Published online Mar 28, 2006. doi: 10.3748/wjg.v12.i12.1975
Revised: June 2, 2005
Accepted: June 8, 2005
Published online: March 28, 2006
Mucinous cystadenoma of the appendix is a rare condition and represents one of the three entities with the common name mucocele of the appendix. It is characterized by a cystic dilatation of the lumen with stasis of mucus inside it. Histopathologically mucocele is divided into three groups: focal or diffuse mucosal hyperplasia, mucinous cystadenoma and mucinous cystadenocarcinoma. This condition is often associated with other neoplasia, especially adenocarcinoma of the colon and ovaries. We here describe a 57 year old male patient who presented with abdominal discomfort, constipation, fresh blood in stool and frequent urination. He had a big cystadenoma of the appendix associated with adenocarcinoma of the colon and hepatocellular carcinoma of the liver. The patient underwent right haemicolectomy, sigmoid colon resection and segmental resection of the liver. Now 3 years later he has no evidence of disease relapse. According to this, we stress the need of accurate preoperative diagnosis and intraoperative exploration of the whole abdomen in these patients.
- Citation: Djuranovic SP, Spuran MM, Kovacevic NV, Ugljesic MB, Kecmanovic DM, Micev MT. Mucinous cystadenoma of the appendix associated with adenocarcinoma of the sigmoid colon and hepatocellular carcinoma of the liver: Report of a case. World J Gastroenterol 2006; 12(12): 1975-1977
- URL: https://www.wjgnet.com/1007-9327/full/v12/i12/1975.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i12.1975
Mucocele of the appendix is a common name for three different entities with similar clinical presentations. Its main characteristic is cystic dilatation of the appendiceal lumen with mucus inside it. Focal or diffuse mucosal hyperplasia and mucinous cystadenoma are of benign nature, but could lead to complications due to rupture, invasion to adjacent organs or recurrence. Mucinous cystadenocarcinoma is a malignant disease and pseudomyxoma peritonei is its worst complication. On the other hand, this condition is often associated with other intra-abdominal neoplasia. According to this, it is necessary to apply strict oncologic principles for resection in order to minimize the possible complications. A correct preoperative diagnosis may help to avoid iatrogenic rupture during surgery and missing the possible associated intra-abdominal tumors. We describe here a case of correct preoperative diagnosis of big appendiceal mucinous cystadenoma associated with adenocarcinoma of the sigmoid colon and hepatocellular carcinoma of the liver.
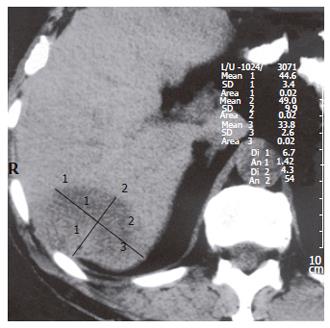
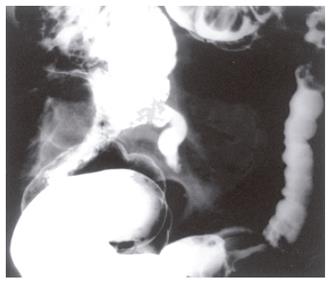
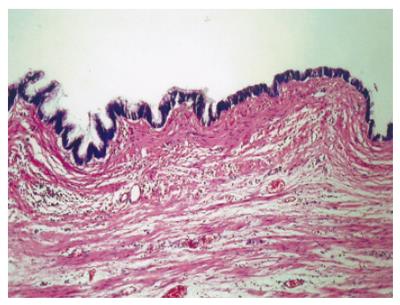
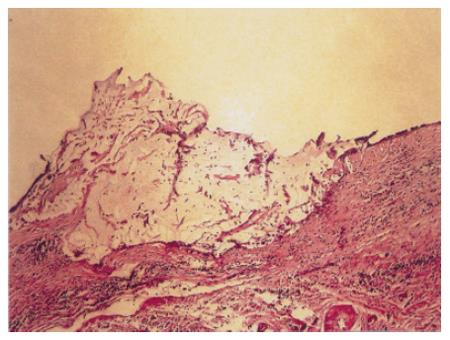
The patient was male, 57 years old with pain in ileo-cecal region for 6 mo prior to administration. He had abdominal discomfort, constipation, fresh blood in stool and frequent urination. On physical examination he had palpable tumor mass in the lower right quadrant of abdomen, enlarged liver and subicterus of sclera. Laboratory findings showed inflammatory syndrome with sideropenic normocytic anemia, elevated alkaline phosphatase, carcinoembryonic antigen, carboanchidratic 19-9 antigen and alpha-feto protein. He had negative markers for hepatotropic viruses (B and C). Transabdominal sonography showed the presence of a large bilocular cystic tumor in the right lower quadrant of abdomen with outlined capsule and maximal dimensions of 106 mm × 74 mm, slightly enlarged liver with focal hyperechogenous tumor in the 6th and 7th liver segments (maximal diameter of 67 mm) and “pseudokidney” sign in the left lower quadrant of abdomen. CT scan displayed tumor of the right liver lobe (Figure 1). Barium enema showed extra luminal compression and medial displacement of cecum and terminal ileum with appendix not filled with the contrast and 4-cm long tubular stenosis of the proximal part of sigmoid colon (Figure 2). According to that we suspected that it was the mucocele of the appendix with neoplasia of the sigmoid colon and hepatic tumor. The patient underwent right haemicolectomy with ileo-transverso termino-lateral anastomosis and sigmoid colon resection with colo-recto termino-terminal anastomosis as well as paraaortal and paracaval lymphadenectomy. Segmetal resection of the liver (the 6th and 7th segments) was done and the whole tumor was resected. Histology showed big mucocele of the appendix caused by mucinous cystadenoma with severe displasia (Figure 3 and Figure 4), adenocarcinoma of the sigmoid colon (T3,N1,M0,L1,V0; Dukes C; Astler-Coller C-2) and carcinoma hepatis hepatocellulare (well-differentiated alveolar type). Adjuvant therapy with 5-fluorouracile and Leucovorine was administrated in five cycles. Now, three years later, the patient is doing well and has gained 17 kilograms with no evidence of disease relapse and his laboratory findings including tumor markers are within the normal range.
Mucocele of the appendix is a descriptive term that implies a dilated appendiceal lumen caused by abnormal accumulation of mucus. Mucocele is found in 0.2-0.3% of all appendectomy specimens. The male:female ratio is 1:4 and the mean age of patients is around 55 years[1,2]. Post-imflammatory obstruction was initially thought to be the main reason for the majority of mucoceles, but recent evidence suggests that neoplasia is the basis of most of these cases. The understanding of the nature of appendiceal mucocele and its terminology has been greatly changed since the initial description of Rokitansky in 1842[3] and Higa et al[4] in 1973. Appendiceal mucocele can be histologically divided into three groups: focal or diffuse mucosal hyperplasia without epithelial atypia, mucinous cystadenoma with some degree of epithelial atypia and mucinous cystadenocarcinoma. A large series of hyperplasia were found in 24.7% cystadenoma, 63% cystadenocarcinoma and 12.3 % of all cases[1,2,4]. Our case could be regarded as mucinous cystoadenoma with severe dysplasia.
Peritoneal (and/or retroperitoneal and pleural) pseudomyxoma is regarded as a worst complication of this disease which could have metastatic characteristics in case of mucinous adenocarcinoma. It is well known that this entity is often associated with colorectal carcinoma (11-20%), ovarian mucinous cystadenoma, uterine myoma, carcinoma of the pancreas and carcinoid tumor of the appendix[4]. Our patient is interesting because of the two associated tumors while one of them (hepatocellular carcinoma) has not so far been mentioned in literature in association with mucinous cystadenoma.
Clinical symptomatology of these patients is not specific. Abdominal pain is present in 64% of the patients and palpable ileo-cecal mass in 50% of them. Disease course is asymptomatic in 25% of the patients even when they have large tumors. Urinary infection and haematuria are often associated (20%)[5]. Intestinal obstruction caused by intussusception and intestinal bleeding are rare complications[6]. Our patient had a long history of abdominal pain, blaunting, subicterus and urinary discomfort, constipation and rectal bleeding. Some of these symptoms are due to associated tumors.
Laboratory findings are usually non specific, but the elevation of tumor marker level often indicates neoplastic origin and/or associated tumors, which was seen in our patient.
Correct and complete preoperative diagnosis was rare in the past, but modern techniques of imaging allow us today to recognise most of the complications and associated conditions[7]. Sonography usually shows a cystic encapsulated lesion with liquid content adjacent to cecum. CT/NMR scan shows a low density, encapsulated, thin-walled mass that does not contain contrast medium and communicates directly with the cecum. Other solid or cystic abdominal and peritoneal tumors could also be visualised by these methods. Barium enema could point out a failure of the appendix to fill with contrast medium and signs of the extra luminal compression in the ileo-cecal region[8,9]. The "sign of volcano" is a pathognomonic colonoscopy finding[8,9]. We could not perform total colonoscopy due to neoplastic stenosis of the sigmoid colon.
Fine needle aspiration biopsy is not recomended because of great risk of pseudomyxoma dissemination.
Classical surgical approach is the best therapy option with intraoperative abdominal cavity exploration because of the already stressed associated tumors. Appendectomy is advised for focal or diffuse mucosal hyperplasia and cystadenoma when the appendiceal base is intact. Cecal resection is performed for cystadenoma with a large base and right colectomy is recommended for cystadenocarcinoma. Other surgical procedures depend upon the existence of associated tumors. In cases of disseminated pseudomyxoma peritonei, ultrasonic surgical aspirator can be used[10,11]. Laparoscopic approach to cystadenoma of the appendix is safe if surgery can be performed without grasping the lesion and if the specimen is removed through the abdominal wall using a bag[12].
The five-year survival rate is 100% in cases of benign mucocele and about 45% in malignant cases. Radiotherapy, chemotherapy and new therapeutic modalities (radioimmunotherapy and matrix metalloproteinase inhibitors) have still to be proven by prospective analysis[13].
In conclusion, accurate preoperative diagnosis and intraoperative exploration of the whole abdomen can improve the prognosis of patients with appendiceal mucocele.
The authors thank Professor Božina Radević, PhD, surgeon, Institute for Cardiovascular Diseases Dedinje, Belgrade and Professor Ivan Boričić, PhD, pathologist, Institute for Pathology, Belgrade, for their kind help.
S- Editor Guo SY L- Editor Wang XL E- Editor Bai SH
| 1. | Kim SH, Lim HK, Lee WJ, Lim JH, Byun JY. Mucocele of the appendix: ultrasonographic and CT findings. Abdom Imaging. 1998;23:292-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 77] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Krebs TL, Daly BD, Wong-You-Cheong JJ, Grumbach K. General case of the day. Mucinous cystadenocarcinoma of the appendix. Radiographics. 1998;18:1049-1050. [PubMed] |
| 3. | Rokitansky CF; A manual of pathological anatomy. Vol.2. English translation of the Vienna edition (1842). Philadelphia: Blancard and Lea 1855; 89. . |
| 4. | Higa E, Rosai J, Pizzimbono CA, Wise L. Mucosal hyperplasia, mucinous cystadenoma, and mucinous cystadenocarcinoma of the appendix. A re-evaluation of appendiceal "mucocele". Cancer. 1973;32:1525-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Minni F, Petrella M, Morganti A, Santini D, Marrano D. Giant mucocele of the appendix: report of a case. Dis Colon Rectum. 2001;44:1034-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Jones CD, Eller DJ, Coates TL. Mucinous cystadenoma of the appendix causing intussusception in an adult. Am J Gastroenterol. 1997;92:898-899. [PubMed] |
| 7. | Scotté M, Laquerrière A, Riff Y, Majerus B, Manouvrier JL, Leblanc I, Michot F, Hémet J, Ténière P. [Appendiceal mucoceles. Pathophysiology and therapeutic indications]. J Chir (Paris). 1994;131:303-312. [PubMed] |
| 8. | Madwed D, Mindelzun R, Jeffrey RB Jr. Mucocele of the appendix: imaging findings. AJR Am J Roentgenol. 1992;159:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 91] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Isaacs KL, Warshauer DM. Mucocele of the appendix: computed tomographic, endoscopic, and pathologic correlation. Am J Gastroenterol. 1992;87:787-789. [PubMed] |
| 10. | Keating JP, Frizelle FA. Use of ultrasonic surgical aspirator in operative cytoreduction of pseudomyxoma peritonei. Dis Colon Rectum. 2000;43:559-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Zagrodnik DF 2nd, Rose DM. Mucinous cystadenoma of the appendix: diagnosis, surgical management, and follow-up. Curr Surg. 2003;60:341-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Navarra G, Asopa V, Basaglia E, Jones M, Jiao LR, Habib NA. Mucous cystadenoma of the appendix: is it safe to remove it by a laparoscopic approach. Surg Endosc. 2003;17:833-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Stevens KJ, Dunn WK, Balfour T. Pseudomyxoma extraperitonei: a lethal complication of mucinous adenocarcinoma of the appendix. Am J Gastroenterol. 1997;92:1920-1922. [PubMed] |