Published online Jul 7, 2006. doi: 10.3748/wjg.v12.i25.4089
Revised: January 5, 2006
Accepted: January 14, 2006
Published online: July 7, 2006
Acute liver failure (ALF) is a medical emergency requiring immediate evaluation for liver transplantation. We describe an unusual case of a patient who presented with ascites, jaundice, and encephalopathy and was found to have ALF due to natural killer (NK)-like T cell leukemia/lymphoma. The key immunophenotype was CD2+, CD3+, CD7+, CD56+. This diagnosis, which was based on findings in the peripheral blood and ascitic fluid, was confirmed with liver biopsy, and was a contraindication to liver transplantation. A review of the literature shows that hematologic malignancies are an uncommon cause of fulminant hepatic failure, and that NK-like T-cell leukemia/lymphoma is a relatively recently recognized entity which is characteristically CD3+ and CD56+. This case demonstrates that liver biopsy is essential in diagnosing unusual causes of acute liver failure, and that infiltration of the liver with NK-like T-cell lymphoma/leukemia can cause acute liver failure.
- Citation: Dellon ES, Morris SR, Tang W, Dunphy CH, Russo MW. Acute liver failure due to natural killer-like T-cell leukemia/lymphoma: A case report and review of the Literature. World J Gastroenterol 2006; 12(25): 4089-4092
- URL: https://www.wjgnet.com/1007-9327/full/v12/i25/4089.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i25.4089
Acute liver failure (ALF) is a medical emergency, and while liver transplantation can be life saving, it is imperative to perform a thorough evaluation to screen for potential contraindications[1]. We describe an unusual case of a patient who developed ALF due to natural killer (NK)-like T-cell leukemia/lymphoma, a diagnosis with important implications, as it is a contraindication to liver transplantation. While a review of the literature shows that previously published case series have found this rare sub-type of T-cell malignancy to involve the liver, we believe that this is the first report of it presenting as ALF.
A previously healthy 63 year-old man was admitted for three mo of fatigue, one mo of increasing abdominal girth and peripheral edema, two weeks of jaundice, and one week of confusion. He noted recent fevers, anorexia, weight loss, and day-night reversal. He had never received a blood transfusion or used intravenous or intranasal drugs. He had no tattoos or recent travel. He did not take prescription or over-the-counter medications, or nutritional or herbal supplements. He admitted using alcohol heavily in the past, but had been sober for more than 10 years. His family corroborated this information. There was no family history of liver disease.
On physical examination he was jaundiced and had findings consistent with hepatic encephalopathy including slurred speech and asterixis. He had moderate ascites, peripheral edema, and scattered spider angiomata. The liver was normal in size, but splenomegaly was detected.
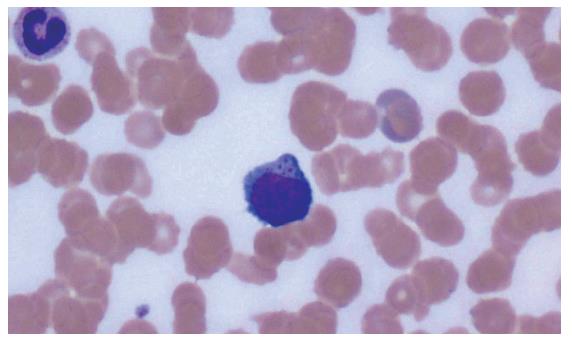
Routine laboratory tests revealed hyponatremia, hypoalbuminemia, hyperbilirubinemia, thrombocytopenia, and prolonged prothrombin time not due to vitamin K deficiency (Table 1). The white blood cell count was 5.1 × 109/L with atypical lymphocytes comprising 53% of the differential (Figure 1). Other diagnostic testing found a negative toxicology screen, 90% iron saturation, negative serologies for hepatis A virus, hepatitis B virus, hepatitis C virus, human immunodeficiency virus, and human T-cell lymphotrophic virus (HTLV) types I and II. Serologies were also negative for anti-nuclear antibodies, anti-smooth muscle antibodies, and anti-mitochondrial antibodies. Serum protein electrophoresis, alpha-1 anti-trypsin levels, ceruloplasmin levels, and alpha-fetoprotein were normal. Serum ammonia level was not measured. Abdominal ultrasound showed a normal liver size with heterogeneous echotexture, splenomegaly, and patent vasculature. Head CT scan excluded mass lesions and infiltrating disease.
| Test | Result (normal range) |
| Sodium | 128 mmol/L (135-145) |
| Creatinine | 1.1 mg/dL (0.8-1.4) |
| AST (SGOT) | 85 U/L (19-55) |
| ALT (SGPT) | 40 U/L (19-72) |
| Total bilirubin | 8.4 mg/dL (0.0-1.2) |
| Direct bilirubin | 7.1 mg/dL (0.0-0.4) |
| Alkaline phosphatase | 138 U/L (38-126) |
| GGT | 80 U/L (13-68) |
| Serum albumin | 1.7 g/dL (3.5-5.0) |
| Ascitic fluid albumin | 0.5 g/dL (unspec) |
| White blood cell count | 5.1 × 109/L (4.5-11) |
| neutrophils (%) | 47 |
| monocytes (%) | 0 |
| lymphocytes (%) | 53 with atypical forms present |
| eosinophils (%) | 0 |
| Hematocrit (%) | 33.3 (41-53) |
| Platelet count | 31 × 109/L (150-440) |
| Prothrombin time | 20 s (11-14) |
| International normalized ratio (INR) | 1.7 |
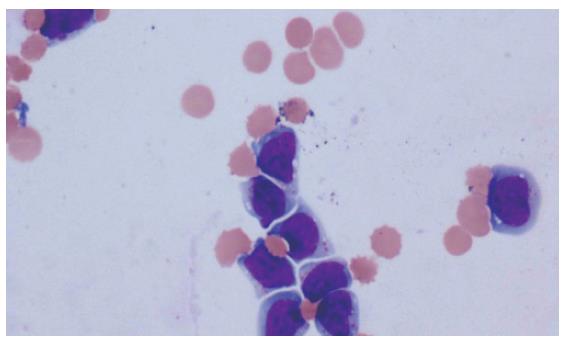
Diagnostic paracentesis at a site in the left-lower-quadrant demonstrated a serum albumin-ascites gradient of 12 g/L, 12 475 red blood cells (RBCs)/mm3 and 1875 white blood cells (WBCs)/mm3 with a differential of 1% neutrophils, 4% monocytes and 95% lymphocytes. Because the lymphocytes were described as atypical with mitotic figures, a repeat paracentesis was performed at a right-lower-quadrant site. This revealed 1550 RBCs/mm3 and 250 WBCs/mm3 with the same differential and atypical cells. A sample of the ascitic fluid was sent for cytology (Figure 2). The peripheral blood flow cytometric immunophenotypes were as follows: CD2+, CD3+, CD7+, CD56+, CD4-, CD5-, CD8-, CD57-, and CD16-. A bone marrow biopsy revealed the same findings. Cytogenetic analysis of the bone marrow aspirate revealed the following karyotypes: 43, X, -Y, add (4) (q35), -5, dic (6;19) (q23; q13.4), -10, -11, -13, -14, -16, -18, add(22)(p11), +6 mars.
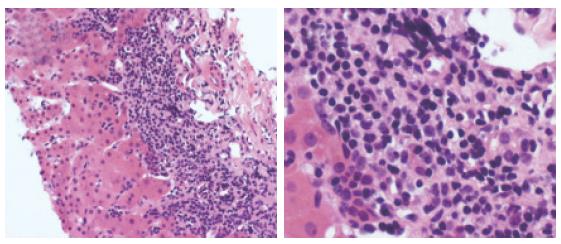
Since the patient’s coagulopathy prohibited percutaneous liver biopsy, transjugular liver biopsy was performed for definitive diagnosis. There was no evidence of cirrhosis, but there was diffuse hepatic infiltration by a malignant lymphoid population (Figures 3A and 3B) which was immunohistochemically stained as follows: CD3+, CD20-, Epstein-Barr virus (EBV)-, granzyme B+, T1A-1+, and TdT-. The paraffin block of the liver biopsy was analyzed for a T-cell receptor (TCR) gamma gene rearrangement by polymerase chain reaction, and there was no evidence of a clonal TCR gamma gene rearrangement.
The patient was diagnosed with NK-like T-cell lymphoma/leukemia as the cause of liver failure on hospital d 4. This was deemed a contraindication to transplantation. His course was complicated on d 3 by bleeding duodenal ulcers amenable to standard endoscopic treatment. On d 4-6, high-dose methylprednisolone failed to induce remission, and his hepatic synthetic function and mental status worsened. On d 10 and 11, a salvage regimen of gemcitabine was unsuccessful in inducing remission. On d 12, neutropenia, fever, and hypotension developed, and the patient’s jaundice and encephalopathy progressed. The patient expired on hospital d 12.
The diagnosis of acute liver failure is a medical emergency because mortality is high without liver transplantation[1]. However, thorough evaluation is mandatory to exclude contraindications to liver transplantation such as underlying malignancy[1,2].
Hematologic malignancies often incidentally involve the liver, but they uncommonly present as acute liver failure[3,4]. When they do so, however, they carry a poor prognosis[5]. Acute leukemias, Hodgkin’s disease, non-Hodgkin’s lymphoma, and transformation of chronic leukemias have all been noted in case reports or case series to present as hepatic failure[5-20]. Infiltration of the liver and subsequent hepatic dysfunction specifically by T-cell leukemias and lymphomas are more unusual, though it has been reported in both the pediatric[21,22] and adult patients[23-29].
Natural killer cells, typically identified morphologically as large granular lymphocytes, are recognized for their role in cell-mediated immunity[30]. They have characteristic immunophenotypes (CD3-, CD56+) which distinguish them from T cells (CD3+, CD56-). Other markers such as CD8 and the additional so-called NK-cell antigens (CD16 and CD57) are variably present[31-32]. Over the past two decades, it has been noted that NK cells undergo clonal expansion and malignant transformation[33]. This is believed to be a rare event, accounting for only a small fraction of all T-cell malignancies, which themselves are thought to comprise approximately just 15% of all non-Hodgkin’s lymphoma[31,34]. NK-cell leukemia/lymphomas are categorized as either immature (and more aggressive) or mature (with an indolent course), and more commonly affect the nasopharynx and sinuses though they have also been reported to involve the skin, mucosa of the gastrointestinal (GI) tract, testes, kidneys, and orbit[31,35]. They are seen more frequently in Asia, Mexico, and South America, ostensibly due to associations with EBV and HTLV[36-38]. Of note, while they are commonly associated with hepatosplenomegaly they have not been reported to present with acute liver failure [31,39-41].
In contrast to NK cells, NK-like T-cells expressing features of both T cells and NK cells, are defined by a CD3+, CD56+ immunophenotypes, and tend not to be associated with EBV[31]. The first reports of NK-like T-cell leukemias and lymphomas[42,43] have described presentations including typical “B” symptoms such as fever, chills, night sweats and weight loss, as well as lymphadenopathy and splenomegaly. Disease involves the spleen, blood, marrow, GI tract, lung, kidneys, and liver, but none of the patients presented with frank liver dysfunction. In most instances, the disease is aggressive and rapidly fatal, regardless of treatment regimen. A large series identified 49 Chinese patients with extra-nasal CD56+ disease, 34 of whom are also CD3+[38]. Of the 5 patients with liver involvement, all had reactive hemophagocytic syndrome but none presented with hepatic failure. Of the 29 patients with follow-up information available, 24 died in a median time of 3.5 mo. A recent phenotypic analysis of 408 Japanese cases of peripheral T/NK cell lymphoma had not described any with liver failure[44].
In this paper we present the clinical course, immunophenotype, and cytogenetics of what we believe to be the first reported case of a patient with acute liver failure due to NK-like T-cell leukemia/lymphoma. This has implications beyond the rarity of this particular patient’s condition. Because this patient had a history of alcohol consumption, his liver disease might have been ascribed to alcoholic hepatitis from a relapse of alcohol use. However this case illustrates the importance of fully analyzing unexpected findings. The atypical lymphocytes seen on the peripheral smear and in the ascitic fluid cell count differential were not attributed to a reactive process. Rather, they led to the transjugular liver biopsy which is essential in making the diagnosis, and underscores the role of and importance of liver biopsy when the etiology of liver failure is unknown.
In conclusion, a hematologic malignancy infiltrating the liver, although rare, is a contraindication to liver transplantation. It is mandatory to exclude such processes in the correct clinical context. In our case, liver biopsy allowed prompt diagnosis and recognition of NK-like T-cell leukemia/lymphoma as the cause of acute liver failure.
S- Editor Wang J L- Editor Wang XL E- Editor Liu Y
| 1. | Polson J, Lee WM. AASLD position paper: the management of acute liver failure. Hepatology. 2005;41:1179-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 644] [Cited by in RCA: 641] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 2. | Murray KF, Carithers RL Jr. AASLD practice guidelines: Evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 516] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 3. | Lee WM. Acute liver failure. N Engl J Med. 1993;329:1862-1872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 497] [Cited by in RCA: 441] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 4. | Myszor MF, Record CO. Primary and secondary malignant disease of the liver and fulminant hepatic failure. J Clin Gastroenterol. 1990;12:441-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Rowbotham D, Wendon J, Williams R. Acute liver failure secondary to hepatic infiltration: a single centre experience of 18 cases. Gut. 1998;42:576-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 150] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Kojima H, Shimizu S, Yoshida C, Katsura Y, Suzukawa K, Mukai HY, Hasgawa Y, Imagawa S, Mori N, Nagasawa T. Rapidly progressive Lennert's lymphoma terminating in fulminant hepatic failure. Leuk Lymphoma. 2003;44:1409-1412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Santos ES, Raez LE, Salvatierra J, Morgensztern D, Shanmugan N, Neff GW. Primary hepatic non-Hodgkin's lymphomas: case report and review of the literature. Am J Gastroenterol. 2003;98:2789-2793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Lettieri CJ, Berg BW. Clinical features of non-Hodgkins lymphoma presenting with acute liver failure: a report of five cases and review of published experience. Am J Gastroenterol. 2003;98:1641-1646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Morali GA, Rozenmann E, Ashkenazi J, Munter G, Braverman DZ. Acute liver failure as the sole manifestation of relapsing non-Hodgkin's lymphoma. Eur J Gastroenterol Hepatol. 2001;13:1241-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Thompson DR, Faust TW, Stone MJ, Polter DE. Hepatic failure as the presenting manifestation of malignant lymphoma. Clin Lymphoma. 2001;2:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Yeshurun M, Isnard F, Garderet L, Rambeloarisoa J, Prevot S, Carbonell N, Najman A. Acute liver failure as initial manifestation of low-grade non-Hodgkin's lymphoma transformation into large-cell lymphoma. Leuk Lymphoma. 2001;42:555-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Anderson SH, Richardson P, Wendon J, Pagliuca A, Portmann B. Acute liver failure as the initial manifestation of acute leukaemia. Liver. 2001;21:287-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Stewart KS, Gordon MC. Non-Hodgkin lymphoma in pregnancy presenting as acute liver failure. Obstet Gynecol. 1999;94:847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Yoshikawa M, Yamane Y, Yoneda S, Iwasawa S, Nishimura K, Kawamoto H, Nakano H, Fukui H, Nakamine H. Acute hepatic failure due to hepatosplenic B-cell non-Hodgkin's lymphoma in a patient infected with hepatitis C virus. J Gastroenterol. 1998;33:880-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Suzuki N, Tsuji H, Nakamura S, Asabe H, Sueishi K, Fujishima M. An autopsy case of Ki-1 lymphoma associated with hepatic failure. Am J Gastroenterol. 1998;93:115-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Souto P, Romãozinho JM, Figueiredo P, Ferreira M, Sousa I, Camacho E, Donato A, Freitas D. Severe acute liver failure as the initial manifestation of haematological malignancy. Eur J Gastroenterol Hepatol. 1997;9:1113-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Shehab TM, Kaminski MS, Lok AS. Acute liver failure due to hepatic involvement by hematologic malignancy. Dig Dis Sci. 1997;42:1400-1405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Woolf GM, Petrovic LM, Rojter SE, Villamil FG, Makowka L, Podesta LG, Sher LS, Memsic L, Vierling JM. Acute liver failure due to lymphoma. A diagnostic concern when considering liver transplantation. Dig Dis Sci. 1994;39:1351-1358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Zafrani ES, Gaulard P. Primary lymphoma of the liver. Liver. 1993;13:57-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Saló J, Nomdedeu B, Bruguera M, Ordi J, Ginès P, Castells A, Vilella A, Rodés J. Acute liver failure due to non-Hodgkin's lymphoma. Am J Gastroenterol. 1993;88:774-776. [PubMed] |
| 21. | Sathiapalan RK, Hainau B, Al-Mane K, Belgaumi AF. Favorable response to treatment of a child with T-cell-rich large B-cell lymphoma presenting with liver failure. J Pediatr Hematol Oncol. 2003;25:809-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Ortega López Juan J, López Espinosa J, Roqueta Mas J, Sabado Alvarez C, Ruiz Marcellan C, Iglesias Berengué J. [Acute liver failure due to T cell lymphoma without hepatic infiltration]. An Pediatr (Barc). 2003;58:59-62. [PubMed] |
| 23. | Petersen-Benz C, Hoffmann N, Beckurts T, Goeser T, Steffen HM, Dries V. Fulminant liver failure induced by hepatosplenic alphabeta T-cell lymphoma. Z Gastroenterol. 2003;41:1083-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Domingo-Domènech J, Fernández J, López-Guillermo A, Miquel R. [Fulminant hepatic failure as form of presentation of a peripheral T cell lymphoma]. Med Clin (Barc). 2002;119:715-716. [PubMed] |
| 25. | Blakolmer K, Gaulard P, Mannhalter C, Swerdlow S, Fassati LR, Rossi G, Maggi U, Conte D, Demetris AJ. Unusual peripheral T cell lymphoma presenting as acute liver failure and reappearing in the liver allograft. Transplantation. 2000;70:1802-1805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Schwartz RA, Rezuke WN, Cartun RW, Hasson J. Case report: an autopsy study of a rare T-cell lymphoma clinically misdiagnosed as fulminant hepatic disease. Conn Med. 1998;62:643-647. [PubMed] |
| 27. | Hino T, Sata M, Arima N, Nouno R, Kumashiro R, Koga Y, Uchimura Y, Yoshitake M, Sakisaka S, Kojiro M. A case of malignant lymphoma with hemophagocytic syndrome presenting as hepatic failure. Kurume Med J. 1997;44:53-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Greer JP, Cousar JB, Miller RF, Vogler LB, Goodin JC, Graber SE, Collins RD. T4+ (helper phenotype) chronic lymphocytic leukemia: case report with liver failure and literature review. Med Pediatr Oncol. 1988;16:356-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Zafrani ES, Leclercq B, Vernant JP, Pinaudeau Y, Chomette G, Dhumeaux D. Massive blastic infiltration of the liver: a cause of fulminant hepatic failure. Hepatology. 1983;3:428-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 55] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Rose MG, Berliner N. T-cell large granular lymphocyte leukemia and related disorders. Oncologist. 2004;9:247-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 108] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 31. | Greer JP, Kinney MC, Loughran TP Jr. T cell and NK cell lymphoproliferative disorders. Hematology Am Soc Hematol Educ Program. 2001;259-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 82] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Oshimi K. Leukemia and lymphoma of natural killer lineage cells. Int J Hematol. 2003;78:18-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 111] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 33. | Siu LL, Chan JK, Kwong YL. Natural killer cell malignancies: clinicopathologic and molecular features. Histol Histopathol. 2002;17:539-554. [PubMed] |
| 34. | Porcu P, Baiocchi RA, Magro C. Recent developments in the biology and therapy of T-cell and natural killer-cell lymphomas. Curr Opin Oncol. 2003;15:353-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Sun T, Brody J, Susin M, Marino J, Teichberg S, Koduru P, Hall WW, Urmacher C, Hajdu SI. Aggressive natural killer cell lymphoma/leukemia. A recently recognized clinicopathologic entity. Am J Surg Pathol. 1993;17:1289-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Cheung MM, Chan JK, Wong KF. Natural killer cell neoplasms: a distinctive group of highly aggressive lymphomas/leukemias. Semin Hematol. 2003;40:221-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 83] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 37. | Yachie A, Kanegane H, Kasahara Y. Epstein-Barr virus-associated T-/natural killer cell lymphoproliferative diseases. Semin Hematol. 2003;40:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Chan JK, Sin VC, Wong KF, Ng CS, Tsang WY, Chan CH, Cheung MM, Lau WH. Nonnasal lymphoma expressing the natural killer cell marker CD56: a clinicopathologic study of 49 cases of an uncommon aggressive neoplasm. Blood. 1997;89:4501-4513. [PubMed] |
| 39. | Ohnuma K, Toyoda Y, Nishihira H, Iguchi A, Honda K, Nagao T, Kigasawa H, Tanaka Y, Kikuta H. Aggressive natural killer (NK) cell lymphoma: report of a pediatric case and review of the literature. Leuk Lymphoma. 1997;25:387-392. [PubMed] |
| 40. | Imamura N, Kusunoki Y, Kawa-Ha K, Yumura K, Hara J, Oda K, Abe K, Dohy H, Inada T, Kajihara H. Aggressive natural killer cell leukaemia/lymphoma: report of four cases and review of the literature. Possible existence of a new clinical entity originating from the third lineage of lymphoid cells. Br J Haematol. 1990;75:49-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 167] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 41. | Murdock J, Jaffe ES, Wilson WH, McManus DT, Alexander HD, Morris TC. Aggressive natural killer cell leukemia/lymphoma: case report, use of telesynergy and review of the literature. Leuk Lymphoma. 2004;45:1269-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Gentile TC, Uner AH, Hutchison RE, Wright J, Ben-Ezra J, Russell EC, Loughran TP Jr. CD3+, CD56+ aggressive variant of large granular lymphocyte leukemia. Blood. 1994;84:2315-2321. [PubMed] |
| 43. | Macon WR, Williams ME, Greer JP, Hammer RD, Glick AD, Collins RD, Cousar JB. Natural killer-like T-cell lymphomas: aggressive lymphomas of T-large granular lymphocytes. Blood. 1996;87:1474-1483. [PubMed] |
| 44. | Ichimura K, Kagami Y, Suzuki R, Kojima M, Yoshino T, Ohshima K, Koike K, Kondo E, Taji H, Ogura M. Phenotypic analysis of peripheral T/NK cell lymphoma: study of 408 Japanese cases with special reference to their anatomical sites. Pathol Int. 2003;53:333-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |