Published online May 7, 2006. doi: 10.3748/wjg.v12.i17.2762
Revised: August 12, 2005
Accepted: September 8, 2005
Published online: May 7, 2006
AIM: To explore the influence of angiostatin up-regulation on the biologic behavior of gallbladder carcinoma cells in vitro and in vitro, and the potential value of angiostatin gene therapy for gallbladder carcinoma.
METHODS: A eukaryotic expression vector of pcDNA3.1(+) containing murine angiostatin was constructed and identified by restriction endonuclease digestion and sequencing. The recombinant vector pcDNA3.1-angiostatin was transfected into human gallbladder carcinoma cell line GBC-SD with Lipofectamine 2000, and paralleled with the vector and mock control. The resistant clone was screened by G418 filtration. Angiostatin transcription and protein expression were examined by RT-PCR, immunofluorescence and Western-blot. The supernatant was collected to treat endothelial cells. Cell proliferation and growth in vitro were observed under microscope.
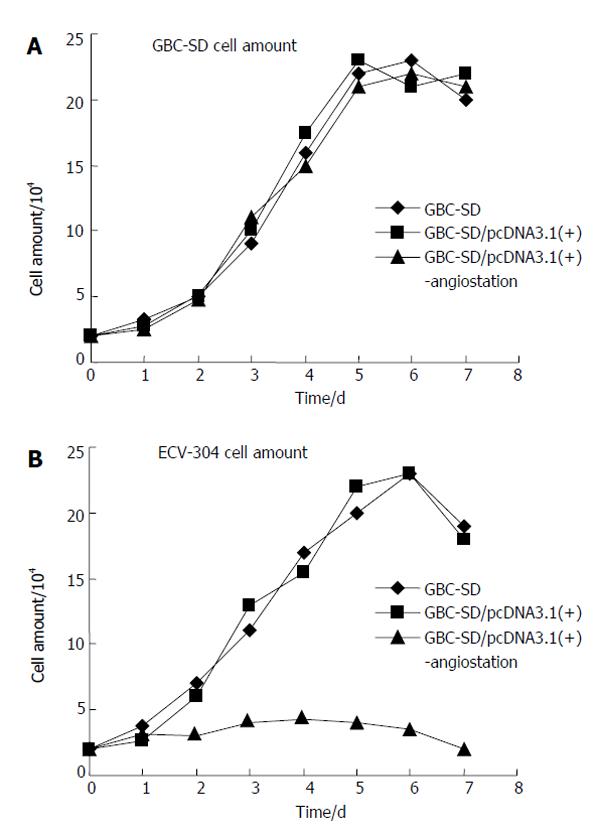
RESULTS: Murine angiostatin cDNA was successfully cloned into the eukaryotic expression vector pcDNA3.1 (+). After 14 d of transfection and selection with G418, macroscopic resistant cell cloning was formed in the experimental group transfected with pcDNA 3.1(+)-angiostatin and vector control. But untreated cells died in the mock control. Angiostatin was detected by RT-PCR and protein expression was detected in the experimental group by immunofluorescence and Western-blot. Cell proliferation and growth in vitro in the three groups were observed respectively under microscope. No significant difference was observed in the growth speed of GBC-SD cells between groups that were transfected with and without angiostatin. After treatment with supernatant, significant differences were observed in endothelial cell (ECV-304) growth in vitro. The cell proliferation and growth were inhibited.
CONCLUSION: Angiostatin does not directly inhibit human gallbladder carcinoma cell proliferation and growth in vitro, but the secretion of angiostatin inhabits endothelial cell proliferation and growth.
- Citation: Yang DZ, He J, Zhang JC, Wang ZR. Expression of angiostatin cDNA in human gallbladder carcinoma cell line GBC-SD and its effect on endothelial proliferation and growth. World J Gastroenterol 2006; 12(17): 2762-2766
- URL: https://www.wjgnet.com/1007-9327/full/v12/i17/2762.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i17.2762
Gallbladder carcinoma is the most common malignant tumor of the biliary tract and a particularly high incidence is observed in Chile, Japan, and northern India. After common treatment, the prognosis of gallbladder carcinoma patients is poor[1].
A large body of work by a number of laboratories in the past 3 decades has provided both direct and indirect evidence that tumor growth and metastasis are accompanied with the growth of new blood vessels[2].
As previously reported, angiostatin is a potent antiangiogenic endogenous protein[3]. In the present study, we constructed a mammalian expression vector that was cloned as an angiostatin gene. Following stable transfection of this vector into human gallbladder carcinoma cell line GBC-SD, we observed the expression of angiostatin and its antiangiogenic effect by evaluating the influence of cultured human umbilical vein endothelial cells (ECV-304).
The human gallbladder carcinoma cell line GBC-SD and the endothelial cell line ECV-304 were purchased from China Center for Type Culture Collection. EcoRI, XbaI, PmeI, HindIII, XbaI and PvuIwere purchased from Bioson Corporation. Lipofectamine™ 2000 and G418 were purchased from Gibco Company. Recombinant eukaryotic expression vector pcDNA3.1(+)-angiostatin and rabbit anti-HAtag multiclonl antibody were presented by Dr. Jicheng Zhang. Trizol reagent, reverse transcriptase, and Taq DNA polymerase were purchased from Life Technologies, Inc. FITC was purchased from Boster Biological Technology Co.
Gallbladder carcinoma cells and endothelial cells were cultured in RPMI1640 (Gibco) supplemented with 10% fetal bovine serum (FBS) (Sijiqing, Hangzhou, China), penicillin (100 units/mL) and streptomycin (100 mg/mL) in a humidified atmosphere containing 5% CO2 at 37 °C.
Mouse angiostatin cDNA fragment encoding for the NH2-terminal secretory signal sequence(SS) and kringle1-4(K1-4) regions of mouse plasminogen, fused with an antigenic epitope tag HA(HA tag) to the COOH terminus of kringle 4, was inserted into enkaryotic expression vector pcDNA3.1(+). The structure of the recombinant vector pcDNA3.1(+)-angiostatin was confirmed by restriction endonuclease digestion and sequencing. Recombinant clones were identified by HindIII, XbaI and PmeI digestion. Positive clones were further confirmed by sequencing.
Gallbladder carcinoma cells (GBC-SD) in logarithmic growth phase were plated on 24-well plates at 2×105 cells/well, and approximately 80% confluence was obtained after overnight incubation. Cultured GBC-SD cells were divided into three groups: transfected with recombinant pcDNA3.1-angiostatin (group A), pcDNA3.1 (+) vector (group B) and without pcDNA3.1 (+) vector(group C). Transfection was performed according to the instructions of Lipofectamine TM2000 reagent kit (Gibco). The cells were then cultured in complete medium containing G418 (50 mg/L) for 14 d. G418-resistant pooled cells were subjected to further studies. Then the isolated resistant cell clones were selected and amplified. Cell growth curve was also plotted.
Total RNA was isolated from GBC-SD cells using Trizol reagent. Reverse transcription was performed with 1 ug of total RNA in a total volume of 20 μL containing reverse transcriptase. The PCR reagents, including 0.5 units of Taq DNA polymerase, were added to a final volume of 25 μL. A 35-cycle amplification profile consisted of denaturation at 94 °C for 1 min, annealing at 56 °C for 1 min, and extension at 72 °C for 1 min. Primers used in PCR were designed according to the reported angiostatin cDNA sequence. The primer sequences were as follows: 5’end: 5’-CCCAACATGGACCATAAGGAAGT-3’ and 3’end: 5’-TGTGGGCAATTCCACAACACTC-3’. Human-actin primers were used as positive controls. Negative controls without RNA and reverse transcriptase were also assessed. The PCR products were identified by 1% agarose gel electrophoresis.
GBC-SD cells with pcDNA3.1(+)angiostatin in logarithmic growth phase were implanted into 6-well plates. After 24 h, the glass flake was taken out and imunofluorescence cytochemistry was carried out. For immunofluorescence, cells on glass flake were fixed for 15min in 3.7% formaldehyde in PBS containing 1mM EGTA at room temperature. After fixation, the cells were made permeable by incubating with 0.2% Triton X-100 in PBS for 15 min, and then washed with PBS. After being blocked with PBS including 1% BSA, antibodies were applied and incubated for 1h at 37 °C. The cells were then stained with secondary antibodies. After being washed with PBS, the expression was detected under fluorescent microscope.
The cells in the three groups were cultured in conditioned media for 5 d. Cell supernatant was mixed with lysine-sepharose and incubated at 4 °C overnight. The resin was washed with Tris-HCl (pH8.0) and protein was eluted. Protein concentration was determined by bicinchoninic acid assay (BCA) with bovine serum albumin as standard. Equal aliquots (40 μg) of protein from cell supernatants were subjected to electrophoresis on 10% sodium dodecyl sulfate (SDS)-polyacrylamide gel. Proteins were transferred onto PVDF membranes (mMillipore) using the transfer buffer for 2 h. The membranes were then blocked for 1.5 h using 5% nonfat dried milk in phosphate-buffered saline containing 0.1% Tween 20 (PBS-T), washed with PBS-T, and incubated at 4 °C overnight in the presence of anti-rabbit HA-tagged antibody.The membranes were washed with PBS-T and incubated with secondary peroxidase-conjugated anti-rabbit immunoglobulin G for 1 h. Following washing with PBS-T, immunoreactive bands were visualized by the enhanced chemiluminescence system (Amersham Life Science).
In logarithmic growth phase of the three groups of gallbladder carcinoma cells (GBC-SD), the supernatant was collected. Endothelial cells (ECV-304) were plated onto 24-well plates at 1×104 cells/well and ECV-304 cells were treated with supernatant separately for 7 d (supernatant/ medium=1/9). Viable cells were counted under microscope everyday and growth curves were plotted.
Data were analyzed by statistical software of SPSS 10.0. Differences between groups were examined by Student’s t test. P < 0.01 was considered statistically significant.
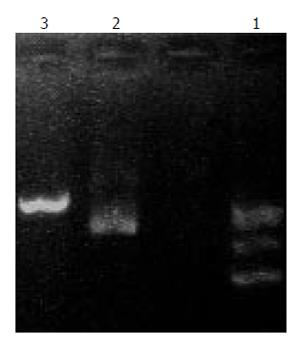
The recombinant plasmid was released by restrictive digestion with HindIII, XbaI and PmeI. As shown in electrophoresis, the linear recombinant plasmid was about 7.0kb, being a fragment of 1.4kb, suggesting that angiostatin fragment was inserted into the pcDNA3.1 (+) vector, named recombinant plasmid pcDNA3.1- angio (Figure1). The sequence obtained was the same as the reported sequence of angiostatin cDNA, indicating that the murine gene was successfully cloned into the eukaryotic expression vector pcDNA3.1 (+).The recombinant plasmid was linearized by pvu I(Figure 2).
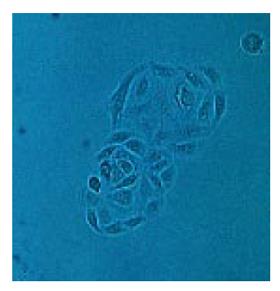
Gallbladder carcinoma cells (GBC-SD) transfected with the corresponding vectors were selected by G418 for 14 d. The transfected pcDNA3.1-angiostatin and vector control groups formed macroscopic cell clones (Figure 3), but the mock group of cells was completely dead after 8 d of selection.
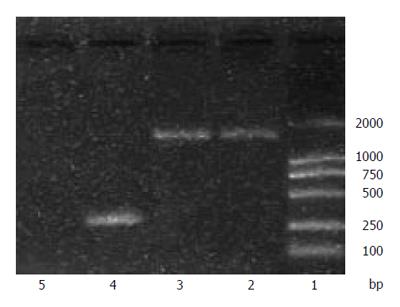
GBC-SD cells transfected with pcDNA3.1- angiostatin were prepared. Total RNA was extracted and used as the template. A band was detected at 1.4 kb with PCR using angiostatin primers, indicating the presence of angiostatin cDNA in the GBC-SD cancer cells (Figure 4).
