Published online Apr 28, 2006. doi: 10.3748/wjg.v12.i16.2629
Revised: January 9, 2006
Accepted: January 14, 2006
Published online: April 28, 2006
Colonic varices are a very rare cause of lower gastrointestinal bleeding. Fewer than 100 cases of colonic varices, and 30 cases of idiopathic colonic varices (ICV) have been reported in the English literature. Among these 30 cases of ICV, 19 cases were diagnosed by angiography, and 7 operated cases were diagnosed later as ileocecal vein deficit, hemangioma, and idiopathic in 1, 1, 5 cases, respectively. We report the case of a 24-year-old man who suffered from multiple episodes of hematochezia of varying degree at the age of 11 years. He had severe anemia with hemoglobin of 21 g/L. On colonoscopy, tortuously dilated submucosal vein and friable ulceration covered with dark necrotic tissues especially at the rectosigmoid region were seen from the rectum up to the distal descending colon. It initially appeared to be carcinoma with varices. Mesenteric angiographic study suggested a colonic hemangioma. Low anterior resection was done due to medically intractable and recurrent hematochezia. Other bowel and mesenteric vascular structures appeared normal. Microscopic examination revealed normal colonic mucosa with dilated veins throughout the submucosa and serosa without representing new vessel growth. Taken all of these findings together, the patient was diagnosed as ICV. His postoperative course was uneventful.
- Citation: Han JH, Jeon WJ, Chae HB, Park SM, Youn SJ, Kim SH, Bae IH, Lee SJ. A case of idiopathic colonic varices: A rare cause of hematochezia misconceived as tumor. World J Gastroenterol 2006; 12(16): 2629-2632
- URL: https://www.wjgnet.com/1007-9327/full/v12/i16/2629.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i16.2629
Colonic varices, a very rare cause of lower gastrointestinal bleeding, are usually secondary to portal hypertension. It was reported that the incidence of colonic varices is 0.07% (2 of 2912 cases)[1]. One case had liver failure, and the other case had chronic pancreatitis. There are no autopsy data about idiopathic colonic varices. Fewer than 100 cases of colonic varices have been reported[1], and 23 reports containing 30 patients with idiopathic colonic varices (ICV) have been reported in the English literature[2-23]. Diagnosis of idiopathic colonic varices is most accurately achieved by mesenteric angiography[3-19]. But in some cases, operation could reveal secondary causes or changed pathologic diagnosis[18,19,24]. We report a patient whose diagnosis of idiopathic colonic varices was confirmed by the segmental colonic resection.
