Published online Jan 7, 2006. doi: 10.3748/wjg.v12.i1.146
Revised: May 28, 2005
Accepted: June 2, 2005
Published online: January 7, 2006
We present herein a case report of sigmoidorectal intussusception as an unusual case of sigmoid adenomatous polyp. The patient was a 56-year-old man who suffered from rectal bleeding for one day. He initially visited his general practitioner and was diagnosed as having an intraluminal mass of 15 cm from the anal verge. Several hours after admission to our coloproctology clinic, he suddenly presented with lower abdominal cramping pain with rectal bleeding during his bowel preparation using polyethylene glycol electrolyte solution. An emergency colonoscopy revealed that the invaginated colon with polypoid mass was protruded to the lower rectum. Gastrograffin enema showed that the invaginated bowel segment was 3 cm from the anal verge. CT scan showed the typical finding of intussusception. We performed laparoscopic anterior resection and anastomosis after the sponge-on-the-stick-assisted manual reduction. The permanent pathologic finding showed villotubular adenoma of the sigmoid colon.
- Citation: Park KJ, Choi HJ, Kim SH, Han SY, Hong SH, Cho JH, Kim HH. Sigmoidorectal intussusception of adenoma of sigmoid colon treated by laparoscopic anterior resection after sponge-on-the-stick-assisted manual reduction. World J Gastroenterol 2006; 12(1): 146-149
- URL: https://www.wjgnet.com/1007-9327/full/v12/i1/146.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i1.146
Adenomatous polyp of the colon is quite a common disease, but its presentation as intussusception is very rare. The diagnosis of the underlying lesion in adult intussusception is often difficult, and it is commonly established only after surgical exploration. However, a modern imaging technique, CT, can be helpful in the precise preoperative identification of the etiology of the intussusception[1,2]. Although surgical resection is generally indicated in most adult intussusceptions, it is still controversial whether or not the sigmoidorectal intussusception should be reduced before resection. We present here a rare case of large villotubular adenoma of the sigmoid colon as a cause of sigmoidorectal intussusception, and it was treated by laparoscopic anterior resection after a manual reduction using our own technique.
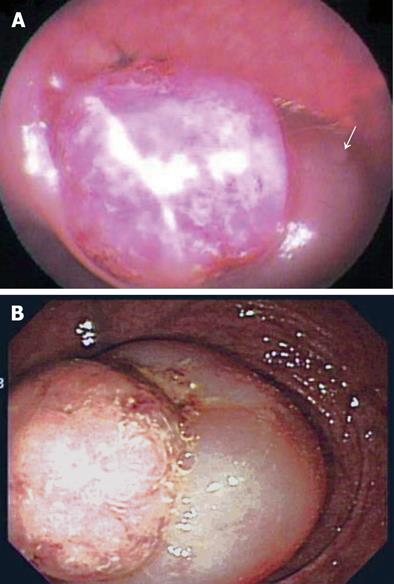
A 56-year-old male was referred by his general practitioner to our Coloproctology Clinic for further evaluation and management of an intraluminal rectal mass with intermittent rectal bleeding for one day. The sodium phosphate enema (Fleet® Enema; CB Fleet Co, Lynchburg, VA, USA) was used for bowel preparation for sigmoidoscopy in the local clinic. The local practitioner finished the sigmoidoscopy without any complications and gave a presumptive diagnosis of rectal mass with partial downward displacement of involved bowel. The rectal mass was detected at 15 cm from anal verge upon flexible sigmoidoscopy (Figure 1A), and the local practitioner did not explore the entire colon beyond the lesion. Several hours after his admission, he suddenly had lower abdominal cramping pain with rectal bleeding during bowel preparation using polyethylene glycol electrolyte solution. A digital rectal examination palpated a protuberant mass-like lesion with a smooth surface. An emergency colonoscopy revealed a sausage-like protrusion at the rectum about 3 cm proximal to the anal verge (Figure 1B), and our initial endoscopic diagnosis was nongangrenous sigmoidorectal intussusception that was caused by a polyp. A CT scan of the pelvis was performed to obtain a detailed delineation of the lesion. The CT showed a round target-shaped mass lesion consistent with intussusception, and the leading lesion was thought to be a benign mass with a low likelihood of malignancy (Figure 2). Our clinical impression was sigmoidorectal intussusception secondary to benign adenomatous polyp of the sigmoid colon. For the next step, we tried a contrast study using gastrograffin for the reduction as well as for the diagnostic imaging of the intussusception. This also showed an invaginated bowel segment at the lower rectum about 3 cm proximal to the anal verge (Figure 3), and a hydrostatic pressure was given via the rectum for reduction, but it was in vain.
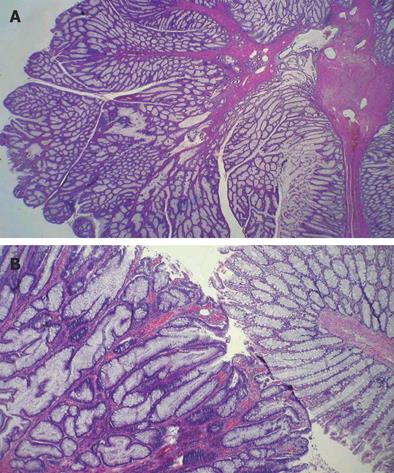
After the general anesthesia, he was placed supine in the modified lithotomy position using Dan Allen stirrups. After the insertion of the umbilical port for the establishment of pneumoperitoneum, surgery was begun in the Trendelenburg position. On laparoscopic exploration, the neck or commencement of the intussusception was located at the rectosigmoid junction, but the distal end was not identified in the peritoneal cavity. The rectal wall of the involved segment was mildly edematous, but it was otherwise healthy on gross examination. No other intra-abdominal pathologic findings were detected. For the manual reduction of the intussusception, we tried to push up the distal end of invaginated segment with a lubricated sponge-on-the-stick from the anus while monitoring by a laparoscope. This maneuver made it possible to laparoscopically visualize the distal end of the intussusception in the pelvic cavity. We then pulled the intussuscepted segment out proximally using a laparoscopic bowel grasper, but this trial failed. We next tried manual reduction again by grasping the upper ring fold of the intussusception steadily by the index and middle fingers of the surgeon through a suprapubic vertical midline incision 4 cm in length while simultaneously pushing the lowest segment up using a lubricated sponge-on-the-stick via the anus; in this fashion we were successful in reducing the intussuscepted segment. The leading point of the intussusception was located in the mid-sigmoid colon. We performed laparoscopic anterior resection on an oncologic basis because the pathology of the mass had not been confirmed as being benign. After the resection of the segment, the specimen was extracted via the previous suprapubic vertical midline incision. The bowel continuity was safely restored using a standard double-stapling technique between the descending colon and midrectum. The final pathologic diagnosis was villotubular adenoma of the sigmoid colon measuring 2.5 cm × 2 cm in size (Figure 4). The patient was discharged from the hospital 8 d after the operation without any complications.
Intussusception is a quite different entity in adults from that found in children. An organic etiology is found in 70%-90% of adult intussusceptions, and primary or secondary malignant neoplasia are documented in about 20%-50% of adult intussusceptions[3-5]. In particular, intussusception occurring in large bowel is more likely to have a malignant etiology[4]. Large polypoid adenomas and lipomas are the most common benign leading points found in adult colocolic intussusception[5,6]. Most reported cases of sigmoido-recto-anal intussusception in the literature are caused by adenoma or carcinoma[7-10], as compared to our case where the lowest intussuscepted segment was located in the lower rectum without protrusion through the anus.
In pathogenesis of intussusception, peristalsis and ingested food push the lesion with the adjacent bowel, which telescopes into the relaxed intestinal segment distal to it[3]. We initially planned to perform colonoscopy after bowel preparation using the polyethylene glycol electrolyte solution, not only to inspect the entire colon but to make a more specific diagnosis of the intussusception. But based on the findings that the patient suddenly complained of lower abdominal pain during bowel preparation and that the intussusceptum was detected 3 cm apart from anal verge at our clinic contrary to the sigmoidoscopic finding that the mass was reported to be 15 cm proximal to the anal verge at previous clinic, this bowel preparation might be, at least, an accelerating factor of intussusception by increased peristalsis. On the ground of clinical course in our case, whole gut irrigation as a bowel preparation should be used with caution because it may accelerate intussusception.
Early diagnosis and appropriate treatment are essential for intussusception because the mesentery of the involved segment is trapped between the overlapping layers of the bowel and its vascularity may be compromised. Unfortunately, a precise preoperative diagnosis is established in only less than half of the cases[3,5,11]. Two factors may be responsible for the low accuracy of the preoperative diagnosis in adult intussusception. One reason is the rare incidence of the intussusception itself and the other reason is the vague or nonspecific symptomatology. This condition is often misdiagnosed as a large polyp[9,12] or rectal prolapse[7,8] because of the wide variety of nonspecific symptoms that include abdominal pain, nausea and/or vomiting. It is noteworthy that, in most reports, the experience of the adult intussusception at each institution is limited to one or two cases per year[3-6,11]. Accordingly, the surgeon must keep in mind the possibility of intussusception even though the clinical signs of the patient may be very subtle.
Radiologic investigations may be helpful to distinguish intussusception from other common causes of intestinal obstruction, and for precisely identifying the etiologies of the intussusception preoperatively[13]. The characteristic finding of intussusception on a contrast study is a cup-shaped filling defect that is often accompanied with an additional filling defect representing the leading tumor[3]. Hydrostatic reduction under radiologic control, as employed in children, is less effective in adults and risk of perforation during the procedure is not negligible[10]. Generally, CT scan is acknowledged to be the most useful radiologic method that may provide additional preoperative information including the possible extension and/or dissemination of a malignant tumor[2,5,11,14]. The most common CT finding is a thickened segment of bowel with an eccentrically placed crescent-like fatty area; this represents the intussusception and the intussuscepted mesentery. This appears either as a round target mass or as a long sausage-shaped mass[14].
The appropriate management of adult intussusception is not always clear cut. Most authors agree that operative management of adult intussusception is almost always indicated because of high likelihood of neoplasm as a leading point, particularly if this occurs in the colon. There is controversy about the reduction before resection in cases of sigmoidorectal intussusception, even though most surgeons agree that primary surgical resection without a prior attempt at reduction is the treatment of choice in colocolic adult intussusception[3,5,13]. Several aspects to consider for reduction prior to resection are the reduction of externally viable bowel despite mucosal necrosis, intraluminal or transperitoneal seeding, venous embolization of malignant cells, and spillage of succus through inadvertent perforation[5]. For patients with sigmoidorectal intussusception, however, the decision regarding the operative procedure may be changed according to tumor involvement of the lower rectum. If the lower rectum is involved, an abdominoperineal resection is indicated. However, without evidence of distal disease, an initial reduction may permit a sphincter-saving procedure instead of the abdominoperineal resection as advocated by Matsuda et al [15]. In this sense, we would like to emphasize the significance of an attempt at manual reduction of the sigmoidorectal intussusception prior to resection, especially for those cases caused by benign lesion whereby an unnecessary abdominoperineal resection can be avoided. Because most colonic intussusceptions do not lead to complete obstruction, adequate preoperative bowel preparation is generally possible and this allows for a primary anastomosis[4].
There are good reasons for laparoscopic anterior resection in this case. The first reason is that the wide resection of intussuscepted colon and its mesentery dictates the most important technical consideration, because two-thirds of colocolic intussusceptions are associated with a malignant lesion[4]. Although preoperative findings were compatible to benign lesion, definite histopathologic diagnosis could not be made in an emergency situation. Moreover, the size of the sessile polyp was large enough (2 cm×2.5 cm on pathologic measurement) for surgeons to consider the possibility of a malignant polyp. In these emergency circumstances, choice of surgical procedure should be judged assuming a possibility of malignancy. The second is the danger in the reduction of externally viable bowel with mucosal necrosis. The third is that intra-abdominal exploration is possible to exclude dissemination in benign-appearing but malignancy-undeniable polyp in an emergency situation. Validities of laparoscopic oncologic colon surgery has been already established in the randomized multicenter trial[16].
In summary, the sigmoidorectal intussusception caused by sigmoid villotubular adenoma can be reduced by the push-up reduction technique, and safely treated by laparoscopic anterior resection. Our own technique using the sponge-on-the-stick is very useful in the situation that an abdominoperineal resection is, at first, deemed to be inevitable because the intussuscepted segment is very close to the anus. Therefore, this prior reduction technique followed by a resection can be considered for the sigmoidorectal intussusception to avoid inadvertent abdominoperineal resection. In conclusion, our principle of prior reduction technique followed by a laparoscopic resection may be of use in the management of benign sigomoidorectal intussusception involving lower rectum to avoid permanent stoma. Besides, it may also be applicable to instances of proven malignant intussusception involving the rectum provided that the lesion is confirmed to be localized without intra-abdominal dissemination or metastasis on the laparoscopic exploration before reduction and bowel resection.
S- Editor Kumar M L- Editor Elsevier HK E- Editor Li HY
| 1. | Huang BY, Warshauer DM. Adult intussusception: diagnosis and clinical relevance. Radiol Clin North Am. 2003;41:1137-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, Kuwano H. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol. 2003;36:18-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 133] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 384] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 4. | Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 233] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 666] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 6. | Carter CR, Morton AL. Adult intussusception in Glasgow, UK. Br J Surg. 1989;76:727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Lynn M, Agrez M. Management of sigmoid colon intussusception presenting through the anus. Aust N Z J Surg. 1998;68:683-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Nelson TM, Pearl RK, Prasad ML, Abcarian H. Perineal sigmoidectomy for sigmoid procidentia: report of a case. Am Surg. 1995;61:320-321. [PubMed] |
| 9. | Brozzetti S, Papa O, Polistena A, Mosiello G, Annessi P, Alessi G, Cavallaro A. Recurrent intussusception of the sigmoid colon caused by a transanal protruding sessile tubulo-villous malignant polyp. Anticancer Res. 2000;20:4697-4700. [PubMed] |
| 10. | Nesbakken A, Haffner J. Colo-recto-anal intussusception. Case report. Acta Chir Scand. 1989;155:201-204. [PubMed] |
| 11. | Eisen LK, Cunningham JD, Aufses AH. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 243] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 12. | Fujino Y, Fujio Y, Shimada E, Okazaki A. Intussusception due to vanishing colon cancer with metastasis of the regional lymph nodes: report of a case. Surg Today. 2000;30:188-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Weilbaecher D, Bolin JA, Hearn D, Ogden W. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121:531-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 213] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Gayer G, Apter S, Hofmann C, Nass S, Amitai M, Zissin R, Hertz M. Intussusception in adults: CT diagnosis. Clin Radiol. 1998;53:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 116] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Matsuda K, Suda K, Tamura K, Deguchi T, Yamazaki E, Yago H, Inaba T, Takeshima T, Adachi M, Okinaga K. Surgical management of adult sigmoid colon intussusception caused by a malignant tumor: report of a case. Surg Today. 2003;33:768-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | The Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2518] [Article Influence: 119.9] [Reference Citation Analysis (0)] |