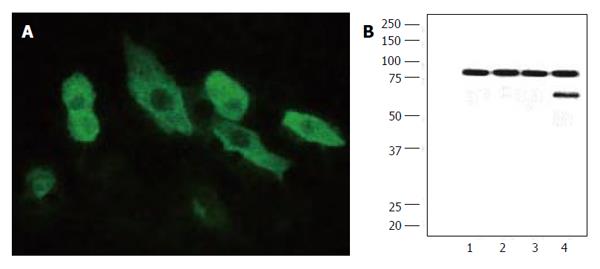
Immunofluorescence showed signals of angiostatin in the experimental group of cell clones genetically engineered but not in the controls (Figure 5A). Supernatants of cultured cells in three groups were collected and analyzed by Western blotting. A band in a molecular mass of 58 000 kb was detected with rabbit anti-HA-tagged antibody from the cells transfected with pcDNA3.1-angiostatin, but no band was detected in mock control group or vector control group (Figure 5B).
To detect the biological activity of encoded angiostatin in vitro, tumor cells transfected with or without the corresponding vectors were cultured for 7 d to plot cell growth curve (Figure 6A). Under microscope, no obvious difference was observed in the cell morphology of the three groups of cells. Cell growth curves indicated no change in cell growth speed and doubling time in the three groups. These results indicate that up-regulated angiostatin expression could neither directly inhibit cell growth and proliferation nor affect cell cycle in vitro. But the biological activity of cells treated with supernatant of GBC-SD/pcDNA3.1(+)-angiostatin and cell growth were obviously inhabited. The cell growth curve of the vector and mock control groups was similar (Figure 6B). These results indicate that angiostatin expression could directly inhibit endothelial cell growth and proliferation in vitro.
Angiogenesis refers to the formation of new blood vessels. Since Dr. Folkman[15] raised the hypothesis of tumor angiogenic dependence, experimental evidence has validated that tumor growth companies new blood vessel growth. At the prevascular stage, tumor is unable to grow to a size beyond 2-3 mm3 and remains in its dormant state. However, once the angiogenic phenotype of tumor is switched on, tumor growth rate changes from linear to exponential[4-6]. Infiltration of new blood vessels in tumors not only supplies nutrients and oxygen for tumor cells, but also removes the waste products produced by tumor cells. In addition, endothelial cells can communicate directly with tumor cells by producing tumor growth promoting factors.
Angiogenesis begins when a fibrin clot forms on the adventitial surface of an existing blood vessel[7], which is followed by sprouting of new capillaries. The initial phase begins with increased vascular permeability and local degradation of the vessel wall. Endothelial cells enter the tumor stroma and proliferate. At this time, the cells may be most vulnerable to agents that interfere with their proliferation, since they lack protection from other cell types[8]. The next step in vessel formation is recruitment of pericytes, followed by smooth muscle cells.
It appears that a switch to the angiogenic phenotype requires a local change in the balance between angiogenic factors and inhibitors[9]. Among the angiogenic factors, fibroblast growth factor (FGF)[10] and vascular endothelial growth factor (VEGF)/vascular permeability factor (VPF)[11] are most commonly expressed in tumors. Others are inhibitors such as angiostatin[12], thrombospondin-1[13], 16-kd prolactin fragment[14], interferon-α and β[15], and endostatin[16]. Because cancer cannot grow or spread without the formation of new blood vessels[17], scientists are trying to find ways to stop angiogenesis.
Tumor angiogenesis is often the consequence of an angiogenic imbalance in which pro-angiogenic factors predominate over anti-angiogenic factors[5]. Furthermore, angiogenesis is essential for growth and metastasis of most solid cancers[18]. Gallbladder carcinoma is not a grossly vascular tumor, but is related to angiogenesis[19]. Antiangiogenic treatment may be necessary and potential for gallbladder carcinoma.
Angiostatin is an internal fragment of plasminogen and may contain either the first three (K1-3) or four (K1-4) kringle domains[20]. A similar activity has been reported for kringle 5 (K-5) of plasminogen[21]. Three receptors of angiostatin on endothelial cells have been reported to date. Adenosine triphosphate (ATP) synthase is one of the receptors. The presence of this typically mitochondrial enzyme on the endothelial cell surface is somewhat surprising[22]. Two other potential target receptors of angiostatin are angiomotin[23] and integrin alpha(v)beta(3)[24]. These receptors on the surface of endothelial cells may be located at sites so proximal to one another that angiostatin may be able to interact with more than one simultaneously[25]. Alternatively, multiple targets could be implicated in binding to different kringles of angiostatin as a function of receptor and peptide presentation[26].
Although angiostatin is a potent inhibitor of angiogenesis and tumor growth[27], the need for high doses, repeated injections and long-term administration of this protein have made it less attractive for clinical trials[28]. In order to develop alternative strategies for therapy, we have investigated the possibility of angiostatin gene therapy. When mouse angiostatin cDNA was transfected into human gallbladder carcinoma cell line GBC-SD and endothelial cell line (ECV-304), angiostatin cDNA was present in cancer cells, and a secreted form of angiostatin was established by immunofluorescence and Western-blot. Although angiostatin had no direct effect on gallbladder carcinoma cell growth in vitro, the supernatant of ECV-304 cells inhibited the growth of endothelial cells in vitro. Xu et al[29] engineered a recombinant adeno-associated virus (AAV) vector encoding mouse angiostatin and found that it suppresses metastatic liver cancer in mice. In our study, similar results were achieved using Lipofectamine 2 000 for transfection. These results support that angiostatin-gene therapy is a potential strategy in the treatment of gallbladder carcinoma.
In conclusion, angiostatin has no direct effect on gallbladder carcinoma cell growth in vitro, but inhibits the growth of ECV-304 cells in vitro.
S- Editor Guo SY L- Editor Wang XL E- Editor Bi L
| 1. | Misra S, Chaturvedi A, Misra NC, Sharma ID. Carcinoma of the gallbladder. Lancet Oncol. 2003;4:167-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 465] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 2. | Gasparini G, Longo R, Fanelli M, Teicher BA. Combination of antiangiogenic therapy with other anticancer therapies: results, challenges, and open questions. J Clin Oncol. 2005;23:1295-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 148] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 3. | Cao Y. Antiangiogenic cancer therapy. Semin Cancer Biol. 2004;14:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Ellis LM, Liu W, Ahmad SA, Fan F, Jung YD, Shaheen RM, Reinmuth N. Overview of angiogenesis: Biologic implications for antiangiogenic therapy. Semin Oncol. 2001;28:94-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Giuliani N, Colla S, Rizzoli V. Angiogenic switch in multiple myeloma. Hematology. 2004;9:377-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | van Hinsbergh VW, Collen A, Koolwijk P. Role of fibrin matrix in angiogenesis. Ann N Y Acad Sci. 2001;936:426-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 218] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 7. | Egginton S, Zhou AL, Brown MD, Hudlicka O. The role of pericytes in controlling angiogenesis in vivo. Adv Exp Med Biol. 2000;476:81-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Sun FY, Guo X. Molecular and cellular mechanisms of neuroprotection by vascular endothelial growth factor. J Neurosci Res. 2005;79:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Neri D, Bicknell R. Tumour vascular targeting. Nat Rev Cancer. 2005;5:436-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 481] [Cited by in RCA: 459] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 10. | Dalal S, Berry AM, Cullinane CJ, Mangham DC, Grimer R, Lewis IJ, Johnston C, Laurence V, Burchill SA. Vascular endothelial growth factor: a therapeutic target for tumors of the Ewing's sarcoma family. Clin Cancer Res. 2005;11:2364-2378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 90] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Mukhopadhyay D, Zeng H, Bhattacharya R. Complexity in the vascular permeability factor/vascular endothelial growth factor (VPF/VEGF)-receptors signaling. Mol Cell Biochem. 2004;264:51-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Narizhneva NV, Razorenova OV, Podrez EA, Chen J, Chandrasekharan UM, DiCorleto PE, Plow EF, Topol EJ, Byzova TV. Thrombospondin-1 up-regulates expression of cell adhesion molecules and promotes monocyte binding to endothelium. FASEB J. 2005;19:1158-1160. [PubMed] |
| 13. | Okamoto R, Ueno M, Yamada Y, Takahashi N, Sano H, Suda T, Takakura N. Hematopoietic cells regulate the angiogenic switch during tumorigenesis. Blood. 2005;105:2757-2763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Izawa JI, Sweeney P, Perrotte P, Kedar D, Dong Z, Slaton JW, Karashima T, Inoue K, Benedict WF, Dinney CP. Inhibition of tumorigenicity and metastasis of human bladder cancer growing in athymic mice by interferon-beta gene therapy results partially from various antiangiogenic effects including endothelial cell apoptosis. Clin Cancer Res. 2002;8:1258-1270. [PubMed] |
| 15. | Folkman J. Endogenous angiogenesis inhibitors. APMIS. 2004;112:496-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 225] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 16. | Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature. 2000;407:249-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6437] [Cited by in RCA: 6481] [Article Influence: 259.2] [Reference Citation Analysis (0)] |
| 17. | Castellino FJ, Ploplis VA. Structure and function of the plasminogen/plasmin system. Thromb Haemost. 2005;93:647-654. [PubMed] |
| 18. | Culy C. Bevacizumab: antiangiogenic cancer therapy. Drugs Today (Barc). 2005;41:23-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Geiger JH, Cnudde SE. What the structure of angiostatin may tell us about its mechanism of action. J Thromb Haemost. 2004;2:23-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | van Moorselaar RJ, Voest EE. Angiogenesis in prostate cancer: its role in disease progression and possible therapeutic approaches. Mol Cell Endocrinol. 2002;197:239-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 77] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Gonzalez-Gronow M, Kalfa T, Johnson CE, Gawdi G, Pizzo SV. The voltage-dependent anion channel is a receptor for plasminogen kringle 5 on human endothelial cells. J Biol Chem. 2003;278:27312-27318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Arakaki N, Nagao T, Niki R, Toyofuku A, Tanaka H, Kuramoto Y, Emoto Y, Shibata H, Magota K, Higuti T. Possible role of cell surface H+ -ATP synthase in the extracellular ATP synthesis and proliferation of human umbilical vein endothelial cells. Mol Cancer Res. 2003;1:931-939. [PubMed] |
| 23. | Troyanovsky B, Levchenko T, Mansson G, Matvijenko O, Holmgren L. Angiomotin: an angiostatin binding protein that regulates endothelial cell migration and tube formation. J Cell Biol. 2001;152:1247-1254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 284] [Cited by in RCA: 289] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 24. | Tarui T, Miles LA, Takada Y. Specific interaction of angiostatin with integrin alpha(v)beta(3) in endothelial cells. J Biol Chem. 2001;276:39562-39568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 145] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 25. | Mayhew TM, Charnock-Jones DS, Kaufmann P. Aspects of human fetoplacental vasculogenesis and angiogenesis. III. Changes in complicated pregnancies. Placenta. 2004;25:127-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 219] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 26. | Kim J, Hajjar KA. Annexin II: a plasminogen-plasminogen activator co-receptor. Front Biosci. 2002;7:d341-d348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 118] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 27. | Cao Y, Xue L. Angiostatin. Semin Thromb Hemost. 2004;30:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Cáceres W, González S. Angiogenesis and cancer: recent advances. P R Health Sci J. 2003;22:149-151. [PubMed] |
| 29. | Xu R, Sun X, Tse LY, Li H, Chan PC, Xu S, Xiao W, Kung HF, Krissansen GW, Fan ST. Long-term expression of angiostatin suppresses metastatic liver cancer in mice. Hepatology. 2003;37:1451-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |