Published online May 7, 2005. doi: 10.3748/wjg.v11.i17.2630
Revised: March 10, 2004
Accepted: January 13, 2005
Published online: May 7, 2005
AIM: To provide the clinical and epidemiological data of inflammatory bowel disease (IBD) patients of North-Eastern Poland.
METHODS: A total of 248 IBD patients diagnosed and hospitalized in the Department of Infectious Diseases in Bialystok between 1990 and 2003 were included in the study. We analyzed age, sex, education, characteristics of job, type of the environment, discontinuation of employment due to IBD, colitis extent, need of surgical treatment, and coexistence of other diseases.
RESULTS: Two hundred and thirty-three IBD patients (94%) were diagnosed as ulcerative colitis (UC), and only 15 (6%) were diagnosed as Crohn’s disease (CD). Patients with CD were significantly younger at the time of diagnosis and male predominance was observed. The mean age of the patients at the time UC diagnosis was 44.9±1.1 years. Histogram of the age of patients showed the characteristic biphasic distribution with two peaks between 20 and 40 years and between 60 and 70 years. The predominant form of UC was left sided colitis, which affected almost 80% of the studied population. The most extensive form - pancolitis was present in 34 patients (15%). Only 6% of UC patients required surgery, whereas 36% of CD patients underwent surgery (P<0.005). Among coexisting disorders, cholelithiasis was the most prevalent and demonstrated in 35 patients (14%), pulmonary disorders were diagnosed in 2%, and psoriasis in 1.4%. Since 1998, the number of admitted IBD patients has slightly increased.
CONCLUSION: Occurrence of UC in Poland is much higher than that of CD. The majority of UC cases are diagnosed in young people (20-40 years) with the predominance of male patients. The most common clinical form of UC is left sided colitis.
- Citation: Wiercinska-Drapalo A, Jaroszewicz J, Flisiak R, Prokopowicz D. Epidemiological characteristics of inflammatory bowel disease in North-Eastern Poland. World J Gastroenterol 2005; 11(17): 2630-2633
- URL: https://www.wjgnet.com/1007-9327/full/v11/i17/2630.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i17.2630
Inflammatory bowel diseases (IBD) including ulcerative colitis (UC) and Crohn’s disease (CD) occur with different frequencies around the world. The countries reporting the highest estimates of UC are USA, UK and Sweden[1-3]. The countries reporting the lowest estimates of UC are the countries of southern Europe, South Africa and Australia[4]. The epidemiological data of the UC prevalence in Europe are provided by the Western Europe countries[5]. Only few and scattered reports come from the countries of the Eastern and Middle Europe. No information is available regarding the incidence and characteristics of IBD in Poland. Therefore, the main objective of our study was to provide the clinical and epidemiological data of IBD patients of North-Eastern Poland treated in our hospital between 1990 and 2003.
All patients diagnosed with IBD and hospitalized in the Department of Infectious Diseases in Bialystok between 1990 and 2003 were included in the study. As a rule all patients from Bialystok area with onset of diarrhea were referred to our Department. IBD diagnosis was based on typical clinical course of the disease and endoscopic examination with histologic confirmation of UC or CD. Patients with unidentified colitis and infectious enterocolitis were excluded.
Data were retrieved from electronic database of all patients hospitalized in Department of Infectious Diseases in Bialystok. We analyzed age, sex, education, characteristics of job, type of the environment, discontinuation of employment due to IBD, colitis extent, need of surgical treatment, and coexistence of other diseases.
The extent of colitis was defined as follows: proctitis: involvement of rectum; left sided colitis: involvement of colon up to splenic flexure; pancolitis: entire colon affected.
Measured values were expressed as mean±SE. Significance of differences between studied groups was calculated by non-parametric Mann-Whitney U test and χ2 test. P <0.05 was considered statistically significant. Statistical analyses were performed with Statistica 5.0 for Windows (Statsoft Inc., Tulsa, USA).
A total of 248 IBD patients were included in the study (mean age 44.3±1.1 years). Epidemiologic characteristics of the studied population are presented in Table 1. Two hundred and thirty three IBD patients (94%) were diagnosed as ulcerative colitis, and only 15 (6%) were diagnosed as CD. Therefore the UC/CD ratio was over 15:1. Patients with CD were significantly younger at the time of diagnosis (44.9±1.1 vs 34.3±2.9 years, P = 0.01) and male predominance was observed (male/female ratio was 1.2 for UC, and 4.0 for CD). There were no significant differences between UC and CD when education, type of job or environmental background were taken into consideration (Table 1). Family history of the disease was noticed only in 2 cases (4 patients).
| UC (n = 233) | CD (n = 15) | P | |
| Age of diagnosis (yr) | 44.9± 1.1 | 34.3± 2.9 | 0.01 |
| Sex (male/female) | 128/105 | 12/3 | 0.06 |
| Environment (urban/rural) | 163/69 | 13/2 | 0.39 |
| Education (grammar/secondary/high) | 106/83/30 | 7/ 5/3 | 0.93 |
| Labor (manual/intellectual) | 138/72 | 10/5 | 0.94 |
The mean age of the patients at the time of UC diagnosis was 44.9±1.1 years (range 18-83 years). There were no significant differences between men and women (45.9±1.4 vs 43.7±1.7 years, P = 0.31). Histogram of the age of patients showed the characteristic biphasic distribution with two peaks between 20 and 40 years and between 60 and 70 years (Figure 1). Age of disease onset was associated with the extent of colitis, the highest proportion of pancolitis was found in patients before 30 (20% vs 14.7%, RR = 1.76, 95% CI 0.91-3.4). Younger UC patients had a significantly higher level of education (university degree in 22% vs 8%, P = 0.001).
The predominant form of UC was left sided colitis, which affected almost 80% (n = 183) of the studied population. The most extensive form - pancolitis was present in 34 patients (15%). The extent of UC was age-dependent. The mean age of patients with pancolitis was 38.4±2.4, left side colitis 45.8±1.3 and proctitis 49.2±3.4 years (P = 0.02). There were no significant differences related to CU extent in respect to sex, environment and job (Table 2).
| Proctitis (n = 16) | Left sided colitis (n = 183) | Pancolitis (n = 34) | P | |
| Age of diagnosis (yr) | 49.2 ±3.4 | 45.8 ±1.3 | 38.4 ±2.4 | 0.02 |
| Sex (male/female) | 10/6 | 97/88 | 23 /11 | 0.28 |
| Environment (urban/rural) | 12/4 | 125/58 | 25/9 | 0.80 |
| Labor (manual/intellectual) | 11/6 | 113/56 | 22/12 | 0.35 |
| Surgical/pharmacological treatment | 0/16 | 1/182 | 14/20 | <0.001 |
| Discontinuation of professional activity | 5/11 | 61/122 | 21/13 | 0.02 |
Only 6% of UC patients required surgery, whereas 36% of CD patients underwent surgery (χ2 = 8.15, P<0.005). Patients with more extensive form of UC required more frequent surgical treatment reaching 40% in pancolitis group (Table 2).
Among coexisting disorders, cholelithiasis was the most prevalent and demonstrated in 35 patients (14%), pulmonary disorders were diagnosed in 2% and psoriasis in 1.4%.
Forty-two men (35%) and 45 women (42%) terminated their professional activity because of UC before retirement age. Therefore the overall proportion of patients unable to continue their professional activity due to UC was 0.37 (95% CI 0.31-0.43). The mean age of these patients was 43.4±1.5 years, and did not differ significantly between men (47.1±2.4) and women (43.0±2.5). The highest number of patients who discontinued employment was observed in pancolitis group (62%, P = 0.02 vs other UC extension, Table 2). Another factor affecting job discontinuation was surgical treatment (67% vs 36% of patients with conservative treatment, P = 0.05).
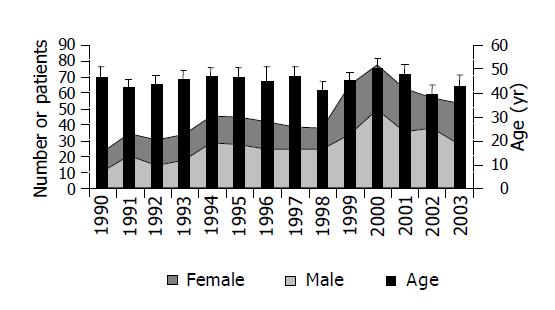
Between 1990 and 1998 the number of IBD patients admitted to the Department of Infectious Diseases was stable (median 61, range 54-73 per year), then slightly increased (median 97, range 80-126 per year, Figure 2). There was no noticeable shift in male/female ratio or patient’s age.
Epidemiology of IBD is known only in a few European countries. Multi-center prospective epidemiologic studies have been conducted mainly in the countries of Western and Southern Europe[5]. Epidemiological data related to IBD in Poland have been published over 20 years before[6-9]. Since then diagnostics and treatment of IBD have undergone some significant changes, which gave us a major impulse to investigate the problem based on the data of IBD patients treated in the Department of Infectious Diseases in Bialystok in 1990-2003.
In 1990-2003 we treated 248 patients. The first immediate observation was the increase of IBD cases in Poland. Previous data from 4 hospitals in North-Western Poland collected between 1965 and 1972 referred to 30 patients with UC and 3 with CD[8]. Another study analyzed 215 IBD patients in 1955-1970[9]. Bartnik[6] treated 406 UC patients between 1955 and 1970. However, it is important to notice that the latest study was conducted in the referral center for digestive diseases throughout the period of 15 years, and their patients originated from the biggest central region of Poland. Our patients came from a small region of Podlasie with a population of over 1 million. In this area there are few other units specializing in treatment of UC, but the majority of patients are usually referred to our hospital.
Increasing of the UC prevalence in the whole world is well documented[4,10]. The Chinese data regarding 10218 UC cases demonstrate a triple increase of UC occurrences. The highest UC prevalence is demonstrated 38-229 cases per 100000 persons in USA and 269 per 100000 in UK[4,11]. In Japan the prevalence rate is 22 per 100000[12]. In Mediterranean countries, both the incidence and the prevalence of ulcerative colitis are much lower: 5.87 per 100000 in urban areas[13]. In another study from Kuwait, UC is demonstrated as an extremely seldom disease[14].
In Polish population, UC is decisively more common than CD (ratio 15/1). Similarly, in most European countries, UC is more common than CD, with a few exceptions in the United Kingdom, France, and Germany[15-17]. CD is less frequently diagnosed than UC also in China (8/66), Greece (42/1300), and Hungary (60/143)[18]. In Spain, in the analyzed population of Gijon, the frequency of CD is only insignificantly lower than UC (46/51)[19]. Similarly, in Hispanic population of Puerto Rico, the frequency of CD varies only slightly from UC (332/499)[20].
The diagnosis of IBD can be made at any age, and CD is diagnosed most frequently in younger patients than UC. It is in accordance with our study, because the age of UC patients is 45 years and CD being 34 years. We have noticed an increase of male patients (1:1.3) whereas in available previous Polish data females predominate (1.4:1)[6,8,9]. However, male predominance is also demonstrated in other studies[10,18].
We demonstrated predominance of IBD patients in the urban population. However, 28% of rural population in our study are much more than 6% in a previous study[9]. Since the majority of urban patients could complete the high school, and the majority of rural patients could only complete their grammar course, we should treat IBD as a mirror of the social structure of our region.
Family history of the disease in UC patients was relatively low (1.6%). However it fits within the window demonstrated by Kaighely[11]. A number of studies suggest that appendectomy is associated with a low risk for subsequent ulcerative colitis. Our study showed that only 2% of patients after appendectomy developed UC. Similarly, a low percentage is documented by Reif[21]. We demonstrated the occurrence of gallbladder stones in 14% of UC patients and 2% of CD patients. Lorusso[22] reported that cholelithiasis is found in 9.6% UC patients and Reif[21] reported that 1.5% UC patients undergo cholecystectomy.
Proctitis was predominant in our patients. Pancolitis was observed usually in the younger population. Similar data are available from different international studies[11,19,23]. As reported in the majority of studies, over 90% of patients responded to pharmacotherapy. Only 6% of our UC patients required surgical treatment, whereas 36% of CD patients underwent surgery.
An interesting observation of our study is that about 37% of the patients retired because of UC regardless of the nature of their employment. Similar figures (32%) are reported in USA and Canada [24,25].
In conclusions the occurrence of UC in Poland is much higher than that of CD. The majority of UC cases are diagnosed in young people (range 20-40 years) with the predominance of male patients. The most common clinical form of UC is left sided colitis.
| 1. | Ehlin AG, Montgomery SM, Ekbom A, Pounder RE, Wakefield AJ. Prevalence of gastrointestinal diseases in two British national birth cohorts. Gut. 2003;52:1117-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Logan RF. Inflammatory bowel disease incidence: up, down or unchanged? Gut. 1998;42:309-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 104] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Trallori G, Palli D, Saieva C, Bardazzi G, Bonanomi AG, d'Albasio G, Galli M, Vannozzi G, Milla M, Tarantino O. A population-based study of inflammatory bowel disease in Florence over 15 years (1978-92). Scand J Gastroenterol. 1996;31:892-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 76] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Loftus EV, Sandborn WJ. Epidemiology of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:1-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 304] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 5. | Shivananda S, Lennard-Jones J, Logan R, Fear N, Price A, Carpenter L, van Blankenstein M. Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD). Gut. 1996;39:690-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 684] [Cited by in RCA: 666] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 6. | Bartnik W, Reguła J, Tomecki R, Butruk E. Results of the treatment of ulcerative colitis during the past 28 years. Pol Arch Med Wewn. 1985;74:340-345. [PubMed] |
| 7. | Bielawski W, Butruk E, Gibiński K, Górski M, Hermanowicz A, Knapik Z, Marlicz K, Pokora J, Popiela T, Radwan P. Nonspecific inflammatory intestinal diseases in Poland and throughout in world. Pol Arch Med Wewn. 1983;70:27-34. [PubMed] |
| 8. | Marlicz K, Kopyłow A, Cwajda H, Majewska M, Sebastyański T. Organic diseases of the large intestine in the patients of three clinics of internal diseases and the Department of Internal Diseases of the City Hospital in Szczecin (author's transl). Przegl Lek. 1975;32:452-456. [PubMed] |
| 9. | Ruzyllo E, Bartnik W, Bakowska Z. Ulcerative colitis--epidemiological data and manifestations. Pol Arch Med Wewn. 1972;49:443-448. [PubMed] |
| 10. | Loftus EV, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Ulcerative colitis in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gut. 2000;46:336-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 360] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 11. | Keighley MR, Stockbrugger RW. Inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18 Suppl 3:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Morita N, Toki S, Hirohashi T, Minoda T, Ogawa K, Kono S, Tamakoshi A, Ohno Y, Sawada T, Muto T. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995;30 Suppl 8:1-4. [PubMed] |
| 13. | Tezel A, Dökmeci G, Eskiocak M, Umit H, Soylu AR. Epidemiological features of ulcerative colitis in Trakya, Turkey. J Int Med Res. 2003;31:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Al-Shamali MA, Kalaoui M, Patty I, Hasan F, Khajah A, Al-Nakib B. Ulcerative colitis in Kuwait: a review of 90 cases. Digestion. 2003;67:218-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Daiss W, Scheurlen M, Malchow H. Epidemiology of inflammatory bowel disease in the county of Tübingen (West Germany). Scand J Gastroenterol Suppl. 1989;170:39-43; discussion 50-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Gower-Rousseau C, Salomez JL, Dupas JL, Marti R, Nuttens MC, Votte A, Lemahieu M, Lemaire B, Colombel JF, Cortot A. Incidence of inflammatory bowel disease in northern France (1988-1990). Gut. 1994;35:1433-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 181] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Rubin GP, Hungin AP, Kelly PJ, Ling J. Inflammatory bowel disease: epidemiology and management in an English general practice population. Aliment Pharmacol Ther. 2000;14:1553-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 197] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 18. | Archimandritis AJ, Kourtesas D, Sougioultziz S, Giontzis A, Grigoriadis P, Davaris P, Tzivras M. Inflammatory bowel disease in Greece-- a hospital-based clinical study of 172 consecutive patients. Med Sci Monit. 2002;8:CR158-CR164. [PubMed] |
| 19. | Saro Gismera C, Riestra Menéndez S, Sánchez Fernández R, Milla Crespo A, Lacort Fernández M, Argüelles Fernández G, Chobak Z, Florido Mancheño JI, Antón Magarzo JL, Altadill Arregui A. Epidemiology in inflammatory bowel disease in five areas of Asturias. Spain. An Med Interna. 2003;20:232-238. [PubMed] |
| 20. | Torres EA, De Jesús R, Pérez CM, Iñesta M, Torres D, Morell C, Just E. Prevalence of inflammatory bowel disease in an insured population in Puerto Rico during 1996. P R Health Sci J. 2003;22:253-258. [PubMed] |
| 21. | Reif S, Lavy A, Keter D, Broide E, Niv Y, Halak A, Ron Y, Eliakim R, Odes S, Patz J. Appendectomy is more frequent but not a risk factor in Crohn's disease while being protective in ulcerative colitis: a comparison of surgical procedures in inflammatory bowel disease. Am J Gastroenterol. 2001;96:829-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Lorusso D, Leo S, Mossa A, Misciagna G, Guerra V. Cholelithiasis in inflammatory bowel disease. A case-control study. Dis Colon Rectum. 1990;33:791-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Souza MH, Troncon LE, Rodrigues CM, Viana CF, Onofre PH, Monteiro RA, Passos AD, Martinelli AL, Meneghelli UG. Trends in the occurrence (1980-1999) and clinical features of Crohn's disease and ulcerative colitis in a university hospital in southeastern Brazil. Arq Gastroenterol. 2002;39:98-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Longobardi T, Jacobs P, Bernstein CN. Work losses related to inflammatory bowel disease in the United States: results from the National Health Interview Survey. Am J Gastroenterol. 2003;98:1064-1072. [PubMed] |
| 25. | Longobardi T, Jacobs P, Wu L, Bernstein CN. Work losses related to inflammatory bowel disease in Canada: results from a National Population Health Survey. Am J Gastroenterol. 2003;98:844-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |