Published online Apr 28, 2006. doi: 10.3748/wjg.v12.i16.2556
Revised: July 2, 2005
Accepted: July 8, 2005
Published online: April 28, 2006
AIM: To evaluate the efficacy of water supplementation treatment in patients with functional dyspepsia or irritable bowe syndrome (IBS) accompanying predominant constipation.
METHODS: A total of 3 872 patients with functional dyspepsia and 3 609 patients with irritable bowel syndrome were enrolled in the study by 18 Italina thermal centres. Patients underwent a first cycle of thermal therapy for 21 d. A year later patients were re-evaluated at the same centre and received another cycle of thermal therapy. A questionnare to collect personal data on social and
occupational status, family and pathological case history, life style, clinical records, utilisation of welfare and health structure and devices was administered to each patient at basal time and one year after each thermal treatment. Sixty patients with functional dyspepsia and 20 with IBS and 80 healthy controls received an evaluation of gastric output and oro-cecal transit time by breath test analysis. Breath test was performed at basal time and after water supplementaton therapies. Gastrointestinal symptoms were evaluated at the same time points. Breath samples were analyzed with a mass spectometer and a gascromatograph. Results were expressed as T1/2 and T-lag for octanoic acid breath test and as oro-cecal transit time for lactulose breath test.
RESULTS: A significant reduction of prevalence of symptoms was observed at the end of the first and second cycles of thermal therapy in dyspeptic and IBS patients. The analysis of variance showed a real and persistant improvement of symptoms in all patients. After water supplementation for 3 wk a reduction of gastric output was observed in 49 (87.5%) of 56 dyspeptic patients. Both T1/2 and T-lag were significantly reduced after the therapy compared to basal values [91 ± 12 (T1/2) and 53 ± 11 (T-lag), Tables 1 and 2] with results of octanoic acid breath test similar to healthy subjects. After water supplementation for 3 wk oro-cecal transit time was shorter than that at the beginning of the study.
CONCLUSION: Mineral water supplementation treatment for functional dyspepsia or conspipation accompanying IBS can improve gastric acid output and intestinal transit time.
- Citation: Gasbarrini G, Candelli M, Graziosetto RG, Coccheri S, Iorio FD, Nappi G. Evaluation of thermal water in patients with functional dyspepsia and irritable bowel syndrome accompanying constipation. World J Gastroenterol 2006; 12(16): 2556-2562
- URL: https://www.wjgnet.com/1007-9327/full/v12/i16/2556.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i16.2556
Functional dyspepsia and irritable bowel syndrome accompanying predominant constipation (IBSc) are two of the most prevalent diseases in the industrialized world. These disturbances are among the first diseases for a gastroenterologic examination with high social and economical costs. In particular, dyspepsia is the first cause of specialized blood and invasive examination in Europe and USA[1]. Dyspepsia may be organic when associated with specific gastrointestinal or liver diseases. To diagnose functional dyspepsia gastroenterologists need specific criteria known as “Roma criteria”[2]. Prevalence of dyspepsia in general population is variable in different studies between 14% and 41%[3-5]. About 65% of dyspeptic patients result from functional dyspepsia[6]. About 35% of patients with functional dyspepsia present a delayed gastric output which is related to clinical symptoms[7,8] or other disturbances of gastrointestinal motility[9,10]. On the contrary, the link between gastric H pylori infection and functional dyspepsia has not been clarified yet[6] because the data on the effect of H pylori eradication on dyspeptic symptoms are discordant[11,12].
Treatment of dyspepsia is based on drugs that inhibit the gastric acid secretion (such as proton pump inhibitors or H2 blocker agents) or drugs that stimulate gastrointestinal motility (prokinetics agents). However, the efficacy of such therapies is often unsatisfactory in particular for the short duration of the improvement of symptoms. It should be underlined that a prolonged treatment with these drugs is related to a high incidence of side effects. Although there is no scientific evidence, several dietetic regimens have been used in combination with drugs by dyspeptic patients.
A high enrichment of fibers in diet is the first therapeutic steps for constipation[13]. In fact, a high fiber intake is related to an increased fecal mass in healthy subjects (with high interindividual variability)[14,15]. The efficacy of this treatment seems to be time-related, probably for an intestinal adaptation to the high intake of fibers[16]. IBSc is a chronic functional disorder associated with psychological, environmental, emotional, social factors (drugs, stress, lifestyle)[17]. A reduction of water intake may play an important role in the pathogenesis of constipation and water supplementation is often suggested by a general practitioner in clinical practice to IBSc patients[18,19]. Recently, it has been described that an increased water intake up to 1.5 liters of mineral water is able to increase the effect of a diet with fiber enrichment in patients with constipation[20]. In Europe, especially in Italy, Germany and France, a large number of thermal centers stress on the real role of a treatment with thermal mineral water in functional gastrointestinal diseases. For this reason we need international studies or controlled trial to evaluate the effect of mineral water on functional dyspepsia or IBSc. These studies may allow a medical prescription by physicians and evaluate the socio-economical impact on public health systems of these treatments compared to pharmacological therapies. The efficacy of thermal treatment with mineral water on gastrointestinal diseases[21] remains to be further clarified.
This study was to evaluate the economic and health indicators for the assessment of the efficacy of thermal therapies in reducing the health costs. Moreover, the effect of water supplementation therapy on functional dyspepsia and IBSc was also evaluated.
A total of 3 872 patients with functional dysepsia and 3 609 patients with IBSc were enrolled in the study from 1999 to 2000 by the medical staff of 18 thermal centres distributed throughout Italy (Bagni di Lucca, Chianciano, Comano, Franciacorta, Pejo e Rabbi, Recoaro, Sangemini, Sant’Andrea Bagni, San Carlo, S. Elena, SanPellegrino, Sarnano, DI Stabia, Vallio, Vulpacchio, Montecatini, Angolo, Boario). Patients with a history of gastrointestinal, liver, pancreatic, gall bladder, neurological, muscular, rheumatological, autoimmunitary and immunological diseses were excluded from the study. Moreover, patients with severe high blood pressure (diastolic>110, systolic>180), cancer, recent surgical resection, and pregnant women were also excluded from the study. All enrolled patients underwent abdominal ultrasonography and fecal occult blood test. Only patients negative in both tests were enrolled in the study and underwent a first cycle of thermal therapy for a standard period (2 000 mL of mineral water for 21 d). Compliance was evaluated by the percentage of empty bottles returned by patients at the end of the cycle. Before the first cycle of thermal therapy was started, an informed consent was obtained from all enrolled subjects. The anamnestic and clinical data were collected by submitting a questionnaire. The questionnaire included approximately 1 400 closed-answer questions (Table 1) for identifying the exposure variables and risk indicator, with special reference to the social-demographic and clinical variables including different sections (personal data, social and occupational status, family and pathological case history, life style, clinical records and social data, also including indicators of the standard living, utilisation of welfare and health structure and devices). According to the first study plan, the patients were re-examined at the same thermal centre one year after the first therapeutic cycle and received a second cycle of thermal treatment. A second follow-up was made after another year. During the follow-up the effect of the treatment was evaluated by assigning a score on side effects, personal opinion of the treatment and overall tolerability of therapy (Table 1). Moreover a retrospective assessment of the clinical follow-up, drug intake and utilisation of welfare and health service between the first and second cycles was carried out. Statistical analysis was performed using Bowker’s symmetry test and ANOVA to compare uncontinuos variables.
Sixty patients (30 females, 30 males, mean age 44±6 years) with functional dyspepsia and 60 healthy controls (30 males, 30 females, the mean age of 41±5 years) were enrolled. All patients underwent upper digestive endoscopy and abdominal ultrasonography to exclude peptic ulcer disease, gastroesophageal reflux disease, liver, pancreatic and gall bladder diseases. Diagnosis of functional dyspepsia was made based on the Roma II criteria. All patients underwent 13C octanoic acid breath test (OBT) and filled in a questionnaire for evaluation of gastrointestinal symptoms (post-prandial fullness, epigastric pain, bloating, heartburn, nausea, vomiting).
After OBT, all patients started a diet supplemented with mineral water (2 000 mL of mineral water/d for 3 wk). During the mineral water treatment, patients were controlled with a standardized diet (similar caloric and fiber intake)[20]. Compliance to thermal therapy was evaluated by the number of empty bottles returned at the end of the study (20% or more of full bottles returned were considered as the indicator of in adequate compliance). After 3 wk of mineral water supplementation treatment, the OBT was repeated and a new questionnaire for evaluation of gastrointestinal symptoms was administered. Patients after an overnight fasting had 91 mg of 13-C octanoic acid dissolved in an egg with a standardized meal (50 g ham, 150 mL fruit juice, 100 g white bread and 100 mL water) in 10 min. Breath samples were collected in a test tube before and every 15 min for 4 h after ingestion of the labeled substrate.
Analysis of 13C in the breath was performed using a mass spectrometer (Breath Mat; FinniganMat; Bremen, Germany). 0T1/2 and T-lag values were used to express the results after a regression analysis of exhaled air curves. Results were expressed as T1/2 and Tlag. T-test for coupled or uncoupled data was used to compare the difference between groups. Difference in symptoms was evaluated by χ2 test or Fisher’s exact test. P < 0.05 was considered statistically significant.
Twenty patients (10 females, 10 males, mean age 41 ± 5 years) with IBSc and 20 sex and age matched healthy controls (10 females, 10 males, mean age 40 ± 7 years) were enrolled. Diagnosis of IBSc was made based on the Roma II criteria. All patients underwent H2-lactulose breath test (LBT) to evaluate the oro-cecal transit time. Then, all patients started a controlled diet with standard fiber and caloric intake supplemented with 2 000 mL of mineral water. After 3 wk the diet was stopped and LBT was performed. All enrolled patients filled in a questionnaire for evaluation of gastrointestinal symptoms (bloating, hard stools, number of evacuations in a week, incomplete evacuation) before and after mineral water supplementation. Compliance to thermal therapy was evaluated by the number of empty bottles returned at the end of the study (20% or more of full bottles returned were considered as the indicator of in adequate compliance).
LBT was performed after 20 g of lactulose dissolved in 100 mL of water was administered. Breath samples were collected at basal time and every 15 min for 4 h in a specific test tube after the assumption of lactulose. The presence of hydrogen in the breath samples was evaluated by gascchromatography (Quintron Milwaukee, Wisconsin USA). The oro-cecal transit time was evaluated by curves of hydrogen exhaled during the test.
The Student t test for coupled or uncoupled data was used to compare the difference between groups. Difference in symptom prevalence was evaluated by χ2 test or Fisher’s exact test as appropriate. P < 0.05 was considered statistically significant.
A totae of 3 872 patients with functional dyspepsia and 3 069 patients with IBSc were enrolled in the first part of the study. After a year 74% and 69.5% came for follow up visit and to perform a second cycle of thermal therapy (Table 2). No difference among different mineral content of water supplemented was observed.
