Published online Jun 21, 2006. doi: 10.3748/wjg.v12.i23.3779
Revised: September 28, 2005
Accepted: October 26, 2005
Published online: June 21, 2006
Hepatobiliary cystadenomas are rare tumors that are difficult to diagnose preoperatively. They can reach large sizes that make them real intraoperative “surprises”. A 63-year-old woman, presented with a symptomatic huge abdominal cystic mass, underwent complete resection of the mass with safety margins. Histopathological report revealed mucinous hepatic cystadenoma with “ovarian-like” stroma and areas of sclerohyalinization. The differential diagnosis of the large cystic tumors which occupy the right hemiabdomen must include the biliary cystadenoma; the complete resection of the tumor with safety margins avoids local recurrence, and therefore represents the optimal therapy because of the malignant potential of the disease. The postoperative follow-up includes abdominal ultrasound or CT scan and CA 19-9 measurement.
- Citation: Beuran M, Venter MD, Dumitru L. Large mucinous biliary cystadenoma with “ovarian-like” stroma: A case report. World J Gastroenterol 2006; 12(23): 3779-3781
- URL: https://www.wjgnet.com/1007-9327/full/v12/i23/3779.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i23.3779
Biliary cystadenomas are rare epithelial tumors with obvious malignant potential (20% of cases), and are frequently multilocular, predominantly located in the right hepatic lobe. They grow slowly and frequently are discovered accidentally during the medical investigations/surgical interventions performed for other conditions. They are more frequently encountered in women (95%)[1]; the maximum incidence is over the age of 40[2].
Cystadenomas represent less than 5% of the hepatic cystic tumors of biliary origin[3-4], their prevalence being 20 times lower than that of the simple hepatic cyst[3]. Based principally on ultrasound and CT, it has been reported that the prevalence of the biliary cystadenomas is much lower, probably 1000 times lower than that of the simple hepatic cyst[2]. In the speciality literature, there have been reported under 100 cases of biliary cystadenomas[5]. We report herein a case of large hepatic mucinous cystadenoma with mesenchymal stroma and a review of this condition based on the study of the speciality literature.
A 63-year-old woman was urgently admitted to the Surgical Clinic with intense abdominal pain located predominantly in the right upper quadrant, which started 5 d before, and was associated with nausea and pressure sensation. Physical examination revealed enlarged abdomen with tenderness in the right hemiabdomen, and a smooth-surfaced large mass (30 cm × 30 cm), without lumbar contact, difficult to mobilize and dull to percussion; as well as an irreducible, painless umbilical hernia with dimensions 4 cm × 4 cm.
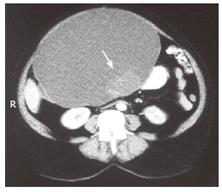
Abdominal ultrasound showed a cystic mass with dimensions 24 cm × 18 cm × 24 cm, thin walls, multiple echoes inside and multiple septations posteriorly which delineated other small cysts with dimensions of maximum 5 cm; but homogeneous structure of the liver. Laboratory findings were within normal ranges. Contrast-enhanced abdominal CT scan showed a large abdominopelvic cystic mass that compressed the left hepatic lobe in its superior region, extending caudally to the uterine body and anteriorly to the peritoneal layer (Figure 1); and a septum and a dense mass (5 cm × 3 cm) could be distinguished in the posterior region of the described mass (Figure 2).
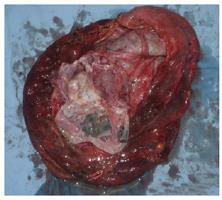
Surgery was performed through a supra- and subumbilical incision, which discovered a large cystic mass (25 cm × 25 cm) belonged to the hepatic segments III-IV-V, with the gallbladder lying over the mass (Figures 3 and 4). A total of 2500 mL of brown, mucinous fluid was evacuated by puncturing the cystic mass; and a mass with increased consistency and irregular surface was palpated in the posterior region of the tumor (Figure 5). Retrograde cholecystectomy, complete resection of the tumor and umbilical hernia repair were performed.
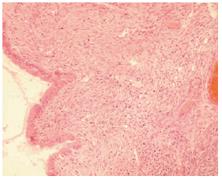
Cross-section of the specimen showed multiple septations in the inner surface and many locules with dimensions between 2-5 cm with mucinous content in the posterior region (Figure 6). Histopathological report revealed mucinous hepatic cystadenoma with “ovarian-like” stroma and areas of sclerohyalinization (Figure 7).
The postoperative course was uneventful ant the patient was discharge at the 10th postoperative day. A clinical check-up was carried out after a month, confirming the favorable evolution.
The problems that occur during the diagnosis of the large hepatic cystic tumors include the determination of the involved organs and differential diagnosis, especially with hepatic malignancies. Pathologically, two types of biliary cystadenomas are described: mucinous and serous[1]. Mucinous cystadenomas appear especially in women (95% of cases, possibly due to hormonal influence) and are located in intrahepatic region (84%), common bile duct (6%), hepatic ducts (4%), cystic duct (4%) and gallbladder 2%[1]. The pathogenesis of the tumor is unknown. It is considered that it has congenital origin from an aberrant intrahepatic biliary duct or from misplaced germ cells[2].
Biliary cystadenoma with mesenchymal stroma represents a tumoral histological variant that only affects women and has a columnar or cuboidal epithelium, an intermediary subepithelial layer of mesenchymal or fusiform cells, resembling ovarian stroma (“ovarian-like” stroma) and an external layer formed by a fibroconjunctive sheath that separates it from adjacent hepatic parenchyma, making a pseudocapsule. Biliary cystadenomas are usually multilocular .
Ultrasonography is the first paraclinical exploration used and shows an anechoic mass with hyperechoic internal septations and possibly mural papillary growths[4]. Abdominal CT demonstrates a single area with thin walls and internal septations; intravenous injection of contrast medium enhances the density of the cystic wall and may visualize the intracystic septations and the mural nodules[2,4]. MRI demonstrates the relationships of the tumor with local vascular structures and may bring informations about the nature of the intracystic fluid[6].Hepatic angiography shows an avascular lesion and possibly displacement of the intrahepatic vascular structures, but scintigraphy has a limited interest[2,4].Intra-operative ultrasound allows an exact identification of the site of the cystic mass and its relations with the adjacent biliovascular structures[7].
The serum CA 19-9 level may be elevated in biliary cystadenoma with mesenchymal stroma. It has been reported normalization of CA 19-9 level after the resection of the tumor, suggesting the possibility of using this investigation during the long-term post-operative follow-up of the patients[2]. The measurement of the CA 19-9 (marked increase but variable) and CEA (moderate increase) levels, originating from the intracystic fluid, differentiate these tumors from the simple and hydatid cysts of the liver, but cannot differentiate the biliary cystadenoma from cystadenocarcinoma[2]. Because of these causes, the differential diagnosis is difficult, especially with simple hepatic cyst, hepatic hydatid cyst and cystadenocarcinoma.
The evolution of biliary cystadenoma is slow with the possibility to occur various complications, out of which malignant transformation is of distinct importance. A study has demonstrated that 1/3 of hepatic cystadenocarcinomas arise from preexisting benign biliary cystadenomas[4].
The treatment of biliary cystadenoma is exclusively surgical. Complete resection of the tumor with intact hepatic resection margin is recommended, sometimes even hemihepatectomy[3]. This therapeutic approach is motivated by the malignant potential of the lesion and by the difficulty of the preoperative differential diagnosis with biliary cystadenocarcinoma. A study emphasizes that biliary cystadenoma with mesenchymal stroma may be enucleated because of the presence of a pseudocapsule which forms a dissection plane[4]. The indication for tumor enucleation is represented by small lesions, with central location, close to the hepatic hilum. Other performed operations, such as drainage through a Roux-en-Y loop, marsupialisation, percutaneous drainage followed by alcoholisation, partial cystectomy, and aspiration followed by partial excision, are associated with certain recurrence[2,5].
Postoperative follow-up is necessary; within the first year of operation, an ultrasound or CT scan of the liver should be performed after 6 mo, and then yearly. It is also useful to measure serum CA 19-9 level after the same time period.
S- Editor Wang J L- Editor Kumar M E- Editor Liu WF
| 1. | Scott SH. Masses of the Liver. Diagnostic Surgical Pathology. Philadelphia: Lippincott Williams & Wilkins 1999; 1561-1562. |
| 2. | Farges O, Menu Y, Benhamou JP. Non-parasitic cystic disease of the liver and intrahepatic biliary tree. Surgery of the Liver and Biliary Tract. 3rd ed. London: W.B. Saunders Company Ltd 2000; 1249-1250. |
| 3. | Sutton CD, White SA, Berry DP, Dennison AR. Intrahepatic biliary cystadenoma causing luminal common bile duct obstruction. Dig Surg. 2000;17:297-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Dixon E, Sutherland FR, Mitchell P, McKinnon G, Nayak V. Cystadenomas of the liver: a spectrum of disease. Can J Surg. 2001;44:371-376. [PubMed] |
| 5. | Quinlan MR. Tumors of the liver in Zuidema DG ed. Shackelford's Surgery of the Alimentary Tract. 4th ed. Philadelphia: W B. Saunders Company 1996; 512-525. |
| 6. | Hagiwara A, Inoue Y, Shutoh T, Kinoshita H, Wakasa K. Haemorrhagic hepatic cyst: a differential diagnosis of cystic tumour. Br J Radiol. 2001;74:270-272. [PubMed] |
| 7. | Kruskal JB, Kane RA. Intraoperative sonography of the biliary system. AJR Am J Roentgenol. 2001;177:395-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |