INTRODUCTION
Endoscopic mucosal resection (EMR) is a well-established and non-invasive therapeutic procedure for colorectal neoplasm in the early stage. Although rare, various complications including hemorrhage and perforation have been reported. On the other hand, pneumoscrotum is uncommon and it is generally a term used for the expression of the presence of gas within the scrotum[1]. Although most cases are associated with pneumoperitoneum, there have only been two reported cases after colonoscopy. We report herein, a delayed colonic perforation revealed by a rare manifestation of pneumoscrotum after EMR of a laterally spreading tumor in the descending colon.
CASE REPORT
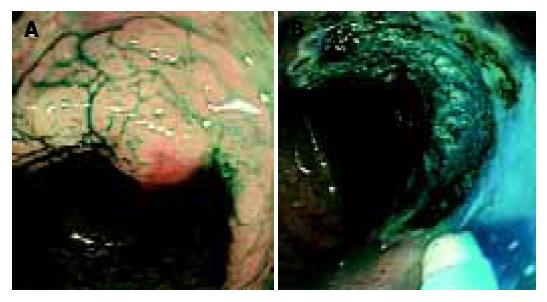
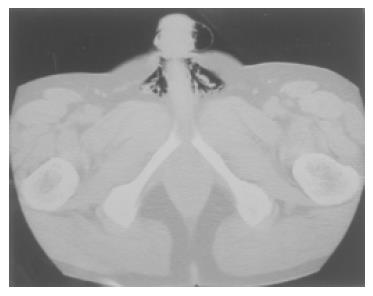
A 52-year-old man underwent total colonoscopy because of a positive fecal occult blood test in our hospital. The colonoscopy showed a laterally spreading tumor with uneven nodules in the descending colon, of which the superficial margin was clear after chromoendoscopy using indigo-carmine dye spraying. (Figure 1A) Magnifying colonoscopy after indigo-carmine dye and crystal violet staining disclosed type IIIL and type IV pit patterns, therefore, this lesion was endoscopically diagnosed as an intra-mucosal carcinoma in an adenoma[2]. Endoscopic mucosal resection (EMR) was attempted with a curative intent. Subsequently, for better elevation and identification of the submucosal layer, 20 mL of 10% glycerin (GLYCEOL®) containing a small amount of 0.4% indigo-carmine was injected into the submucosal layer[3] The lesion was well-elevated, and was resected with five fragments. After the EMR, magnifying observation revealed a small amount of residual tumor at the periphery, and argon plasma coagulation (APC) was performed for ablation. (Figure 1B) The argon plasma coagulator was used with setting at 2.0 L/min gas flow and with power of 50 W. To reduce the risk of perforation, APC was only applied to coagulate the edge of the EMR site and the duration of application was as short as 5 s. The patient did not complain of abdominal pain or fullness during or immediately after the therapeutic procedure, and no complication such as bleeding or perforation was identified during colonoscopy. The patient’s education included no alcohol and no exercise for 1 wk after EMR. He was discharged 1 h after the procedure, uneventfully. However, he revisited our center the next day because of mild inguinal pain and an enlarged scrotum. Before admission, he had taken two meals including a dinner and a breakfast as usual. On admission, his vital signs were within normal limits excluding mild fever, and physical examination disclosed only an enlarged but light scrotum, and no abdominal tenderness or muscular defense was found. Upright abdominal X-ray film showed free air in the left sub-diaphragm. (Figure 2) Computed tomograhy (CT) of the chest and abdomen revealed pneumopericardium, pneumoperitoneum and bilateral pneumoscrotum. (Figure 3) The laboratory data showed that WBC count was 12 000 and C-reactive protein was 58 mg/dL, respectively. Other data were within normal limitation. A diagnosis of colonic perforation in delayed fashion was made. After consultation with the surgeons, the patient was first treated medically under NPO; administration of antibiotics (cefmetazole sodium, 4 g/d) and subsequent hyperalimentation were carried out for 2 d. The fever and inguinal pain were relieved within 24 h. The pneumoscrotum resolved within 2 d, the resolution of the pneumoscrotum was judged by CT and physical examination and the symptoms of the patient. C-reactive protein levels decreased from 5.8 to 0.6 mg/dL in 4 d. The permission of oral intake was based on the clinical course, physical examination, laboratory data, and the patient’s symptoms. Oral intake was started on the third day at hospital, and he was discharged uneventfully after five days of hospitalization. The removed specimen was histologically diagnosed as a tubular adenoma, with focal carcinoma limited to within the mucosal layer. No muscle layer was identified in the resected specimens.
Figure 1 A: Colonoscopy after indigo-carmine dye spraying showed a laterally spreading tumor 35 mm in diameter in the descending colon; B: The ulcer after piecemeal EMR and APC revealed no active bleeding or perforation.
Figure 2 Upright abdominal X-p film showed free air in the sub-diaphragmatic space.
Figure 3 Abdominal computed tomography disclosed free air in the scrotum.
DISCUSSION
Colonic perforation associated with therapeutic colonoscopy is uncommon, and the reported incidence ranges from 0.073% to 2.14%[4-6]. It could occur immediately or in a delayed fashion. Most of the signs of colonic perforation are abdominal symptoms including peritonitis. However, our case presented pneumoscrotum as a sign of a colonic perforation after EMR in delayed fashion. Pneumoscrotum is a term, which implies the presence of air within the scrotum[1]. Although pneumoscrotum associated with pneumomediastinum and subcutaneous emphysema, secondary to pneumothorax is a well-described entity, there have only been two reported cases following colonoscopy and both cases occurred immediately after the procedures[7-11]. Our patient developed pneumoscrotum in a delayed fashion, which is different from the previous reports. The reason, why we diagnosed the perforation developed in delayed fashion is as follows, first, our patient did not complain of any symptoms related to colonic perforation during EMR or in the recovery room before discharge. Second, repeated review of the recorded video tape of the procedure also revealed no definite perforation. Therefore, the perforation was suggested to have developed in a delayed fashion to firstly create pneumoperitoneum, and the air then reached the scrotum and created pneumoscrotum, which presented as the first symptom and sign of colonic perforation.
Colonic perforation may be intraperitoneal or retrope-ritoneal, or both[11]. Our case presented pneumoscrotum, pneumopericardium and pneumoperitoneum, which suggested that the perforation developed in the retroperitoneal space. That our case developed in a delayed fashion also supported that the perforation was retroperitoneal, as, compared to intraperitoneal perforation, retroperitoneal perforation is reported to be relatively painless and to become clear, some hours after the procedure. Furthermore, most cases presenting pneumoscrotum are associated with pneumoperitoneum, like ours[12-14].
Our case was treated successfully without laparotomy, however, the choice of conservative or surgical treatment for iatrogenic colonic perforation remains controversial[15-18]. The finding of air in the scrotal sac may be an early sign of a life-threatening condition, or may represent an incidental finding associated with more common benign conditions[1]. It depends on the local air production or movement of air from the peritoneal space. Local air production suggests gas gangrene or scrotal trauma, which is infectious and may be fatal, unless treated appropriately. On the other hand, movement of air from the peritoneal space is usually non-infectious and can be treated conservatively. The reported case of pneumoscrotum secondary to colonic perforation in the retroperitoneal space following colonoscopy were successfully treated non-operatively[10,11]. In this case, the choice of non-surgical treatment was based on the following: first, the patient’s vital signs were stable; second, the abdominal pain was mild and localized; and third, the pneumoscrotum was painless and the air was not locally produced but originated from the pneumoperitoneum. Additionally, and perhaps most important, no unexplained peritoneal fluid was found in the abdominal CT, which suggested no severe peritonitis. Therefore, in this case the pneumoscrotum and pneumoperitoneum was finally judged to be non-infectious.
In conclusion, we report a case of colonic perforation occurring in delayed fashion after EMR, which was revealed by pneumoscrotum. Although rare, colonoscopists should keep in mind that pneumoscrotum could present as a sign of colonic perforation, and the choice of treatment should be chosen carefully.