Published online Nov 15, 2004. doi: 10.3748/wjg.v10.i22.3382
Revised: May 4, 2004
Accepted: May 13, 2004
Published online: November 15, 2004
We report a case of caudate lobe hemangioma with an atypical CT enhancement pattern. In the present case, hemangioma exhibited a very subtle discontinuous peripheral rim enhancement at the post-enhanced arterial phase, and the peripheral enhanced zone had a moderately increased enhancement degree and with widened enhancement thickness during the portal-phase and delayed-phase. The slow enhancement rate for this caudate lobe hemangioma was due to sluggish perfusion by the small feeding arteries of caudate lobe branches as demonstrated by angiography.
- Citation: Chen HC, Lee CM, Chen CS, Wu CH. A case of atypical caudate lobe hemangioma mimicking hepatocellular carcinoma: CT and angiographic manifestations. World J Gastroenterol 2004; 10(22): 3382-3384
- URL: https://www.wjgnet.com/1007-9327/full/v10/i22/3382.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i22.3382
Cavernous hemangioma is the most common benign hepatic tumor and usually presents with a typical enhancement pattern when studied by dynamic spiral computed tomography (CT). However, there are a small number of hemangiomas that exhibit atypical enhancement patterns due to the presence of intralesional non-enhanced or less-enhanced components[1-4]. Herein, we report a case of hepatitis B and C with an atypical caudate lobe hemangioma that preoperatively was misdiagnosed as a hepatocellular carcinoma because the caudate lobe mass was supplied by small caudate lobe arteries with very sluggish perfusion, resulting in a slow enhancement rate and atypical enhancement patterns when studied by dynamic CT. CT imaging features and corresponding angiographic findings of the atypical caudate lobe hemangioma were provided.
An asymptomatic 58-year-old woman was found incidentally to have a hepatic mass in the caudate lobe by ultrasound study during a health examination. She was a known hepatitis B carrier (serum positive HBsAg) for 10 years and also known as a hepatitis C carrier (positive IgG anti-HCV) for 1 year. Laboratory evaluation demonstrated normal liver and renal function. The counts of red blood cells, white blood cells, and platelets, coagulation function test, urinalysis, and serum biochemistry profile analysis were normal. The serum alpha-fetoprotein level was not elevated. Abdominal ultrasound detected a 4.0 cm × 4.6 cm inhomogeneous hyperechoic mass situated at the caudate lobe.
Pre- and post-contrast triphasic spiral CT scans were subsequently performed with intravenous administration of a total of 100 mL of contrast material at an injection rate of 2 ml/s via a power injector. Hepatic arterial-phase, portal-phase and delayed-phase were obtained 35, 75 and 180 s, respectively, after the injection of contrast material. Pre-contrast CT revealed a well-circumscribed, low attenuation (attenuation value of 40 HU) ovoid mass (measuring approximately 4.0 cm × 4.6 cm in dimension) occupying the caudate lobe. The mass exhibited a very faint discontinuous peripheral rim enhancement (attenuation value of 76 HU) at the arterial-phase (Figure 1A), with a moderately increased enhancement degree (attenuation value of 110 to 114 HU) and widened enhancement thickness for the enhanced peripheral zone during the portal-phase and delayed-phase (Figures 1B, C). Minimal enhancement (attenuation value of 61 HU) was also noted in the central portion of the mass during the delayed-phase.
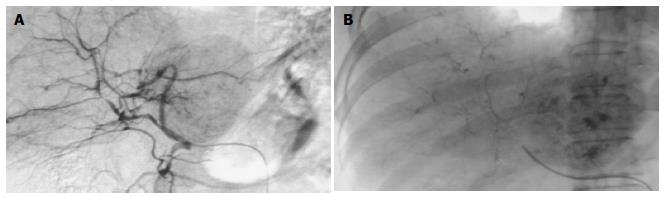
The patient also received a conventional angiographic examination for further evaluation of the caudate lobe mass. Selective proper hepatic angiography showed two small, slightly tortuous, but not enlarged caudate lobe arteries deriving from the right and left hepatic arteries and supplying the caudate lobe mass. Very faint peripheral tumor stains were detected during the late arterial phase (Figure 2A) and parenchymal phase. However, there were no persistent, dense tumor stains at the late venous phase. During the angiographic study, 4 mL of lipiodol (iodized oil) was also slowly injected into the proper hepatic artery and showed several foci of spotty lipiodol retention in the peripheral and central portions of the caudate lobe mass (Figure 2B).
The patient underwent caudate lobe excision under the presumptive diagnosis of hepatocellular carcinoma based on the imaging findings. Pathological examination revealed a cavernous hemangioma occupying the caudate lobe. Only several small foci of organizing thrombi within the hemangioma were discovered.
Cavernous hemangioma is the most common benign hepatic tumor. The vast majority of hepatic hemangiomas present with a typically initial intense peripheral nodular enhancement with gradual central fill-in enhancement when studied by dynamic CT study, and it is easy to differentiate from other hepatic tumors. However a small number of hemangiomas could exhibit atypical enhancement patterns due to the presence of intralesional non-enhanced thrombosis, fibrotic, degenerated or calcified components[1,4]. In addition, variable vascularity of hemangiomas could also influence the lesion's enhancement rate and result in atypical enhancement patterns[2-4]. An atypical hemangioma may mimic a malignant hepatic tumor, causing diagnostic confusion, especially in patients at risk of malignancy.
Previous investigators[2-4] have observed that atypical enhancing hemangiomas were more common for smaller lesions than for larger lesions. Approximately 15.6% to 22.2% of hemangiomas smaller than 2 cm in diameter might have an atypical enhancement pattern of low or iso-attenuation during the post-enhanced arterial and portal venous phases by dynamic CT[2-4]. However, atypical enhancement patterns of large hemangiomas were very rare. Yun et al[2] reported that only 2.2% of hemangiomas larger than 2 cm in diameter presented with atypical enhancement patterns. These reports were correlated with the concept that the presence of typical peripheral nodular enhancement required larger blood supply vessels for hemangiomas and this was associated more with a larger lesion size. Thus, a hemangioma fed by small, not-enlarged supply arteries may fail to exhibit a typical enhancement pattern.
In this present case, although the caudate lobe hemangioma was larger than 4 cm in diameter, the angiograms showed that it was supplied by slightly tortuous, but un-enlarged feeding arteries due to its unique location on an independent hepatic segment of the caudate lobe that only receives the small diameter caudate arterial branches derived from the proximal portion of right and left hepatic arteries. So, this caudate lobe hemangioma failed to exhibit a typical initial peripheral nodular enhancement due to the absence of large feeding arteries. Moreover, the small caudate arteries with their sluggish perfusion also resulted in a slow enhancement rate for the caudate lobe hemangioma. On the post-enhanced arterial-phase, a very faint discontinuous peripheral rim enhancement was noted. During the portal-phase, there was a moderately increased enhancement degree for the enhanced peripheral zone, but the degree of enhancement was not as high as intra-hepatic vessels. At the delayed-phase, complete centripedal fill-in enhancement was not present in the hemangioma, but only a subtle enhancement of the intralesional central portion was noted. The enhancement pattern in the caudate lobe hemangioma thus simulated a well-differentiated hepatocellular carcinoma with delayed pseudocapsule enhancement, because a well-differentiated hepatocellular carcinoma might usually only possess a slightly increased arterial supplement and is not fed by markedly enlarged vessels[5]. Therefore, both a well-differentiated hepatocellular carcinoma and a hemangioma with small feeding arteries may exhibit a similar enhancement pattern on dynamic CT study. However, the thickness of pseudocapsules in a hepatocellular carcinoma was thinner than that of the enhanced peripheral rim in a hemangioma. Furthermore, the increased enhancement degree and the increased enhancement thickness of the intra-lesional peripheral rim also provided a diagnostic clue for the hemangioma with a slow progressive central fill-in enhancement. In contrast, a hepatocellular carcinoma usually exhibited contrast medium washout during the delayed-phase.
MR imaging is superior to CT study to improve diagnostic confidence for hepatic hemangiomas. CT has a sensitivity of 62%-88% and a specificity of 84%-100% (100% when enhancement is isoattenuating to the aorta) for detection of the typical globular enhancement in hemangiomas[6]. However, MR imaging has a higher sensitivity of 98% and a specificity of 98% for detection of the hemangiomas[7]. Some atypical hemangiomas can be diagnosed by MR imaging study. Nevertheless, some atypical hemangiomas will still remain uncertain at MR study due to the presence of intralesional thrombosis, calcified, hyalinized or cystic components that results in the loss of its characteristic appearance of markedly high signal intensity on heavy T2-weighted imaging and present with atypical enhancement patterns on post-enhanced study[8]; and these cases will require biopsy and histopathologic examination.
Except that hemangiomas can exhibit peripheral rim enhancement, the presence of peripheral rim enhancement could also be observed in hepatic metastatic lesions[9].
However, the peripheral rim enhancement in a metastatic lesion often has a serrated margin and not a lobular margin as seen in a hemangioma. Thus, in the present case, the caudate lobe hemangioma had an enhanced peripheral rim with a lobular margin and not a serrated margin allowing it to be differentiated from a metastatic lesion.
As in the present case of a hepatitis carrier at risk for malignancy, CT and MR imaging were considered as complementary imaging study for detection of the malignant hepatic masses. Kang et al[10] reported that although MR imaging study had a higher sensitivity of 95% than that of CT study with a sensitivity of 88% for detection of the hepatocellular carcinomas, However, there was no significant difference in the diagnostic specificity between MR study (97%) and the CT study (98%).
Intra-arterial lipiodol injection has also been used to increase detection of small hepatic neoplasms. Lipiodol retention with a spotty and/or nodular type distribution in the peripheral or central portions of hepatic hemangiomas has been described by Moon et al[11]. However, the presence of spotty lipiodol retention has also been observed in other hepatic tumors, such as focal nodular hyperplasia, metastases and hepatocellular carcinoma. Hepatocellular carcinomas tended to exhibit a peripheral distribution of lipiodol accumulation, rather than a central distribution of lipiodol deposition as seen in hemangiomas. In this present case, conventional angiography failed to demonstrate the typical "cotton-wool" appearance of puddling of contrast material within the large vascular spaces and persisting into the venous phase of a caudate lobe hemangioma. The absence of persistent tumor stains in the hemangioma may be due to its unique location in the hepatic caudate lobe where there is a rapid venous drainage to the adjacent portal vein and inferior vena cava. In such a situation, it is difficult to distinguish a hemangioma from a hepatocellular carcinoma based only on conventional angiographic imaging findings. Whereas, intra-arterial lipiodol injection demonstrated spotty lipiodol retention at the intralesional peripheral and central portions, with a "cotton wool" appearance, and suggested a diagnosis of hemangioma. In addition, the number of lipiodol retention foci was also more pronounced than the number of contrast material stains as seen on conventional angiograms, because the lipiodol materials could be retained in the ectatic and tortuous vascular channels of the hemangioma, thus decreasing its venous washout degree via the portal vein and inferior vena cava. Therefore, intra-arterial lipiodol injection is able to help in the diagnosis of a hemangioma with a rapid venous drainage.
In conclusion, the presence of slow progressive peripheral rim enhancement persisting to the delayed phase, associated with the presence of central distributed spotty lipiodol retention in a caudate lobe mass should give rise to a suspicion of the possibility of hepatic hemangioma. This report emphasizes that a hepatic hemangioma in this unique caudate lobe location can present with an atypical enhancement pattern and resembles a hepatocellular carcinoma. Thus, we recommend that when studying a caudate lobe lesion, a longer post-enhanced delayed time (more than 3 min) is required on CT, in order to reflect its actual vascularity characteristics. In addition, further evaluation by MR study with a long echo time of 150 to 180 ms is also necessary to confirm the diagnosis of a cavernous hemangioma in order to prevent inappropriate therapeutic decision making.
Edited by Wang XL Proofread by Zhu LH and Xu FM
| 1. | Mitsudo K, Watanabe Y, Saga T, Dohke M, Sato N, Minami K, Shigeyasu M. Nonenhanced hepatic cavernous hemangioma with multiple calcifications: CT and pathologic correlation. Abdom Imaging. 1995;20:459-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Yun EJ, Choi BI, Han JK, Jang HJ, Kim TK, Yeon KM, Han MC. Hepatic hemangioma: contrast-enhancement pattern during the arterial and portal venous phases of spiral CT. Abdom Imaging. 1999;24:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Hanafusa K, Ohashi I, Himeno Y, Suzuki S, Shibuya H. Hepatic hemangioma: findings with two-phase CT. Radiology. 1995;196:465-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 109] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | van Leeuwen MS, Noordzij J, Feldberg MA, Hennipman AH, Doornewaard H. Focal liver lesions: characterization with triphasic spiral CT. Radiology. 1996;201:327-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 92] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Hwang GJ, Kim MJ, Yoo HS, Lee JT. Nodular hepatocellular carcinomas: detection with arterial-, portal-, and delayed-phase images at spiral CT. Radiology. 1997;202:383-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Leslie DF, Johnson CD, Johnson CM, Ilstrup DM, Harmsen WS. Distinction between cavernous hemangiomas of the liver and hepatic metastases on CT: value of contrast enhancement patterns. AJR Am J Roentgenol. 1995;164:625-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 85] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Soyer P, Gueye C, Somveille E, Laissy JP, Scherrer A. MR diagnosis of hepatic metastases from neuroendocrine tumors versus hemangiomas: relative merits of dynamic gadolinium chelate-enhanced gradient-recalled echo and unenhanced spin-echo images. AJR Am J Roentgenol. 1995;165:1407-1413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 66] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Vilgrain V, Boulos L, Vullierme MP, Denys A, Terris B, Menu Y. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics. 2000;20:379-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 257] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 9. | Mitchell DG, Saini S, Weinreb J, De Lange EE, Runge VM, Kuhlman JE, Parisky Y, Johnson CD, Brown JJ, Schnall M. Hepatic metastases and cavernous hemangiomas: distinction with standard- and triple-dose gadoteridol-enhanced MR imaging. Radiology. 1994;193:49-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 90] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Kang BK, Lim JH, Kim SH, Choi D, Lim HK, Lee WJ, Lee SJ. Preoperative depiction of hepatocellular carcinoma: ferumoxides-enhanced MR imaging versus triple-phase helical CT. Radiology. 2003;226:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Moon WK, Choi BI, Han JK, Kim SH, Chung JW, Park JH, Han MC. Iodized-oil retention within hepatic hemangioma: characteristics on iodized-oil CT. Abdom Imaging. 1996;21:420-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |