Published online Sep 1, 2004. doi: 10.3748/wjg.v10.i17.2535
Revised: April 4, 2004
Accepted: April 29, 2004
Published online: September 1, 2004
AIM: To evaluate the relationships between the personal, sociocultural, and environmental characteristics, and the presence or absence of symptoms with the detection of Enterobius vermicularis (E. vermicularis) in a population sample in our region (General Mansilla, Province of Buenos Aires, Argentina), by individual and familiar analyses.
METHODS: E. vermicularis was diagnosed in 309 people from 70 family units residing in the urban area and the rural area of the city of General Mansilla. Each of them was surveyed so as to register personal, environmental and sociocultural data. Questions about the presence or absence of anal itch, abdominal pain and sleeping disorder were also asked. Significant associations were determined by square chi tests. Logistic regression models were adjusted by using a backward conditional stepwise method to determine the presence of this parasite in the individuals and in the families.
RESULTS: The parasites were found in 29.12% (90/309) of the individuals, with a frequency of 14.28% (20/140) among the heads of the families and of 41.42% (70/169) among the children. The only variables showing a significant association were affiliation, where the risk category was "being the son/daughter of", and the symptoms were abdominal pain, sleeping disorder, and anal itch. Families with a member infected with parasite were considered Positive Families (PF) and they were 40/70 (57.14%), only 5% (2/40) of the PF had 100% of their members infected with the parasite. The logistic regression models applied showed that the risk categories were mainly affiliation (son/daughter) and housing (satisfactory) among others.
CONCLUSION: The presence of E. vermicularis was proved in one third of the studied population. The frequency of families with all their members infected with the parasite was very low. Most of the studied personal, sociocultural, and environmental variables did not turn out to be significantly associated with the presence of the parasite. An association with the category of "son/daughter" and housing classified as "satisfactory" was determined. The latter may be due to the fact that the people living in that category of housing have hygienic practices at home that favour the distribution of the eggs in the environment. The presence of the analysed symptoms was associated with the presence of the parasite, thus strengthening the need of periodical control of the population showing at least one of these symptoms.
-
Citation: Pezzani BC, Minvielle MC, Luca MM, Córdoba MA, Apezteguía MC, Basualdo JA.
Enterobius vermicularis infection among population of General Mansilla, Argentina. World J Gastroenterol 2004; 10(17): 2535-2539 - URL: https://www.wjgnet.com/1007-9327/full/v10/i17/2535.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i17.2535
Enterobius vermicularis (E. vermicularis) is a small whitish nematode whose evolution cycle differs from other intestinal helminths in the biological peculiarities[1].
Enterobiosis is a cosmopolitan parasitosis. The peculiar biology of E. vermicularis contributes to the creation of contamination foci around the infected resident and the re-infections. The intra-family or cohabitating members' infection is very frequent. The most important infection routes are through oral and respiratory tract. The oral infection included the anus-hand-mouth route, onychophagia and/or ingestion of contaminated food. The respiratory tract infection would be from inhaling dust contaminated with the parasite eggs[2].
The main source of contamination inside the house is found in the environmental dust and carried by children. This would be one of the infection routes for the family units.
It has been reported that no sex difference existed in the infection rates. The teen-age, however, infection rates remain unchanged in boys but decrease among girls, since girls start observing hygienic practices with higher precocity than boys[3,4]. Among adults, the infection frequency is similar in both sexes, but it was commonly observed that many adults seemed not to get infected even when subjected to contaminated environments due to personal hygiene[1-5].
Waste disposal little affects the distribution of the infection, since the oxyurus eggs are not found in excrement. Several groups in the population may be infected without depending on the socioeconomic conditions and environmental hygiene due to the biological characteristics of this parasite[6,7].
Generally, this parasitosis is an asymptomatic illness, and in those cases where clinical manifestations are present, anal itch is the most frequent symptom. Indirectly, and mainly in children, it produces insomnia, fatigue and irritability, and sometimes abdominal pain[2-8,9].
The objective of this study was to evaluate the relationship between the personal, socio-cultural and environmental characteristics, presence or absence of symptoms, and the detection of E. vermicularis in a sample population in our region (Province of Buenos Aires, Argentina), through individual and family analysis.
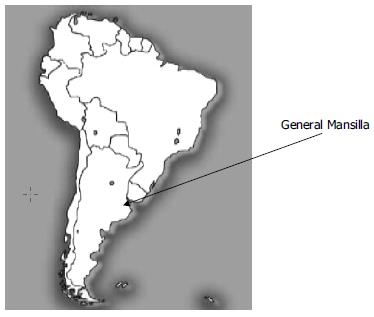
The city of General Mansilla is located in the northeast of the Province of Buenos Aires, in the central-western area of the Argentine Republic (South America), 96 km from the city of Buenos Aires. Population is 2300 in the urban area and 1700 in the rural area. The urban area covers 250 hectares and the rural population is settled in a 15 km range around it (Figure 1).
A total of 309 people constituting 70 family units, made up by mother, father and children (1 to 6 per family), were studied. Fifty families were analyzed from the urban area (221 people) and 20 from the rural area (88 people). Each member of the family was surveyed to record personal, environmental and socio-cultural data. The following variables were assessed: a) personal: sex, age, affiliation of each member, and number of children in each family; b) socio-cultural and environmental: habitat (urban area - rural area), water supply (water pump - running water), disposal of waste (sewer - no sewer), housing (satisfactory - unsatisfactory), home garbage (collected - not collected), bathroom (existent - non-existent), and overcrowding (yes - no). Housing was considered satisfactory when built of masonry with cement floors, and unsatisfactory when built of wood and/or metal with dirt floors. Overcrowding was considered when more than three individuals slept together in the same room. Besides, questions were asked about the presence or absence of the following symptoms: anal itch, abdominal pain and sleeping disorders, since they are considered to be typical of this parasitosis.
A perianal swab method was performed to each surveyed individual for the detection of E. vermicularis. Each surveyed person was given five 10 cm × 10 cm gauze pads and a bottle of 5% formaldehyde. At the same time, they were explained the procedure for sample taking. In the case of minors, instructions were given to their parents. Each of the testee collected the sample before getting up for 5 consecutive days, each day rubbing a gauze pad previously imbibed in water, on the perianal margins. Then, they put the sample in the container with formaldehyde and sent it to the lab.
The association between each of the variables studied and the presence of E. vermicularis was analyzed by means of the chi square test. In the case of finding statistically significant associations, the odds ratio (OR) was calculated.
Logistic regression models were adjusted by using backward conditional stepwise method to determine the presence of E. vermicularis in individuals and in families. In the case of individuals (total, rural and urban), socio-cultural and environmental characteristics, symptoms, age and sex were used as (independent) explanatory variables. In the case of families, only socio-cultural and environmental characteristics and affiliation were used. The logistic regression model predicts the probability of being infected with E.vermicularis according to the explanatory variables. From this prediction, individuals are classified according to their risk of infection as: high risk (when the probability is higher than 0.5), and low risk (when the probability is lower than 0.5). For this classification, sensitivity (S), specificity (E), positive predictive value and negative predictive value, and global adjustment (total percentage of correct predictions) in each of the models were estimated. The model can be used to obtain OR estimators for each variable. SPSS (Statistical Package for the Social Sciences) software version 11.5 was used.
The frequency of infected people in the total studied population (309) was 29.12% (90/309). Among the parents, it was 14.28% (20/140) and 41.42% (70/169) among the children.
Families with at least one infected member were called positive families (PF) and the rest, negative families (NF). The number of PF was 40/70 (57.14%). Of these, 8 families presented less than 25% of their members with the parasite, 20 had 26%-50%, 6 between 51% and 75%, 4 between 76% and 99% and only two had 100% of their members infected.
The mean age of parents from PF and NF was 32.3 and 33.6, respectively. The mean age for children from PF and NF was 8.48 and 7.71, respectively. The mean age of positive children was 6.85. Thirty percent (12/40) of the mothers from PF were infected while only 20% (8/40) of the fathers were infected. Prevalence for adults from PF was 25% (20/80).
The number of children from PF was 103. Of these, 67.96% (70/103) were positive and 52.85% (37/70) were male. The number of children from NF was 66, 48.48% (32/66) of which were male.
The results obtained from socio-cultural and environmental aspects both from PF and NF and their statistical analysis are shown in Table 1.
| Variable | PF (n = 40) | FN (n = 30) | P | |
| Habitat | Urban | 29 (72.5) | 21 (70) | 0.8188 |
| Rural | 11 (27.5) | 9 (30) | ||
| Water supply | Water pump | 12 (30) | 13 (43.33) | 0.2493 |
| Running water | 28 (70) | 17 (56.66) | ||
| Disposal of waste | Sewer | 14 (35) | 8 (26.66) | 0.4573 |
| No sewer | 26 (65) | 22 (73.33) | ||
| 1Housing | Satisfactory | 30 (75) | 20 (66.66) | 0.4450 |
| Unsatisfactory | 10 (25) | 10 (33.33) | ||
| Garbage | Collected | 28 (70) | 21 (70) | 1.0000 |
| Not collected | 12 (30) | 9 (30) | ||
| Bathroom | Existent | 25 (62.5) | 22 (73.33) | 0.3396 |
| Non-existent | 15 (37.5) | 8 (26.66) | ||
| 2Overcrowding | Yes | 17 (42.5) | 9 (30) | 0.2841 |
| No | 23 (57.5) | 21 (60) |
When analyzing the association between the presence of E.vermicularis and each variable separately, the only one showing statistically significant association was affiliation, where the risk category was being the son/daughter (P = 0.000, OR = 4.242), and the symptoms of abdominal pain (P = 0.001, OR = 2.680), sleeping disorders (P = 0.003, OR = 2.339), and anal itch (P = 0.001, OR = 2.662).
Table 2 (a, b, c and d) shows the results from the logistic regression models built for the total of individuals, those residing in the urban area, those living in the rural area, and the families.
| Variable | Risk category | Coefficient | Odds Ratio |
| For the total of individuals, n = 309 | |||
| Affiliation | Son/daughter | 1.267 | 3.550 |
| Housing | Satisfactory | 0.829 | 2.288 |
| Garbage | Not collected | 1.372 | 3.944 |
| Water | Running | 0.951 | 2.591 |
| Abdominal pain | Present | 0.555 | 1.742 |
| Sleeping disorders | Present | 0.561 | 1.752 |
| Constant | -1.825 | ||
| For rural individuals, n = 88 | |||
| Affiliation | Son/daughter | 10.246 | 28 167 |
| Housing | Satisfactory | 2.857 | 17.5 |
| Age (yr) | Eldest son/daughter | 0.316 | 1.372 |
| Bathroom | Non-existent | 2.160 | 8.670 |
| Sleeping disorders | Present | 1.967 | 7.151 |
| Constant | -12.493 | ||
| For urban individuals, n = 221 | |||
| Affiliation | Son/daughter | 1.176 | 3.241 |
| Housing | Satisfactory | 0.917 | 2.5 |
| Water | Running | 1.372 | 3.937 |
| Abdominal pain | Present | 0.690 | 1.993 |
| Constant | -1.612 | ||
| For positive families, n = 40 | |||
| Housing | Satisfactory | 2.749 | 15.625 |
| Water | Running | 2.614 | 13.699 |
| Garbage | Not collected | 2.75 | 15.636 |
| Bathroom | Non-existent | 2.403 | 11.056 |
| Constant | 0.338 | ||
(1) In the whole population, the affiliation variable was the most significant, that is, children had greater probability of being infected than parents. In order of importance, the variables garbage collection and type of housing followed. Type of water supply and symptoms of abdominal pain and sleeping disorders turned out to be of lesser importance. This model classified 22.2% of the infected individuals (S) and 92.2% of the non-infected individuals (E) correctly. Globally, it classified 71.8% of the individuals correctly.
