Published online Sep 28, 2005. doi: 10.3748/wjg.v11.i36.5739
Revised: November 15, 2004
Accepted: November 19, 2004
Published online: September 28, 2005
Placement of self-expandable metal stents (SEMS) is an effective mode of palliative treatment for patients with malignant gastrointestinal obstruction. Gastrointestinal mucosal bleeding complicates about 5% of placement of SEMS but is not well described. We report three cases of gastrointestinal bleeding post-SEMS placement and suggest that bleeding is caused by direct mucosal infringement by the sharp edges of the ends of the stents.
- Citation: Wai CT, Khor C, Lim SE, Ho KY. Post-metallic stent placement bleeding caused by stent-induced ulcers. World J Gastroenterol 2005; 11(36): 5739-5741
- URL: https://www.wjgnet.com/1007-9327/full/v11/i36/5739.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i36.5739
Placement of self-expandable metal stents (SEMS) has emerged as an effective mode of palliative treatment for patients with malignant gastrointestinal obstruction[1,2]. This is particularly true in patients with locally advanced disease or patients with multiple co-morbidities, where open or laparoscopic surgical by -pass is associated with high post-operative mortality and morbidity[3,4] . Although placement of SEMS is successful in almost 100% of cases, complications of SEMS do occur and include re-obstruction (10%), stent migration (10%), pain (5%), perforation (4%), and rarely, death (1%)[5,6]. Bleeding has been reported to occur in 5% of patients following placement of SEMS. The mechanisms to explain such bleeding have not been well described. In this report, we describe three cases of bleeding post -SEMS placement and suggest that stent-induced ulcers were caused by infringement of the raw ends of the stents onto the mucosa that may be the cause of such bleeding.
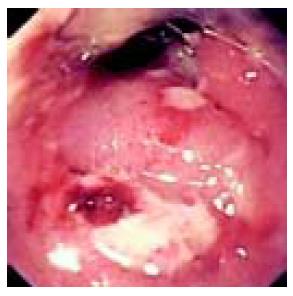
The first patient was a 93-year-old female with a past history of diabetes mellitus, hypertension, cerebrovascular accident, who presented with subacute intestinal obstruction. Sigmoidoscopy showed a large tumor at the recto-sigmoid junction, causing almost complete obstruction of the intestinal lumen. The CF240 endoscope (Olympus Pte Ltd, Singapore) could not be passed to cross the structure (Figure 1). In view of her poor pre-morbid status, the family and the attending gastroenterologist opted for palliative stenting. Stenting was done with 85 mm × 25 mm Ultraflex® stent (Boston Scientific Pte Ltd, Singapore), which was successful and uneventful. The patient was able to pass motion after the stenting and was discharged one day after the procedure. Unfortunately, she was readmitted 8 wk later for fresh per rectal bleeding. A repeat sigmoidoscopy showed a patent stent with a circumferential mucosal ulcer being impinged upon by the proximal sharp edges of the stent (Figure 2). The bleeding stopped spontaneously and no specific treatment was required. The patient was well till 4 wk post-discharge.
The second patient was a 51-year-old man who presented with gastric outlet obstruction one year after cholecystectomy with hepaticojejunostomy for gallbladder carcinoma. CT scan of the abdomen showed local recurrence at the head of pancreas with liver metastasis. Gastroscopy showed pyloric stenosis due to extrinsic compression, which was not passable by the XQ240 endoscope (Olympus Pte Ltd, Singapore). In view of the metastatic disease and previous laparotomy, the family and the attending gastroenterologist decided on placement of SEMS for palliation of the gastric outlet obstruction. A 60 mm × 22 mm uncovered Enteral Wallstent® (Boston Scientific Pte Ltd, Singapore) was subsequently placed successfully. The patient was able to tolerate oral diet and remained well until 4 wk later, when he was noted to have a drop in hemoglobin to 3.9 g/dL from a baseline level of 9 g/dL. A repeat gastroscopy showed a patent stent with circumferential ulcers on the mucosa of the first part of duodenum being impinged upon by the distal end of the stent (Figure 3). Hemostasis was secured by application of argon plasma coagulation (Erbe, JDH Medical System, Singapore). He recovered well with stable hemoglobin and absence of rebleeding up to 4 wk post discharge.
The third patient was an 80-year-old man with adenocar- cinoma at the gastroesophageal junction, presenting with dysphagia. Despite seven previous dilatations using savary dilators, his dysphagia persisted. A 16 cm × 24 mm Flamingo stent (Boston Scientific Pte Ltd, Singapore) was subsequently inserted uneventfully with relief of his dysphagia. He was readmitted 16 wk later for melena and anemia, requiring blood transfusion. A repeat gastroscopy showed oozing from the esophageal mucosa at the proximal end of the stent (Figure 4). No endoscopic therapy was applied as no focal site of active bleeding was noted at that time. The patient was given oral sulcralfate and tranexamic acid. He succumbed to his metastatic disease 8 wk later although his rebleeding did not occur.
Gastrointestinal cancers are among the commonest cancers in most developed countries. Unfortunately, less than half of the patients are candidates for curative surgery, and maintaining patency of the gastrointestinal tract becomes one of the most important aspects of palliative management[7,8]. Among the different modes of palliation, SEMS placement offers the advantage of a high success rate and a low procedure-related complication rate[9]. However, 10-20% of complications, including stent migration, reobstruction by tumor ingrowth, and perforation, have been reported[10]. Bleeding post-stent placement is considered rare at <5%, and has not been studied well.
In this study, we encountered three cases of delayed bleeding post-stent placement, which occurred 4-16 wk after placement. The bleeding originated from ulcers that arose as a result of impingement by the sharp flaring edges of the stents. No active bleeding was noted from the tumor itself. Bleeding stopped spontaneously in one case, and was arrested by argon plasma coagulation application in one and sulcrafate plus tranexamic acid in another. The bleeding appeared to be self-limiting, as no rebleeding was seen after 4-8 wk of follow-up.
Mucosal response to stents is not well understood. Previous animal studies suggest that stents could cause inflammation and collagenous reaction at the underlying mucosa[11]. Another human autopsy study suggests that stents could cause pressure necrosis in the underlying tumor, followed by chronic inflammatory response in the tumor, and epithelialization of the stent lumen[12]. However, these studies did not evaluate the cause of bleeding post-tent insertion.
We believe that direct impingement of gastrointestinal mucosa by the sharp edges of the metallic stent may be an important cause of ulcer formation and bleeding post-stent placement. Manufacturers of SEMS should be aware of this potential technical complication and consider making stents with blunt and softer edges, which may help in avoiding such a complication.
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
| 1. | Kim JH, Yoo BM, Lee KJ, Hahm KB, Cho SW, Park JJ, Kim SS, Park HC, Kim JH. Self-expanding coil stent with a long delivery system for palliation of unresectable malignant gastric outlet obstruction: a prospective study. Endoscopy. 2001;33:838-842. [PubMed] [DOI] [Full Text] |
| 2. | Baron TH, Rey JF, Spinelli P. Expandable metal stent placement for malignant colorectal obstruction. Endoscopy. 2002;34:823-830. [PubMed] [DOI] [Full Text] |
| 3. | Buechter KJ, Boustany C, Caillouette R, Cohn I. Surgical management of the acutely obstructed colon. A review of 127 cases. Am J Surg. 1988;156:163-168. [PubMed] [DOI] [Full Text] |
| 4. | van Wagensveld BA, Coene PP, van Gulik TM, Rauws EA, Obertop H, Gouma DJ. Outcome of palliative biliary and gastric bypass surgery for pancreatic head carcinoma in 126 patients. Br J Surg. 1997;84:1402-1406. [PubMed] [DOI] [Full Text] |
| 5. | Khot UP, Lang AW, Murali K, Parker MC. Systematic review of the efficacy and safety of colorectal stents. Br J Surg. 2002;89:1096-1102. [PubMed] [DOI] [Full Text] |
| 6. | Gukovsky-Reicher S, Lin RM, Sial S, Garrett B, Wu D, Lee T, Lee H, Arnell T, Stamos MJ, Eysselein VE. Self-expandable metal stents in palliation of malignant gastrointestinal obstruction: review of the current literature data and 5-year experience at Harbor-UCLA Medical Center. MedGenMed. 2003;5:16. [PubMed] |
| 7. | Bond JH. Colorectal cancer update. Prevention, screening, treatment, and surveillance for high-risk groups. Med Clin North Am. 2000;84:1163-182, viii. [PubMed] [DOI] [Full Text] |
| 8. | Morgan R, Adam A. Use of metallic stents and balloons in the esophagus and gastrointestinal tract. J Vasc Interv Radiol. 2001;12:283-297. [PubMed] [DOI] [Full Text] |
| 9. | Yim HB, Jacobson BC, Saltzman JR, Johannes RS, Bounds BC, Lee JH, Shields SJ, Ruymann FW, Van Dam J, Carr-Locke DL. Clinical outcome of the use of enteral stents for palliation of patients with malignant upper GI obstruction. Gastrointest Endosc. 2001;53:329-332. [PubMed] [DOI] [Full Text] |
| 10. | Baron TH, Harewood GC. Enteral self-expandable stents. Gastrointest Endosc. 2003;58:421-433. [PubMed] [DOI] [Full Text] |
| 11. | Cwikiel W, Willén R, Stridbeck H, Lillo-Gil R, von Holstein CS. Self-expanding stent in the treatment of benign esophageal strictures: experimental study in pigs and presentation of clinical cases. Radiology. 1993;187:667-671. [PubMed] [DOI] [Full Text] |
| 12. | Bethge N, Sommer A, Gross U, von Kleist D, Vakil N. Hu-man tissue responses to metal stents implanted in vivo for the palliation of malignant stenoses. Gastrointest Endosc. 1996;43:596-602. [DOI] [Full Text] |