syringes connected through a 3-way stopcock, and it was then injected through a 20 gauge right superior extremity intravenous line. Micro bubbles were detected immediately in the right sided cardiac chambers on apical 4-chamber view of 2-dimensional transthoracic echocardiography. Delayed visualization of micro bubbles in the left heart chamber (i.e., after 3 cardiac contractions following visualization of micro bubbles in the right heart chamber) was suggestive of intrapulmonary “right to left” shunting. Normally no bubbles should be detected in the left heart chambers even after 3 injections of agitated normal saline. If it is visible within 3 cardiac contractions it suggests intracardiac shunting. In our case micro bubbles were visible in the left heart chambers after 5 cardiac contractions. Chest radiography, electrocardiography, and echocardiography were performed to exclude primary pulmonary or cardiac pathology.
Hence, we diagnosed it as a case of HPS occurring as a rare complication of amoebic liver abscess due to transient portal hypertension with near normal liver function. The patient was put on tube drainage with intravenous metronidazole. The pig-tail catheter was removed after the drainage volume decreased and the IVC was fully decompressed. A repeat ABG after 8 wk showed normalization of both hypoxia and orthodeoxia (Supine PaO2: 94 mmHg, Standing PaO2: 91 mmHg, Standing A-a O2 gradient: 9 mmHg).
Amebic liver abscess is common in this part of the world. Development of BCS due to amebic liver abscess though uncommon, has been previously reported[1,2]. HPS is a specific entity identified in the recent past. Although many data have emerged, questions remain unanswered regarding its natural history and pathogenesis. Hepatic dysfunction appears to be the usual setting in which it occurs. Prevalence of HPS in cirrhotic patients ranges from 5% to 29%[3,4]. However, there have been anecdotal reports of HPS in patients with portal hypertension, without evidence of hepatic dysfunction (e.g., congenital hepatic fibrosis[5], nodular hyperplasia[6], Budd-Chiari syndrome[7]). HPS also has been reported in cases of non-cirrhotic portal hypertension[8], where hepatocellular dysfunction is minimal.
In our case hepatic dysfunction was minimal but transient portal hypertension was evidenced by prominent epigastric vein and ultrasonographic documentation of dilated portal vein (15.5 mm). Development of HPS in this short period (3 mo) is unusual but has been reported[2]. Portal hypertension plays an important role in the pathogenesis of HPS, probably by increased NO production[9]. Hemodynamic alteration in BCS leads to increased sinusoidal pressure and increased shear stress. The activation of NO release, by shear stress, from endothelial cells through a specific G protein-mediated signaling pathway may be an important factor[10]. HPS can be reversed by cavoplasty in cases of BCS due to inferior vena cava obstruction[2]. In our case decompression of IVC by drainage of the abscess led to the reversal of HPS. Thus, the above mentioned mechanisms might form the basis of development of intrapulmonary vascular dilatation as a result of elevated portal pressure, irrespective of the associated hepatic functional status.
S- Editor Wang J L- Editor Zhu LH E- Editor Bi L
| 1. | Dilawari JB, Bambery P, Chawla Y, Kaur U, Bhusnurmath SR, Malhotra HS, Sood GK, Mitra SK, Khanna SK, Walia BS. Hepatic outflow obstruction (Budd-Chiari syndrome). Experience with 177 patients and a review of the literature. Medicine (Baltimore). 1994;73:21-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 215] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | De BK, Sen S, Biswas PK, Mandal SK, Das D, Das U, Guru S, Bandyopadhyay K. Occurrence of hepatopulmonary syndrome in Budd-Chiari syndrome and the role of venous decompression. Gastroenterology. 2002;122:897-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Krowka MJ, Tajik AJ, Dickson ER, Wiesner RH, Cortese DA. Intrapulmonary vascular dilatations (IPVD) in liver transplant candidates. Screening by two-dimensional contrast-enhanced echocardiography. Chest. 1990;97:1165-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 137] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Stoller JK, Moodie D, Schiavone WA, Vogt D, Broughan T, Winkelman E, Rehm PK, Carey WD. Reduction of intrapulmonary shunt and resolution of digital clubbing associated with primary biliary cirrhosis after liver transplantation. Hepatology. 1990;11:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 98] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Maggiore G, Borgna-Pignatti C, Marni E, Abbati G, Magrini U. Pulmonary arteriovenous fistulas: an unusual complication of congenital hepatic fibrosis. J Pediatr Gastroenterol Nutr. 1983;2:183-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Abrams GA, Fallon MB. The hepatopulmonary syndrome. Clin Liver Dis. 1997;1:185-200, xiii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | De BK, Sen S, Biswas PK, Sanyal R, Majumdar D, Biswas J. Hepatopulmonary syndrome in inferior vena cava obstruction responding to cavoplasty. Gastroenterology. 2000;118:192-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | al-Moamary M, Altraif I. Hepatopulmonary syndrome associated with schistosomal liver disease. Can J Gastroenterol. 1997;11:449-450. [PubMed] |
| 9. | Selim KM, Akriviadis EA, Zuckerman E, Chen D, Reynolds TB. Transjugular intrahepatic portosystemic shunt: a successful treatment for hepatopulmonary syndrome. Am J Gastroenterol. 1998;93:455-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Kuchan MJ, Jo H, Frangos JA. Role of G proteins in shear stress-mediated nitric oxide production by endothelial cells. Am J Physiol. 1994;267:C753-C758. [PubMed] |