| Water Type | Pathology | 1st yr | 2nd yr | 3rd yr |
| Dyspepsia | ||||
| Bicarbonate | 1 667 | 966 | 110 | |
| Salse | 1 282 | 979 | 30 | |
| Solfate | 923 | 923 | 24 | |
| Total | 3 872 | 2 868 | 164 | |
| IBSc | ||||
| Bicarbonate | 1 471 | 861 | 59 | |
| Salse | 1 181 | 701 | 19 | |
| Solfate | 957 | 949 | 30 | |
| Total | 3 609 | 2 511 | 108 |
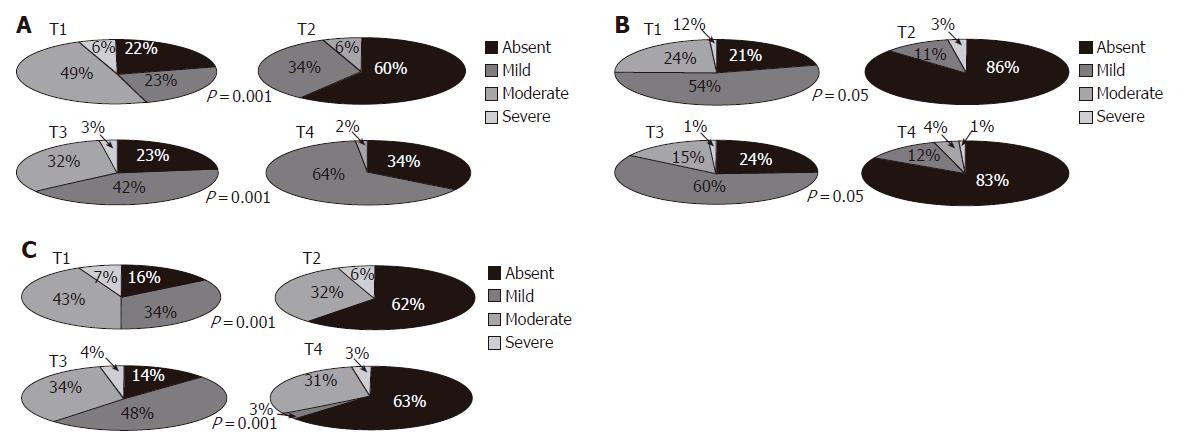
Figures 1A and 1B show the prevalence of dyspeptic symptoms (epigastric pain and post-prandial fullness) during the two cycles of thermal therapy. A significant reduction in the prevalence of dyspeptic symptoms was observed both at the end of the first and second cycles. In particular, 80% of the patients were symptom free after the first cycle of thermal therapy. Moreover, the score during the pretreatment period was similar between the two cycles. However, ANOVA showed reduction of symptoms when the whole follow-up period was considered. Similar results were observed for post-prandial fullness. The analysis of variance showed a real and persistant improvement of symptoms in all patients.
When the main symptoms of IBSc (bloating, hard stools, incomplete evacuation) were considered, significant improvement was observed with ANOVA (Figures 2A-2C).
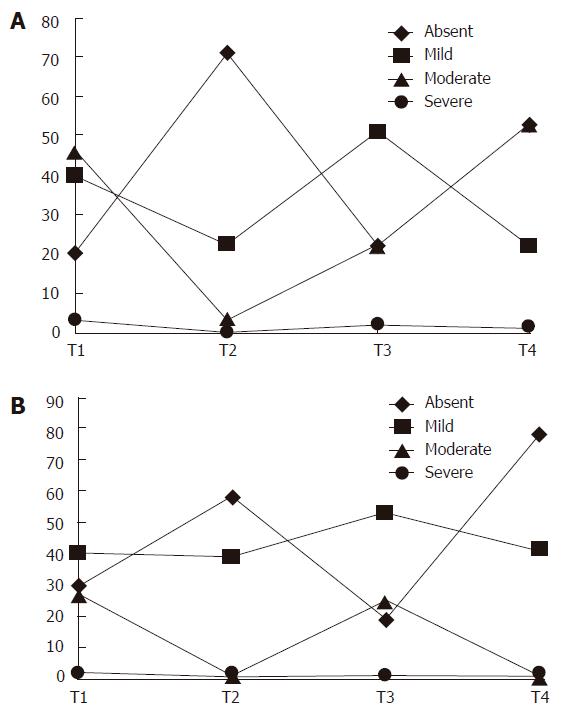
To better underline the temporal evolution of syptoms we reported the mean of scores for symptoms of dyspepsia and IBS at the 4 time points (Figures 3A and 3B).
The data on the number of hospitalization, days of absence from work and the clinical recrudescence before and after two cycles of thermal therapy were decreased by about 30% (Table 3). Moreover, data on overall tolerablity of treatment and reasons of acceptance of this treatment are shown in Table 4. About 80% of patients appreciated the treatment and about 95% gave a positive result of the treatment
| Personal opinions on therapy (%) | Reasons of good opinion (%) | ||
| Excellen | 42 | Care | 95.6 |
| Good | 41.8 | Relax | 68 |
| Lean | 1.2 | Stay | 55.8 |
| Null | 6.3 | Climate | 45.3 |
| No comment | 8.4 | ||
Sixty patients and 60 healthy controls were enrolled in the study. Fifty-eight patients had a slow gastric output measured by OBT (mean T1/2: 131 ± 18; Table 2). Patients with a normal gastric output were excluded. One patient and 2 controls refusing to give their consent were excluded. One patient was excluded for low compliance with the treatment (more than 20% of full bottles returned).
Dyspeptic patients presented an alterated gastric output and a significant difference at enollment compared with healthy controls when both T1/2 (131 ± 18 vs 81 ± 7; P < 0.01) and T-lag (92 ± 11 vs 51±10; P < 0.01) were considered.
After mineral water supplementation for 3 weeks, a reduction of gastric output was observed in 49 (87.5%) of 56 dyspeptic patients. Both T1/2 and T-lag were significantly reduced after the therapy compared to the basal values (91 ± 12 for T1/2 and 53 ± 11 for T-lag, Table 5) with OBT similar to that in healthy controls. In controls and 7 patients, the gastric output did not change after mineral water supplementation treatment.
| Pre-treatment | Post-treatment | P | |
| T1/2 | 131 ± 18 | 91 ± 12 | < 0.001 |
| T-lag | 92 ± 11 | 53 ± 11 | < 0.001 |
The prevalence of dyspeptic symtoms was significantly lower after the therapy than at enrolment. The prevalence of bloating and gastric fullness was significantly lower after mineral water supplementation treatment (Table 6). The overall prevalence of gastrointestinal symptoms was reduced after mineral water supplementation treatment too. At the basal point, a mean global score of symptoms was 15 ± 4. After 30 d of mineral water supplementation treatment, the score was 7 ± 3. A lower prevalence of abdominal pain, nausea, vomiting was also observed. No severe side effects were reported by patients. Only one control experienced mild diarrhea but treatment was not stopped. Five patients and 7 controls reported an increased number of evacuations during treatment. No effects of mineral water supplementation trealment on blood pressure, glycaemic control and heart rate were observed.
| Symptomatology | T0 % (n/n) | T2 % (n/n) | P |
| Gastric fullness | 86 (48/56) | 25 (14/56) | < 0.0001 |
| Epigastric pyrosis | 52 (29/56) | 30 (17/56) | < 0.05 |
| Bloating | 52 (29/56) | 23 (13/56) | < 0.005 |
| Epigastric pain | 24 (12/56) | 11 (6/56) | NS |
| Nausea | 5 (3/56) | 0.2 (1/56) | NS |
| Vomiting | 0.2 (1/56) | 0 (0/56) | NS |
| Overall | 100 (56/56) | 68 (38/56) | < 0.0001 |
Oro-cecal transit time was longer in patients with IBSc than in controls (Table 7). All patients and 3 healthy controls had an abnormal oro-cecal transit time. After minere water supplementation treatment for 3 wk, the oro-cecal transit time was shorter than at the beginning of the study. A slight reduction in transit time was observed in healthy controls especially in those presenting a pathological transit time at the start of the treatment. The number of evacuations in a week was increased and bloating was reduced during mineral water supplementation treatment in patients with IBSc (Table 8). No side effects were reported by patients and controls.
| Pre treatament | Post treatament | P | |
| Patients | 120 ± 12 | 97 ± 8 | < 0.001 |
| Controls | 85.5 ± 14 | 81 ± 8 | NS |
| P | < 0.001 | < 0.001 |
| Symptoms | T0 % (n/n) | T21 % (n/n) | P |
| Bloating | 90 (9/10) | 20 (2/10) | < 0.005 |
| Abdominal Pain | 40 (4/10) | 20 (2/10) | NS |
| T0 Media | T21 Media | ||
| Evacuation/wk (n) | 1.7 | 3.3 | < 0.001 |
Several diseases have been treated with thermal therapies for a long time in different countries. However, whether thermal therapy should be considered as pertinent to alternative medicines is a matter of debate and largely depends on the different cultural settings in which this practice is performed. In the Scandinavian, British and North American countries the therapeutic value and benefits of thermal (spa) treatment are seen with scepticism and looked at as an alternative and unorthodox practice. On the contrary, spa has been considered a credible medical treatment and supported by official undergraduate and postgraduate university teaching in most countries of the continent, Southern and Eastern Europe (France, Germany and Italy). It should also be mentioned that, differently from various forms of alternative medicine, spa therapy is firmly maintained in medical hands and undergoes orthodox medical control. As a consequence, thermal medicine appears as a supportive rather than alternative practice. Thus in the mentioned countries, spa therapy cannot be labelled as “alternative” medicine, but should be defined as “complementary” or “auxiliary” medicine. Nevertheless, also in these settings, an alignment to the Anglo-Saxon scepticism towards spa therapies has recently developed within the medical and academic community, although not all do so among patients and within the “civic” society.
Such scepticism is based on the scant number of studies published in medical journals of good reputation, apt to investigate with correct methodology and design the real benefits of spa therapies in various clinical conditions in term of efficacy and cost-effectiveness. Even in those countries in which “hydrology” is a recognized medical speciality with an academic background (as in Italy) most researcher work done in the past has been characterized by an approach mainly pathophysiologic and pharmacological, aimed at investigating the mechanism and biological effects of the mineral water rather than at assessing the related clinical and health economic effects with appropriate methods.
As in a number of European countries, variable kinds of financial support (public and private) have been provided for different forms of thermal treatment applied to various diseases. This issue is not a simple question of medical and academic relevance but has great implications from the socioeconomic point of view. In Italy, almost 340 thermal industries are crucial economics and social factor for many geographic areas. The yearly financial turnover related to the thermal activities amounts to 300 million dollars and 2 000 million dollars as for health aspects and linked activities, respectively, and is a key element of the national economy.
The evaluation of literature on the efficacy of spa therapies in the international bibliography can clearly show how wide the gap is in this context, if compared to traditional clinical domains and other nonconventional therapies. The limited impact of scientific research on the efficacy of spa therapies accounts the reservations of the scientific world to the actual efficacy of spa therapies, thus paving the way in Italy to discuss the public funding of these activities. On these bases in 1995, the Association of Thermal Industries and Curative Mineral Waters (Federterme”, which officially represents all 340 Italian “medical” spa centres) have developed the epidemiological, health and cost-effectiveness aspects related to spa activities to assess the efficacy of thermal therapies in reducing the health costs.
The observational study has given very important results. The high number of patients who decided to come back for a second period of thermal treatment suggests a very good impact of the therapy on symptoms evaluted by ANOVA test. The data cannot be ascribed only to a placebo effect. We however, cannot conclude that thermal therapies are able to influence the natural history of studied diseases (dyspepsia and IBSc). It is possible that the beneficial effet of a single thermal treatment can influence the perception of symptoms as less severe even in a long follow-up period. This hypotesis was supported by reduction of day and number of hospitalization and day of absence by work during the follow-up period. It should be important to evaluate the economical impact of such results but it was not possible in this study. However, all cited parameters showed a reduction of about one third during the follow-up perion when compared to the former years. No reduction in drug use was observed (data not shown). It is possible to conclude that mineral water supplementation treatment for functional dyspepsia and IBSc can improve symptoms and reduce the medical cost as well as deserves further attentions. However, a best detailed analysis on cost/effectiveness should be performed.
Our data showed that mineral water supplementation therapy could reduce the gastric output of solid food and improve symptoms in patients with functional dyspepsia. The improvement of both studied parameters (T1/2 and Tlag) suggests that mineral water can normalize both gastric output time and redistribution of alimentary bolus in the stomach. The pathophysiologic mechanism causing these effects are unknown. Our study demonstrated that mineral water supplementation therapy could improve symptoms and gastric acid output in functional dyspeptic patients evaluated by a questionnaire and OBT. The effects exerted by mineral water include stimulation of chemoreceptors and baroceptors in the gastric walls. The well known effect of water on intestinal motility (due to osmotic properties) with increased intestinal transit time induces an early duodenal transit of food with an earlier relaxation of pylorus and a faster transit of bolus from stomach to duodenum. Moreover, the presence of liquid in the stomach accelerates food disintegration and solubilization.The chemical content of particular water plays a role in the stimulation of specific gastric receptors that increases the gastric motility by secreting local hormones (gastrin, secretin, vasoactive intestinal peptide). The evidence that the effect of water is limited in patients suggests that hormones may be dysrequlated in such patients. The presence of large amounts of calcium and magnesium in mineral water may directly stimulate the gastric smooth muscle to increase its motility and relax pylorus, thus producing its effect on gastric output and symptoms. The restoration of a correct gastric output reduces the time of exposition of bolus to intestinal bacteria, thus reducing the intensity of bloating due to intestinal bacteria overgrowth.
Constipation predominant irritable bowel sindrome is one of the frequent gastroenterological diseases in general population. Several pharmacological treatments have been proposed and used. Although therapies for constipation are efficacious, most of them are self-prescribed by patients with a high cost. Laxatives for example are widely used without medical control and may produce side effects. Moreover, the efficacy of laxative treatment is temporary and induces patients to increase dosage of drugs. A diet containing high fibers has been demonstrated to be a valid alternative to drugs for chronic constipation[20].
In our study, mineral water supplementation theray (2 000 mL) for 3 wk accelerated oro-cecal transit time and improved symptoms in patients with IBSc. Compliance to therapy was excellent. The mechanisms of action of mineral water are not completely clear. Others iones present in mineral water may directly or indirectly (via neuroendocrine secretion of vasointestinal active peptides) stimulate smooth muscle to increase its motility. These actions reduce the transit time and increase the number of evacuations in a day with improvement of symptoms in IBSc patients. The decreased transit time improves bloating and reduces the time of contact between intestinal content and saprophytic flora with reduction in gas production.
In conclusion, mineral water supplementation theray can improve gastiric acid output, oro-cecal transit time and symptoms in patients with functional dyspepsia or IBSc. Mineral water supplementation therapy seems to be a simple, well-tolerated, cheap therapy for functional dyspepsia or IBSc and should be taken into account by physicians in the treatment of dyspepsia ad IBSc.
S- Editor Wang J L- Editor Wang XL E- Editor Bi L
| 1. | Morrissey JF, Reichelderfer M. Gastrointestinal endoscopy (2). N Engl J Med. 1991;325:1214-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Colin-Jones DG. The management of dyspepsia. Scand J Gastroenterol Suppl. 1988;155:96-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Talley NJ, Weaver AL, Zinsmeister AR, Melton LJ 3rd. Onset and disappearance of gastrointestinal symptoms and functional gastrointestinal disorders. Am J Epidemiol. 1992;136:165-177. [PubMed] |
| 4. | Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ 3rd. Dyspepsia and dyspepsia subgroups: a population-based study. Gastroenterology. 1992;102:1259-1268. [PubMed] |
| 5. | Jones RH, Lydeard SE, Hobbs FD, Kenkre JE, Williams EI, Jones SJ, Repper JA, Caldow JL, Dunwoodie WM, Bottomley JM. Dyspepsia in England and Scotland. Gut. 1990;31:401-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 279] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Shaib Y, El-Serag HB. The prevalence and risk factors of functional dyspepsia in a multiethnic population in the United States. Am J Gastroenterol. 2004;99:2210-2216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 112] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Wegener M, Börsch G, Schaffstein J, Reuter C, Leverkus F. Frequency of idiopathic gastric stasis and intestinal transit disorders in essential dyspepsia. J Clin Gastroenterol. 1989;11:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 48] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Corinaldesi R, Stanghellini V, Raiti C, Rea E, Salgemini R, Barbara L. Effect of chronic administration of cisapride on gastric emptying of a solid meal and on dyspeptic symptoms in patients with idiopathic gastroparesis. Gut. 1987;28:300-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 138] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Camilleri M, Brown ML, Malagelada JR. Relationship between impaired gastric emptying and abnormal gastrointestinal motility. Gastroenterology. 1986;91:94-99. [PubMed] |
| 10. | Labò G, Bortolotti M, Vezzadini P, Bonora G, Bersani G. Interdigestive gastroduodenal motility and serum motilin levels in patients with idiopathic delay in gastric emptying. Gastroenterology. 1986;90:20-26. [PubMed] |
| 11. | Blum AL, Talley NJ, O'Moráin C, van Zanten SV, Labenz J, Stolte M, Louw JA, Stubberöd A, Theodórs A, Sundin M. Lack of effect of treating Helicobacter pylori infection in patients with nonulcer dyspepsia. Omeprazole plus Clarithromycin and Amoxicillin Effect One Year after Treatment (OCAY) Study Group. N Engl J Med. 1998;339:1875-1881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 280] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 12. | McColl K, Murray L, El-Omar E, Dickson A, El-Nujumi A, Wirz A, Kelman A, Penny C, Knill-Jones R, Hilditch T. Symptomatic benefit from eradicating Helicobacter pylori infection in patients with nonulcer dyspepsia. N Engl J Med. 1998;339:1869-1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 297] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 13. | Badiali D, Corazziari E, Habib FI, Tomei E, Bausano G, Magrini P, Anzini F, Torsoli A. Effect of wheat bran in treatment of chronic nonorganic constipation. A double-blind controlled trial. Dig Dis Sci. 1995;40:349-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 77] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Müller-Lissner SA. Effect of wheat bran on weight of stool and gastrointestinal transit time: a meta analysis. Br Med J (Clin Res Ed). 1988;296:615-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 142] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Cummings JH. Constipation, dietary fibre and the control of large bowel function. Postgrad Med J. 1984;60:811-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 71] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Read NW. Dietary fiber and the gut: action in gastrointestinal disorders in Sleisenger MH, and Fordtran JS (eds). Gastrointestinal Disease: Pathophisiology, Diagnosis, Management, 5th ed. Philadelphia: WB Saunders 1993; 288-296. |
| 17. | Devroede G. constipation in Sleisenger MH, and Fordtran JS (eds). Gastrointestinal Disease: Pathophisiology, Diagnosis, Management, 5th ed. Philadelphia: WB Saunders 1993; 837-887. |
| 18. | Alessi CA, Henderson CT. Constipation and fecal impaction in the long-term care patient. Clin Geriatr Med. 1988;4:571-588. [PubMed] |
| 19. | Sàez LR. Therapeutic proposals for the treatment of idiopathic constipation. Ital J Gastroenterol. 1991;23:30-35. [PubMed] |
| 20. | Anti M, Pignataro G, Armuzzi A, Valenti A, Iascone E, Marmo R, Lamazza A, Pretaroli AR, Pace V, Leo P. Water supplementation enhances the effect of high-fiber diet on stool frequency and laxative consumption in adult patients with functional constipation. Hepatogastroenterology. 1998;45:727-732. [PubMed] |