Published online Mar 21, 2006. doi: 10.3748/wjg.v12.i11.1793
Revised: October 30, 2005
Accepted: December 7, 2005
Published online: March 21, 2006
A 62-year-old male with decompensated liver cirrhosis due to hepatitis C virus developed severe hepatic encephalopathy with status epileptic us. The blood ammonia level on admission was more than twice the normal level. Brain computed tomography and magnetic resonance imaging were normal. In addition, electroencephalogram showed diffuse sharp waves, consistent with hepatic encephalopathy. The status epilepticus was resolved after antiepileptic therapy (phenytoin sodium) and treatment for hepatic encephalopathy (Branched chain amino acids). The blood ammonia level normalized with the clinical improvement and the patient did not have a recurrence of status epilepticus after the end of the antiepileptic treatment. Additionally, the electroencephalogram showed normal findings. Thus, we diagnosed the patient as hepatic encephalopathy with status epilepticus. We consider the status epilepticus of this patient to a rare and interesting finding in hepatic encephalopathy.
- Citation: Tanaka H, Ueda H, Kida Y, Hamagami H, Tsuji T, Ichinose M. Hepatic encephalopathy with status epileptics: A case report. World J Gastroenterol 2006; 12(11): 1793-1794
- URL: https://www.wjgnet.com/1007-9327/full/v12/i11/1793.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i11.1793
Hepatic encephalopathy typically presents with alterations in behavior, impairment of consciousness, and alterations in motor tone[1]. Although, according to some reports, the incidence of seizures in patients with hepatic encephalopathy is unknown, reports of epileptic seizures in patients with hepatic encephalopathy during the clinical course are very rare, but not in the terminal stage of liver cirrhosis[2-4]. We present a rare and interesting case of a 62-year-old male with hepatic encephalopathy with status epilepticus accompanying decompensated liver cirrhosis.
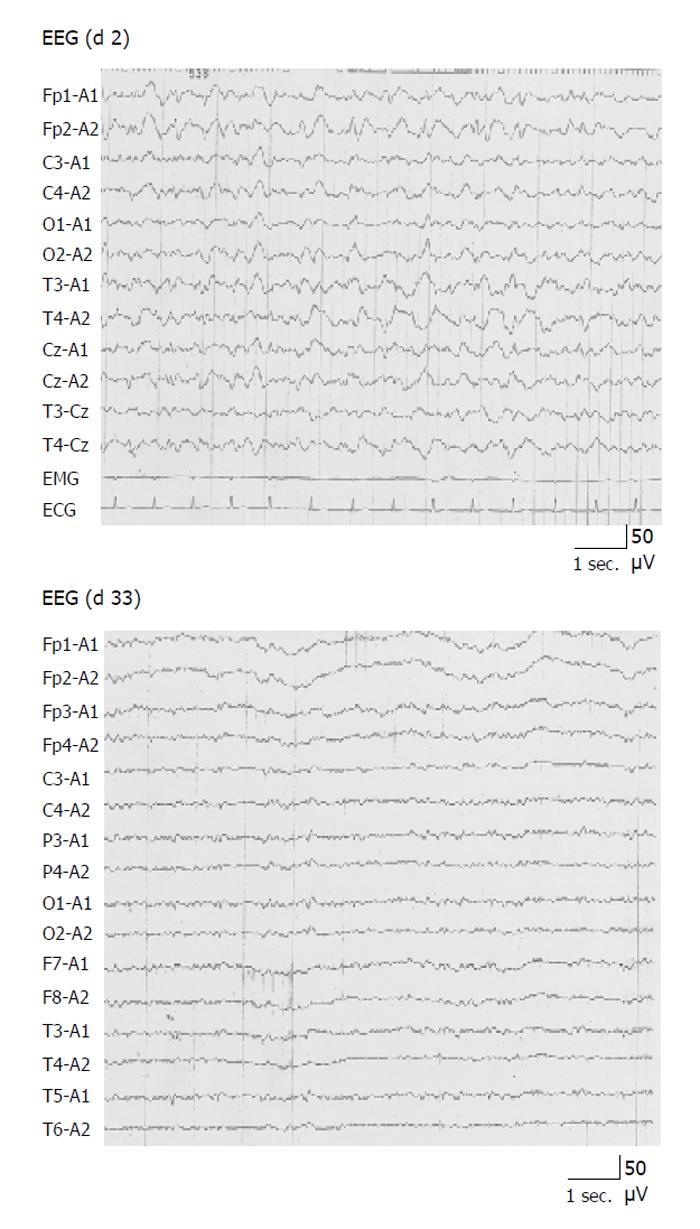
A 62-year-old patient was diagnosed as having decom-pensated liver cirrhosis due to hepatitis C virus one year earlier. At that time he reported a ten-year history of mild psychosis but no history of diabetes mellitus, epilepsy, stroke, or brain trauma. He was admitted to our hospital because of generalized tonic-clonic seizures for several hours and loss of consciousness (status epilepticus) in October 2004. He had a history of recurrent episodes of hepatic encephalopathy. The results of further clinical examination, except for signs of decompensated liver cirrhosis, were normal. Laboratory data showed anemia, thrombopenia, increased transaminase, alkaline phosphatase and total bilirubin, and decreased albumin, total cholesterol and BTR (branched chain amino acid/tyrosine ratio). Furthermore, the plasma ammonia (NH3) level on admission was twice the normal level (186 μmol/L; normal value is 23-76 μmol/L). Chest and abdominal roentgenograms, brain computed tomography (CT) and magnetic resonance imaging (MRI) were also normal, although abdominal echosonography and CT revealed atrophic cirrhotic liver and splenomegaly. Electroencephlogram (EEG) on day 2 after admission showed diffuse sharp waves, consistent with hepatic encephalopathy (Figure 1). According to the history and the results of EEG, in combination with laboratory and radiological data, hepatic encephalopathy with status epilepticus was suspected. Status epilepticus and loss of consciousness were resolved after antiepileptic therapy (phenytoin sodium) and treatment for hepatic encephalopathy (branched chain amino acids; BCAA). The plasma NH3 level returned to a normal level concurrently with his clinical improvement. He did not have a recurrence of status epilepticus after the end of antiepileptic treatment and his conscious level returned to normal with continuous therapy for hepatic encephalopathy with BCAA. Another EEG on day 33 after admission showed a normal level (Figure 1). Thus, we diagnosed our patient as having hepatic encephalopathy with status epilepticus. In the follow-up, 7 mo later, he was in good condition, in spite of the recurrence of hepatic encephalopathy.
The present case was diagnosed as hepatic encephalopathy with status epilepticus. Although the patient had a history of mild psychosis, there were no psychological findings except for the loss of consciousness at the time the seizures occurred. In addition, he had a history of recurrent episodes of hepatic encephalopathy. Second, no focal brain lesion could be detected by brain CT and MRI, and the EEG was suggestive of metabolic dysfunction, especially hepatic encephalopathy. Third, the elevated plasma NH3 level and EEG findings (diffuse sharp waves) on admission and its subsequent normalization with the clinical improvement after the end of antiepileptic treatment strongly suggested hepatic encephalopathy with status epilepticus.
Epileptiform abnormalities in EEG, seizures and status epilepticus may be seen in patients with hepatic encephalopathy, although their incidence is unknown. Ficker DM et al. reported in a retrospective study that the majority of cirrhotic patients with epileptiform changes in EEG either died or deteriorated[3]. However, reports of epileptic seizures in hepatic encephalopathy during the clinical course are very rare[5,6].
The pathophysiology of seizures in hepatic ence-phalopathy remains unknown. Various metabolic factors may be suggested. The plasma NH3 levels are consistently elevated, while other factors, such as short chain free fatty acids, phenols, mercaptanes and false neurotransmitters, have also been implicated. These factors may be respon-sible for the generation of epileptiform discharges as well as epileptic seizures in patients with hepatic enc-ephalopathy[7,8].
On the other hand, it has been reported that the focal hyperemia/hypermetabolism may be related either to the seizures or to the encephalopathy itself, based on intracranial ultrasonography and single-photon-emission computed tomography (SPECT)[6].
S- Editor Pan BR and Wang J L- Editor Zhang JZ E- Editor Wu M
| 1. | Rothstein JD, Herlong HF. Neurologic manifestations of hepatic disease. Neurol Clin. 1989;7:563-578. [PubMed] |
| 2. | Sherlock S. Hepatic encephalopathy. In: S. Sherlock, J Dooley eds. Diseases of the liver and billiary system. 10th ed. Oxford:. Blackwell. 1997;91-92. |
| 3. | Ficker DM, Westmoreland BF, Sharbrough FW. Epileptiform abnormalities in hepatic encephalopathy. J Clin Neurophysiol. 1997;14:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Eleftheriadis N, Fourla E, Eleftheriadis D, Karlovasitou A. Status epilepticus as a manifestation of hepatic encephalopa-thy. Acta Neurol Scand. 2003;107:142-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Annoni JM, Giostra E, Goumaz M, Slosman D, Hadengue A, Mentha G. Focal hepatic encephalopathy with status epile-pticus: incomplete recovery after hepatic transplantation. Dig Dis Sci. 1997;42:792-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Wszolek ZK, Aksamit AJ, Ellingson RJ, Sharbrough FW, Westmoreland BF, Pfeiffer RF, Steg RE, de Groen PC. Epileptiform electroencephalographic abnormalities in liver transplant recipients. Ann Neurol. 1991;30:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Bickford RG, Butt HR. Hepatic coma: the electroencephalographic pattern. J Clin Invest. 1955;34:790-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 197] [Article Influence: 9.0] [Reference Citation Analysis (0)] |