Published online Nov 28, 2005. doi: 10.3748/wjg.v11.i44.7024
Revised: July 12, 2005
Accepted: July 15, 2005
Published online: November 28, 2005
AIM: To estimate the incidence of catheter tract implantation metastasis among patients undergoing percutaneous transhepatic biliary drainage (PTBD) for extrahepatic cholangiocarcinoma, and to provide data regarding the management of this unusual complication of PTBD by reviewing cases reported in the literature.
METHODS: A retrospective analysis of 67 consecutive patients who underwent PTBD before the resection of extrahepatic cholangiocarcinoma was conducted. The median follow-up period after PTBD was 106 mo. The English language literature (PubMed, National Library of Medicine, Bethesda, MD, USA), from January 1966 through December 2004, was reviewed.
RESULTS: Catheter tract implantation metastasis developed in three patients. The cumulative incidence of implantation metastasis reached a plateau (6%) at 20 mo after PTBD. All of the three patients with implantation metastasis died of tumor progression at 3, 9, and 20 mo after the detection of this complication. Among the 10 reported patients with catheter tract implantation metastasis from extrahepatic cholangiocarcinoma (including our three patients), two survived for more than 5 years after the excision of isolated catheter tract metastases.
CONCLUSION: Catheter tract implantation metastasis is not a rare complication following PTBD for extrahepatic cholangiocarcinoma. Although the prognosis for patients with this complication is generally poor, the excision of the catheter tract may enable survival in selected patients with isolated metastases along the catheter tract.
- Citation: Sakata J, Shirai Y, Wakai T, Nomura T, Sakata E, Hatakeyama K. Catheter tract implantation metastases associated with percutaneous biliary drainage for extrahepatic cholangiocarcinoma. World J Gastroenterol 2005; 11(44): 7024-7027
- URL: https://www.wjgnet.com/1007-9327/full/v11/i44/7024.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i44.7024
Percutaneous transhepatic biliary drainage (PTBD) has been widely employed as a biliary decompression procedure for malignant biliary obstruction[1-5]. It may cause implantation metastasis along the catheter tract, which has generally been considered as an unusual and lethal complication[6,7]. Although sporadic cases of such implantation metastasis have been reported[6-10], the incidence of this complication following PTBD is yet to be determined. Also, there is a paucity of data regarding the management of this complication. Taken together, these facts prompted us to conduct the current study.
The aims of this study were to estimate the incidence of catheter tract implantation metastasis among patients undergoing PTBD for extrahepatic cholangiocarcinoma, and to provide data regarding the management of this unusual complication by reviewing cases reported in the literature.
A total of 87 patients with carcinoma arising from the extrahepatic bile ducts (extrahepatic cholangiocarcinoma) underwent resection with curative intent at our department during the 15-year period between January 1988 and December 2002. Carcinoma arising from the cystic duct was categorized as extrahepatic cholangiocarcinoma according to the tumor-node-metastasis staging system[14]. Three patients who also had gallbladder carcinoma were excluded. Of the remaining 84 patients, 67 jaundiced patients underwent PTBD before the resection. They formed the basis of this retrospective study, and included 39 men and 28 women with a median age of 65 years (range: 35-88 years). All patients were Japanese.
The resectional procedures were chosen according to the primary tumor location. Forty-one patients with hilar cholangiocarcinoma underwent a hepatectomy with bile duct resection, 12 with non-hilar tumor underwent a Whipple procedure or a pylorus-preserving pancreaticoduodenectomy, six underwent a bile duct resection, and eight underwent a combination of hepatectomy and pancreaticoduodenectomy. Regional lymphadenectomy was performed in all patients.
The resected specimens were submitted to the Department of Surgical Pathology at our hospital for histologic evaluation. The histologic findings were described according to the tumor-node-metastasis staging system[14]. The histologic grade was determined based on the areas of the tumor with the highest grade[14]. Adenocarcinoma was identified as the primary tumor in 64 patients and adenosquamous carcinoma was identified in three patients.
Patients were followed up regularly at outpatient clinics every 3 mo. The median follow-up period after PTBD was 106 mo (range: 4 to 186 mo). By the time of disease status assessment, 38 patients had died of tumor recurrence. Seven patients had died of other causes with no evidence of tumor recurrence. One patient was alive with recurrent disease, and the remaining 21 patients were alive without disease.
The English language literature (PubMed, National Library of Medicine, Bethesda, MD, USA), from January 1966 through December 2004, was reviewed, and revealed that a total of seven patients undergoing resection of extrahepatic cholangiocarcinoma suffered from catheter tract implantation metastasis following PTBD[7-13].
Medical records and survival data were obtained for all the 67 patients. The causes of death were determined based on the medical records. The follow-up period was defined as the interval between the date of PTBD and that of the last follow-up. The Kaplan-Meier method was used to estimate both the cumulative incidence of catheter tract implantation metastasis and the cumulative patient survival rates. The differences in survival were evaluated using the log rank test. All statistical evaluations were performed using the SPSS 11.5J software package (SPSS Japan Inc., Tokyo, Japan). All tests were two-sided, and the differences with P values of <0.05 were considered statistically significant.
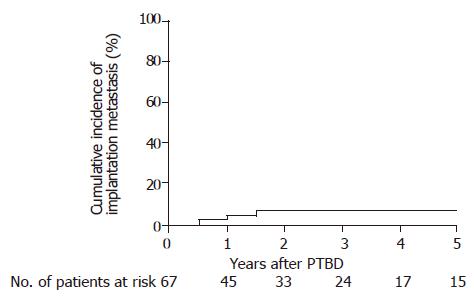
Catheter tract implantation metastasis after PTBD presented as a subcutaneous nodule in 3 of the 67 patients during the follow-up period. The interval between PTBD and the detection of implantation metastases was 7, 14, and 20 mo for those 3 patients. The cumulative incidence of this complication reached a plateau (6%) at 20 mo after PTBD (Figure 1).
Of the three patients with implantation metastases, one underwent a resection of the catheter tract (patient 9 in Table 1), one underwent local radiation (patient 8), and the other received the best supportive care (patient 10). They died of disease at 3, 9, and 20 mo after the detection of this complication.
| First | Sex/age | Histology of the primary tumor | Detection of metastases metastases after PTBD (mo) | Sites of recurrences other than the PTBD tract | Management of implantation metastases | Outcome after the detection of implantation metastases (mo) | ||
| n | author | (yr) | Type | Grade | ||||
| 1 | Sano[7] | M/68 | Adeno | G1 | 45 | – | Hx | 100; NED |
| 2 | Inagaki[8] | F/51 | As | nd | 6 | – | Hx, EAW | 65; NED |
| 3 | Matsumoto[9] | F/61 | Adeno | G2 | 21 | – | Hx | 24; NED |
| 4 | Shimizu[10] | M/75 | Adeno | G2 | 16 | – | Hx | 14; NED |
| 5 | Tersigni[11] | M/66 | Adeno | G1 | 13 | – | RTx, CTx | 4; DOD |
| 6 | Omokawa[12] | M/45 | Adeno | nd | 3 | - | Hx | nd; nd |
| 7 | Uenishi[13] | F/57 | Adeno | G1 | 14 | Pleura (right) | Pleuropneum- onectomy, ECW2 | 21; DOD |
| 8 | Sakata1 | F/63 | Adeno | G1 | 14 | Bone, Local | RTx | 20; DOD |
| 9 | Sakata1 | M/70 | Adeno | G2 | 20 | Peritoneum | EAW | 9; DO |
| 10 | Sakata1 | M/76 | Adeno | G3 | 7 | Local | BSC | 3; DOD |
An analysis of the 10 reported patients (including our three patients; Table 1) with catheter tract implantation metastasis revealed that the histologic grade of the primary tumor was well differentiated in four patients, moderately differentiated in three, poorly differentiated in one, and not documented in two. The median interval between PTBD and the detection of this complication was 14 mo (range: 3 to 45 mo).
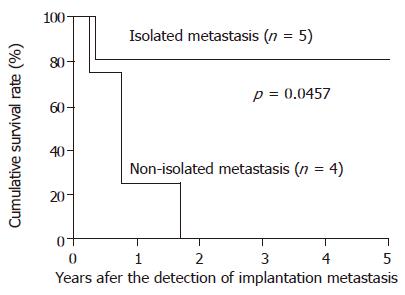
Catheter tract implantation metastasis was isolated (without recurrences at other sites) in six patients, whereas it was non-isolated (with recurrences at other sites) in the other 4 patients (Table 1). Although the survival after the detection of implantation metastasis was generally poor, two patients who underwent excision of isolated implantation metastases survived for more than five years. Among the nine patients with documented outcomes, those with isolated implantation metastases survived longer than those with non-isolated implantation metastases (P = 0.0457; Figure 2).
The incidence of catheter tract implantation metastasis after PTBD has been reported to range from 0.6 to 6% in patients with malignant biliary obstruction due to tumors of various origins[7,11,15-17]. Nimura et al[18] have reported a 3% incidence of such implantation metastasis among 133 patients with hilar cholangiocarcinoma. In the current series, the cumulative incidence of this complication increased with time and reached a plateau (6%) 20 mo after PTBD (Figure 2). The above data suggests that catheter tract implantation is not a rare complication following PTBD for extrahepatic cholangiocarcinoma.
Uesaka et al[19] have reported that catheter tract implantation metastasis from hilar cholangiocarcinoma occurred more frequently in patients with well differentiated tumors. Among the 10 reported patients with this complication (Table 1), only one had a poorly differentiated tumor, implying that differentiated tumors may be more related to the development of this complication than poorly differentiated ones. The association between implantation metastasis after PTBD and the histologic grade of extrahepatic cholangiocarcinoma warrants further investigation.
Although Sano et al[7] have reported the occurrence of a late implantation metastasis arising 46 mo after PTBD for extrahepatic cholangiocarcinoma, most of our collected patients suffered from this complication within 21 mo after PTBD (Table 1). Thus, patients undergoing PTBD for extrahepatic cholangiocarcinoma should be monitored for catheter tract implantation for around 2 years.
The survival of patients with catheter tract implantation metastasis from extrahepatic cholangiocarcinoma was found to be generally poor (Table 1), as with our patients. Despite the metastatic nature of this condition, surprisingly, the outcome after the excision of the implantation metastasis was not so dismal in some patients with isolated implantation metastases (patients 1-4). The possibility that the course of deceased patients is unlikely to be reported (a publication bias) may, in part, explain this. In order to excise catheter tract metastases following PTBD, a hepatectomy is usually required, because the catheter tract runs through the liver parenchyma; in some patients, a local excision of the abdominal wall is also required. Two of the five patients who underwent a hepatectomy, with or without a local excision of the abdominal wall, for isolated implantation metastases (patients 1 and 2) survived for more than 5 years with no evidence of the disease. This clearly demonstrates that excision of the metastases offers the only chance for long-term survival.
The issue how to prevent catheter tract implantation metastasis following PTBD is yet to be resolved. Although excision of the catheter tract along with the resection of the primary tumor appears to be effective, it is practically difficult to excise the whole catheter tract between the surface of the skin and the punctured intrahepatic bile ducts. Some authors have advocated ethanol injection into the catheter tract to prevent cancer implantation[10,19,20]. However, Shimizu and colleagues have reported a case of implantation metastasis following ethanol injection[10]. Further investigation is warranted to conclude the effects of this procedure.
In conclusion, catheter tract implantation metastasis is not a rare complication following PTBD for extrahepatic cholangiocarcinoma. Although the prognosis for patients with this complication is generally poor, excision of the catheter tract, which usually requires a hepatectomy, enables long-term survival in selected patients with isolated implantation metastases.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Takada T, Hanyu F, Kobayashi S, Uchida Y. Percutaneous transhepatic cholangial drainage: direct approach under fluoroscopic control. J Surg Oncol. 1976;8:83-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 71] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Hatfield AR, Tobias R, Terblanche J, Girdwood AH, Fataar S, Harries-Jones R, Kernoff L, Marks IN. Preoperative external biliary drainage in obstructive jaundice. A prospective controlled clinical trial. Lancet. 1982;2:896-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 263] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 3. | Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 1990;14:535-543; discussion 544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 320] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 4. | Nagino M, Hayakawa N, Nimura Y, Dohke M, Kitagawa S. Percutaneous transhepatic biliary drainage in patients with malignant biliary obstruction of the hepatic confluence. Hepatogastroenterology. 1992;39:296-300. [PubMed] |
| 5. | Wakai T, Shirai Y, Moroda T, Yokoyama N, Hatakeyama K. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer. 2005;103:1210-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 181] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 6. | Chapman WC, Sharp KW, Weaver F, Sawyers JL. Tumor seeding from percutaneous biliary catheters. Ann Surg. 1989;209:708-713; discussion 713-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 75] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Sano T, Nimura Y, Hayakawa N, Kamiya J, Kondo S, Nagino M, Kanai M, Miyachi M, Uesaka K. Partial hepatectomy for metastatic seeding complicating pancreatoduodenectomy. Hepatogastroenterology. 1997;44:263-267. [PubMed] |
| 8. | Inagaki M, Yabuki H, Hashimoto M, Maguchi M, Kino S, Sawa M, Ojima H, Tokusashi Y, Miyokawa N, Kusano M. Metastatic seeding of bile duct carcinoma in the transhepatic catheter tract: report of a case. Surg Today. 1999;29:1260-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Matsumoto A, Imamura M, Akagi Y, Kaibara A, Ohkita A, Mizobe T, Isomoto H, Aoyagi S. A case report of disseminated recurrence of inferior bile duct carcinoma in PTCD fistula. Kurume Med J. 2002;49:71-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Shimizu Y, Yasui K, Kato T, Yamamura Y, Hirai T, Kodera Y, Kanemitsu Y, Ito S, Shibata N, Yamao K. Implantation metastasis along the percutaneous transhepatic biliary drainage sinus tract. Hepatogastroenterology. 2004;51:365-367. [PubMed] |
| 11. | Tersigni R, Rossi P, Bochicchio O, Cavallini M, Ambrogi C, Bufalini G, Alessandroni L, Arena L, Armeni O, Miraglia F. Tumor extension along percutaneous transhepatic biliary drainage tracts. Eur J Radiol. 1986;6:280-282. [PubMed] |
| 12. | Omokawa S, Hashizume T, Ohsato M, Nanjo H, Asanuma Y, Koyama K. Insemination of bile duct carcinoma to the liver after insertion of percutaneous biliary endoprosthesis. Gastroenterol Jpn. 1991;26:678-682. [PubMed] |
| 13. | Uenishi T, Hirohashi K, Inoue K, Tanaka H, Kubo S, Shuto T, Yamamoto T, Kaneko M, Kinoshita H. Pleural dissemination as a complication of preoperative percutaneous transhepatic biliary drainage for hilar cholangiocarcinoma: report of a case. Surg Today. 2001;31:174-176. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, Morrow M. American Joint Committee on Cancer (AJCC) Staging Manual. 6th ed. New York: Springer-Verlag 2002; 145-150. [DOI] [Full Text] |
| 15. | Oleaga JA, Ring EJ, Freiman DB, McLean GK, Rosen RJ. Extension of neoplasm along the tract of a transhepatic tube. AJR Am J Roentgenol. 1980;135:841-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Shorvon PJ, Leung JW, Corcoran M, Mason RR, Cotton PB. Cutaneous seeding of malignant tumours after insertion of percutaneous prosthesis for obstructive jaundice. Br J Surg. 1984;71:694-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Kim WS, Barth KH, Zinner M. Seeding of pancreatic carcinoma along the transhepatic catheter tract. Radiology. 1982;143:427-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Nimura Y, Kamiya J, Kondo S, Nagino M, Uesaka K, Oda K, Sano T, Yamamoto H, Hayakawa N. Aggressive preoperative management and extended surgery for hilar cholangiocarcinoma: Nagoya experience. J Hepatobiliary Pancreat Surg. 2000;7:155-162. [RCA] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 268] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 19. | Uesaka K, Kamiya J, Nagino M, Yuasa N, Sano T, Oda K, Kanai M, Hayakawa N, Yamamoto H, Yokoi S. [Treatment of recurrent cancer after surgery for biliary malignancies]. Nihon Geka Gakkai Zasshi. 1999;100:195-199. [PubMed] |
| 20. | Kondo S, Nimura Y, Hayakawa N, Kamiya J, Shionoya S. Ethanol injection for prevention of seeding metastasis along the tract after percutaneous transhepatic biliary drainage. J Jpn Bil Assoc. 1989;3:100-105 (in Japanese with English abstract). |