A 24-year-old man was admitted to hospital with exertional dyspnea and weakness. He had a 13-year history of multiple episodes of hematochezia of varying degree. At age 22, he visited our hospital due to dizziness. He denied alcohol consumption, or any family history of gastrointestinal bleeding. He had severe anemia with hemoglobin of 27 g/L. After 2-unit blood transfusion, he refused further investigations or management.
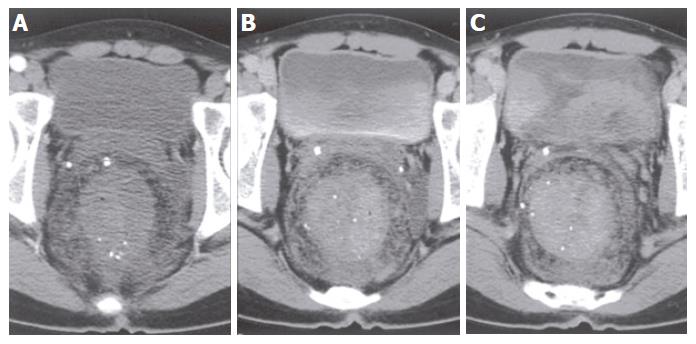
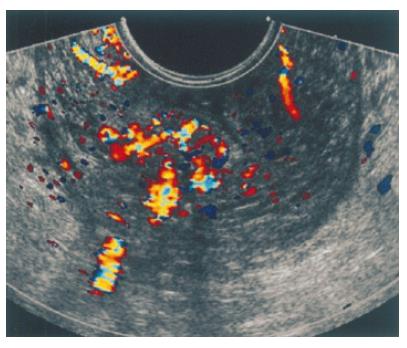
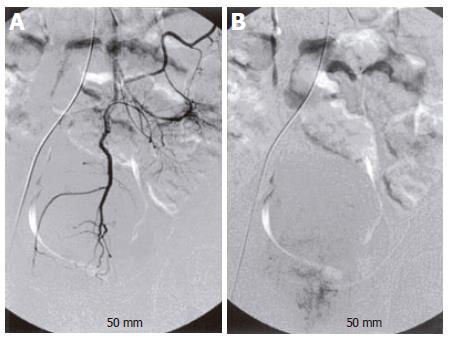
On admission, he was pale with mild tachycardia but had no abnormality on physical examination. Laboratory studies showed 4.93 ×109/WBC, 21 g/L hemoglobin, 0.09% hematocrit, 256 ×109/L platelets, and 22.2 μmol/L iron. Coagulation studies, liver function tests, and viral hepatitis serology were normal. Colonoscopy revealed considerable bluish and tortuously dilated submucosal veins which were seen from the rectum up to the distal descending colon, and friable ulceration covered with dark necrotic tissues especially at the rectosigmoid region (Figure 1). It seemed to be carcinoma with varices. Gastroduodenoscopic examination showed unremarkable finding, without evidence of varices or arteriovenous malformations. Abdominal ultrasonography also revealed no abnormal finding. An abdomen-pelvis triphasic computed tomography showed thickened bowel wall, intramural calcification and delayed enhancement from the rectum up to the descending colon (Figure 2). Transrectal Doppler sonography also demonstrated diffuse wall thickening with internal hypervascular structure (Figure 3). Selective angiography of the superior and inferior mesenteric artery showed delayed venous pooling in rectum but no other abnormal vascular structure (Figure 4). The angiographic diagnosis was a colonic hemangioma.
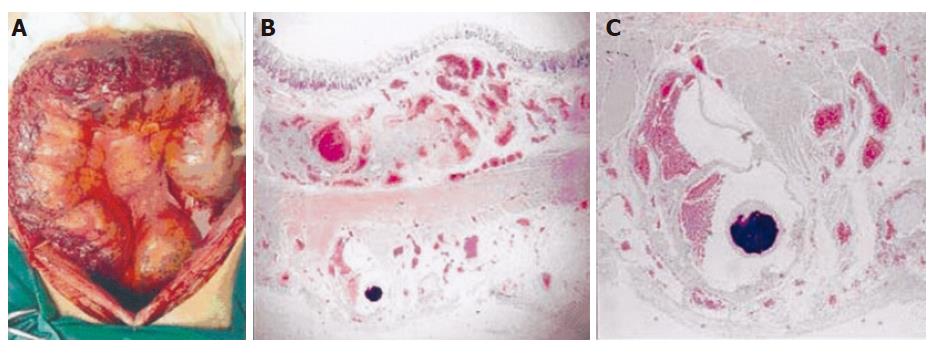
Low anterior resection was done due to medically intractable and recurrent hematochezia. During surgery, tortuously dilated subserosal and mesenteric vessels were seen at the rectum, sigmoid colon and distal descending colon (Figure 5A). Other bowel and mesenteric vascular structures appeared to be normal. Microscopic examination revealed normal colonic mucosa with dilated veins throughout the submucosa and serosa without new vessel formation (Figures 5B and 5C). In addition, thrombi were frequently observed in the endovascular lumen, and dystrophic calcification was also often found in the wall of vessels. He remained well showing no further signs of gastrointestinal hemorrhage at the time when he was reported in this paper.
Colonic varices are a very rare cause of lower gastrointestinal bleeding. Portal hypertension is the most common cause of colonic varices, which are usually located in the rectosigmoid region and the cecum[16]. Other less common causes of colonic varices are congestive heart failure, mesenteric vein thrombosis, pancreatitis with splenic vein thrombosis and adhesions, and mesenteric vein compression[1,2].
The varix is a descriptive term of enlarged and convoluted vein, artery or lymphatic vessel, which does not indicate the etiology of them. Establishing the diagnosis of ICV amid various factors remains difficult. It needs to exclude secondary causes by laboratory and imaging studies, such as liver function test, hepatitis serology, and liver sonography or computed tomography. Diagnosis of ICV usually requires angiography with visualization of the enlarged vessels showing prolonged observation of the venous phase but no portal/mesenteric vein obstruction[3,5]. Gross examination and biopsy under laparoscope or exploration can definitely confirm ICV.
We fully reviewed 30 cases reported as ICV. Hemangioma and vascular malformation are described as ICV in some of these reports[2,3,18,19]. But hemangioma has obviously different pathologic findings, and vascular malformation has plainable etiology. So, in our opinion, hemangioma and vascular malformation can be ruled out from ICV. According to these, 21 reports containing 25 patients remain to be idiopathic[4-17,20-23]. In more than half of the cases, the total colon is affected[6-9,14-16,20-22], and in segment-involved cases, the lesions are distributed equally between right and left colon. About 30% of these have familial tendency[8-11,14-16,20,21] and more than half of these manifest the onset of hematochezia before the third decade[9-13,15-17,22], suggesting that ICV may be congenital in origin. But the number of the cases is too small to conjecture the inheritance pattern of ICV. Angiography has been performed in only 19 cases[3-19]. Before angiography, two of these cases, suspected to be ICV, were diagnosed as congenital anomaly of the portocaval system[2] and hemangioma[3]. 7 cases which were surgically confirmed, were diagnosed as congenital failure of ileocecal vein[18], hemangioma[19], and ICV[15-17,19,20] in 1, 1, 5 cases, respectively.
ICV is usually accompanied with recurrent and massive rectal bleeding. It is presumed that bleeding from colonic varices is the result either of abrasion from hard stool in the distal colon, or of pressure ischemia and sloughing of the overlying mucosa in the cecum[16].
The barium contrast enema may be helpful, but is often misinterpreted as air bubble, fecal material, polyposis, carcinoma, or as normal[12]. Therefore, it is unreliable. Colonoscopy is more sensitive, but collapse of varices by excessive air inflation can make the physician to mistake ICV as normal condition. ICV can mimic polyp, cancer, and ulcerative colitis. Biopsy may induce massive hemorrhage[15].
Scintigraphic studies have not been found to be adequate in localizing the segment of colon associated with bleeding varices but can detect hemorrhage with greater sensitivity than angiography[25].
Mesenteric angiography is a most accurate radiologic diagnostic tool, but secondary colonic varices could be misinterpreted as an ICV on angiography. Defreyne et al[24] have explained that angiographical diagnosis is in disagreement with the histopathological diagnosis of an arteriovenous malformation probably because the blood passage through the small fistulas is too slow. The same principle can be applied to our case. In about 30% cases, operation revealed secondary causes or changed histopathologic diagnosis as previously described[15-21], suggesting that angiography is an incomplete tool to confirm ICV. Laparoscopy may be a more accurate and definitive diagnostic tool than histology, because histological tissue sampling is very dangerous if not in operation.
The prognosis of ICV seems to be good at all ages compared with cirrhotic varices, which may be related to low pressure in the varices as well as the absence of significant hepatocellular disease[5]. Conservative therapy is sufficient for most ICV patients. Patients with intractable and persistent bleeding may require partial colectomy for involved area.
In conclusion, it is very difficult to diagnose ICV as in our case. The most important thing is to role out secondary causes of varices. In the suspected case, the physician should consider the clinical, radiologic, and surgical information collectively for the proper diagnosis. This case report describes a life-threatening bleeding episode of ICV, mimicking carcinoma in colonoscopy and hemangioma in angiography. ICV can be confirmed by surgical histopathogy, and successfully treated with partial colectomy on involved area.
S- Editor Wang J L- Editor Wang XL E- Editor Bai SH
| 1. | FELDMAN M, SMITH VM, WARNER CG. Varices of the colon. Report of three cases. JAMA. 1962;179:729-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Weingart J, Höchter W, Ottenjann R. Varices of the entire colon-an unusual cause of recurrent intestinal bleeding. Endoscopy. 1982;14:69-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Lieberman DA, Krippaehne WW, Melnyk CS. Colonic varices due to intestinal cavernous hemangiomas. Dig Dis Sci. 1983;28:852-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Villarreal HA, Marts BC, Longo WE, Ure T, Vernava AM, Joshi S. Congenital colonic varices in the adult. Report of a case. Dis Colon Rectum. 1995;38:990-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Iredale JP, Ridings P, McGinn FP, Arthur MJ. Familial and idiopathic colonic varices: an unusual cause of lower gastrointestinal haemorrhage. Gut. 1992;33:1285-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Shrestha R, Dunkelberg JC, Schaefer JW. Idiopathic colonic varices: an unusual cause of massive lower gastrointestinal hemorrhage. Am J Gastroenterol. 1995;90:496-497. [PubMed] |
| 7. | Vella-Camilleri FC, Friedrich R, Vento AO. Diffuse colonic varices: an uncommon cause of intestinal bleeding. Am J Gastroenterol. 1986;81:492-494. [PubMed] |
| 8. | Morini S, Caruso F, De Angelis P. Familial varices of the small and large bowel. Endoscopy. 1993;25:188-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | el-Dosoky MM, Reeders JW, Dol JA, Tytgat GN. Familial intestinal varices without portal hypertension: a case report. Eur J Radiol. 1994;18:140-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Solis-Herruzo JA. Familial varices of the colon diagnosed by colonscopy. Gastrointest Endosc. 1977;24:85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Kori M, Keter D, Grunshpan M, Zimmerman J, Ackerman Z. Familial colonic varices. J Pediatr Gastroenterol Nutr. 2000;30:447-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Place RJ. Idiopathic colonic varices as a cause of lower gastrointestinal bleeding. South Med J. 2000;93:1112-1114. [PubMed] |
| 13. | Schilling D, Maier M, Kohler B, Würmel W, Jakob P, Riemann JF. Idiopathic mesenteric varices causing lower gastrointestinal bleeding. Eur J Gastroenterol Hepatol. 1996;8:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Abraham-Igwe C, Patel R. Idiopathic colonic varices: a case report. Endoscopy. 2002;34:680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Vescia FG, Babb RR. Colonic varices: a rare, but important cause of gastrointestinal hemorrhage. J Clin Gastroenterol. 1985;7:63-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Nikolopoulos N, Xynos E, Datsakis K, Kasapidis P, Vassilakis JS. Varicosis coli totalis: report of a case of idiopathic aetiology. Digestion. 1990;47:232-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Isbister WH, Pease CW, Delahunt B. Colonic varices. Report of a case. Dis Colon Rectum. 1989;32:524-527. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Sugiyama S, Yashiro K, Nagasako K, Sato S, Watanabe K, Igarashi T, Hanyu F, Obata H. Extensive varices of ileocecum. Report of a case. Dis Colon Rectum. 1992;35:1089-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Atin V, Sabas JA, Cotano JR, Madariaga M, Galan D. Familial varices of the colon and small bowel. Int J Colorectal Dis. 1993;8:4-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Beermann EM, Lagaay MB, van Nouhuys JM, Overbosch D. Familial varices of the colon. Endoscopy. 1988;20:270-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Wagner M, Kiselow MC, Keats WL, Jan ML. Varices of the colon. Arch Surg. 1970;100:718-720. [PubMed] |
| 22. | Hawkey CJ, Amar SS, Daintith HA, Toghill PJ. Familial varices of the colon occurring without evidence of portal hypertension. Br J Radiol. 1985;58:677-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Pickens CA, Tedesco FJ. Colonic varices. Unusual cause of rectal bleeding. Am J Gastroenterol. 1980;73:73-74. [PubMed] |
| 24. | Defreyne L, Meersschaut V, van Damme S, Berrevoet F, Robberecht E, Praet M. Colonic arteriovenous malformation in a child misinterpreted as an idiopathic colonic varicosis on angiography: remarks on current classification of childhood intestinal vascular malformations. Eur Radiol. 2003;13 Suppl 4:L138-L141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Gudjonsson H, Zeiler D, Gamelli RL, Kaye MD. Colonic varices. Report of an unusual case diagnosed by radionuclide scanning, with review of the literature. Gastroenterology. 1986;91:1543-1547. [PubMed] |