Published online Jul 28, 2005. doi: 10.3748/wjg.v11.i28.4443
Revised: July 13, 2004
Accepted: July 17, 2004
Published online: July 28, 2005
A 44-year-old man was referred to our hospital with intermittent abdominal pain. Because distention of fluid- and gas-filled loops of small intestine was proved by X-ray, the patient was diagnosed as having small bowel obstruction. A laparotomy revealed a segmental stenosis in the jejunum, which showed diffuse thickening of the intestinal wall. Some mesenteric lymph nodes were swollen. Pathological examination was defined. We diagnosed diffuse large B-cell lymphoma based on the pathological findings of diffuse transmural infiltration of large lymphoid cells and flow-cytometric analyses. Rituximab was administered as adjuvant therapy at weekly doses of 375 mg/m2. Four cycles were performed every 6 mo and he remained CR. Rituximab may be effective as adjuvant therapy.
- Citation: Nomura K, Tomikashi K, Matsumoto Y, Yoshida N, Okuda T, Sakakura C, Mitsufuji S, Horiike S, Yamagishi H, Okanoue T, Taniwaki M. Small bowel non-Hodgkin's lymphoma remaining in complete remission by surgical resection and adjuvant rituximab therapy. World J Gastroenterol 2005; 11(28): 4443-4444
- URL: https://www.wjgnet.com/1007-9327/full/v11/i28/4443.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i28.4443
Primary gastrointestinal lymphoma (PGL) accounts for 4-20% of all non-Hodgkin’s lymphomas (NHL)[1,2]. The location most frequently involved has been the ileocecal region, followed by small bowel, accounting for 20-40% of PGL[1]. Small bowel lymphoma tends to be annular in the distal ileum, not proximal[2]. Jejunum obstruction in a patient with NHL has been exceptionally described.
Regarding treatment, it has been established that the primary surgical treatment had the most favorable influence on failure-free survival in localized diseases and hence the resection may be appropriate as the primary treatment[3]. On the other hand, the effectiveness of adjuvant therapy for localized NHL remains to be unclear, because some cases could be cured only by surgical resection.
In this study, we have described the primary jejunal NHL with small bowel obstruction, which remained in complete remission by surgical resection followed by rituximab administration.
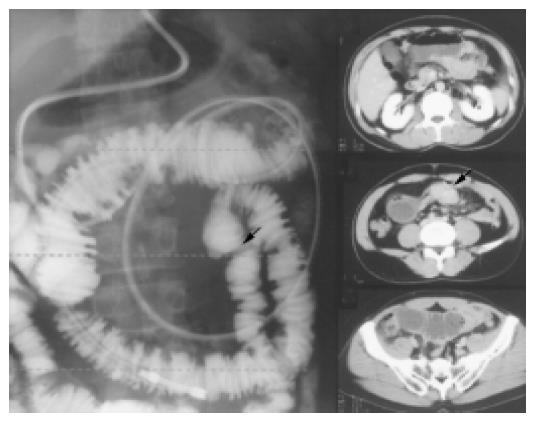
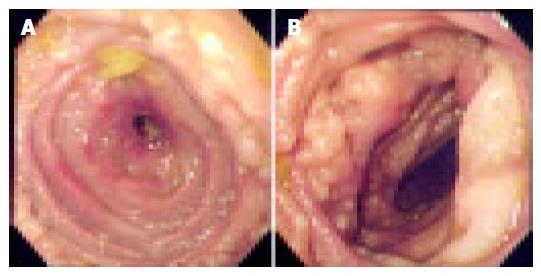
A 44-year-old man was admitted to our hospital in May 2002 because of intermittent abdominal pain. Small bowel series and computed tomography (CT) of the abdomen showed stenosis at jejunum and dilatation of small bowel (Figures 1 and 2), indicating small bowel obstruction. However, the cause of obstruction remained unclear in spite of several workups. Laparotomy disclosed a 3 cm long jejunal segment stenosis at 110 cm from the ligament of Treitz and some mesenteric lymph nodes were swollen. The resected specimens showed diffuse thickening of the intestinal wall, histopathological analysis of which showed that large lymphoid cells aggregated diffusely. Mesenteric lymph nodes were also involved. Flow-cytometric studies showed that the tumor cells expressed HLA-DR (84.8%), s-IgA (46.6%), g (69.8%), CD10 (44.7%), CD19 (68.1%), and CD20 (62.4%) with a high-intensity signal. Results for CD5 were negative (26.2%) with a low-intensity signal. Postoperative workup did not demonstrate the evidence of systemic involvement. Thus, the patient was diagnosed having primary jejunal diffuse large B-cell lymphoma at stage II1. Rituximab was administered as adjuvant therapy at weekly doses of 375 mg/m2. Four courses were performed every 6 mo and the patient is in complete remission with a follow-up time of 24 mo with no significant adverse effects.
We experienced a rare case of primary jejunal NHL as radiological workup including CT and angiography provided no evidence for final diagnosis, we performed laparotomy and segmental intestinal resection. The recognition of the possibility of jejunal obstruction due to NHL may facilitate early diagnosis. Yamamoto et al[4] have recently developed double-balloon endoscopy. This method enables us to survey all intestines with ease. In future, this method may become the routine mode of study for small bowel obstruction.
Regarding treatment, we performed segmental resection of jejunum and rituximab therapy as adjuvant treatment. The efficacy and toxicity of adjuvant therapy for localized NHL remained unclear because excess chemotherapy may provoke secondary malignancies. On the other hand, a new anti-CD20 mAb, rituximab, is effective in the treatment of B-cell lymphoma with slight adverse effects[5,6]. Thus we treated the patient under study with rituximab as adjuvant therapy. He tolerated this adjuvant therapy well, with slight nausea. Rituximab may be effective as adjuvant therapy for PGL. The efficacy and toxicity should be examined in large series.
Science Editor Zhu LH and Guo SY Language Editor Elsevier HK
| 1. | Lee J, Kim WS, Kim K, Ko YH, Kim JJ, Kim YH, Chun HK, Lee WY, Park JO, Jung CW. Intestinal lymphoma: exploration of the prognostic factors and the optimal treatment. Leuk Lymphoma. 2004;45:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Domizio P, Owen RA, Shepherd NA, Talbot IC, Norton AJ. Primary lymphoma of the small intestine. A clinicopathological study of 119 cases. Am J Surg Pathol. 1993;17:429-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 146] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Samel S, Wagner J, Hofheinz R, Sturm J, Post S. Malignant intestinal non-Hodgkin's lymphoma from the surgical point of view. Onkologie. 2002;25:268-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Yamamoto H, Sugano K. A new method of enteroscopy--the double-balloon method. Can J Gastroenterol. 2003;17:273-274. [PubMed] |
| 5. | Maloney DG, Grillo-López AJ, Bodkin DJ, White CA, Liles TM, Royston I, Varns C, Rosenberg J, Levy R. IDEC-C2B8: results of a phase I multiple-dose trial in patients with relapsed non-Hodgkin's lymphoma. J Clin Oncol. 1997;15:3266-3274. [PubMed] |