(2) Among the rural population the affiliation variable had an even higher significance degree. It also turned out to be important age variable. This continuous variable had a positive coefficient, which implies that at an older age there is more risk to be infected. But being the affiliation variable present, older children are those with the higher risk of being infected. In order of importance, the symptom of sleeping disorders, type of housing and no bathroom available followed. This model classified 53.8% of the positive individuals (S), and 93.3% of the non-infected individuals (E) correctly. Globally, it classified 81.4% of the individuals correctly.
(3) Among the urban population, the affiliation variable was also the most significant. The symptom of abdominal pain, type of water supply and type of housing followed. This model classified 23.4% of the infected individuals (S) and 89.3% of the non-infected individuals (E) correctly. Globally, it classified 70.4% of the individuals correctly.
(4) Among the positive families, the variables of garbage collection, housing, water supply and bathroom had a similar degree of significance. This model classified 95% of the infected families (S) and 23% of the non-infected families (E) correctly. Globally, it classified 64.3% of the families correctly.
Regarding the three studied symptoms, the analysis showed anal itch in 19.41% (60/309) of the people. Of them, 27/60 (45%) were positive for E. vermicularis (P = 0.0026, OR = 2.42), 12/60 (20%) were negative but belonged to a PF, and 21/60 (35%) were negative from NF. The presence of sleeping disorders was shown in 22.65% (79/309) of the studied population, 30/70 (42.85%) (P = 0.0040, OR = 2.24) of which were parasite infected, 17/70 (24.28%) showed no parasites but belonged to a PF, and 23/70 (32.85%) were negative from NF.
Abdominal pain was detected in 19.41% (60/309) of the testees, 28/60 (46.66%) (P = 0.009, OR = 2.64) of which were parasite infected individuals, 12/60 (20%) were negative for the parasite test but belonged to a PF, and 20/60 (33.33%) were negative from NF.
In the present study a high frequency of infection was found for E. vermicularis, going from 29.12% in the total population up to 41.42% if only the child population considered. These percentages are higher than those published in other countries. In Korea, a prevalence of this parasitosis was reported in 9.8% of school children[10], 9.2% in pre-schoolers[3], 14.8 in kindergarten children[11], 12.6% in school children in the rural area[4]. and 9.8% in children of school age[12]. In the town of Chennai, India, a prevalence of 0.50% was reported[13] in school age children. In Thailand, in 5- to 10-year-old children, the prevalence was 21.91%[7]. In Taiwan it was 11% in school age children[14]. A prevalence of 10.5% was found for children between 7 and 13 years old in Turkey[15]. A study carried out in 18- to 35-year-old adults in Malaysia, Kuala Lumpur, reported a frequency of 9.2%[16,17]. In Poland, the frequency among 7-year-old children was 16.45%[19]. And in Sweden, it was 21% in children from primary care centres[18].
In America, a study carried out in New York (United States) on the prevalence of E.vermicularis in mentally and developmentally retarded children showed a prevalence of 4.5%[19]. In Venezuela, the prevalence found in 5- to 14-year-old children was 19.1%[20], and in Peru it was 1.1% in adults and children from different communities[21]. In Argentina, a study carried out in two aboriginal communities from the province of Misiones, a prevalence of 0% and 5% for E. vermicularis was shown[22]. In the Province of La Rioja, a percentage of 14.8% was reported in middle-class children[23], and in the city of Buenos Aires, 20.50% was reported in hospital population[24]. In Neuquen (Patagonia), 18.8% was reported in adults and children from deprived neighbourhoods[25].
However, the high frequency shown in our study is similar to that reported by Norhayati et al[26] in 1994 in Malaysia (40.4%), Nithikathkul et al[6]. in 2001 in Thailand (38.82%), Bahader et al[27] in 1995 in Egypt (43.8%), Gilman et al[28] in 1991 in Peru (42.0%), and Mercado et al[29] in 1996 in Chile (35.2%) on studies done in diverse populations.
This study did not show significant sex and age differences regarding parasite infected parents, but there was a higher frequency among the mothers, probably due to the greater daily contact with their parasite infected children (regular behaviour among the inhabitants of this region).
The children had a higher probability of being infected than the parents. As to the infected children, no statistically verifiable differences could be found regarding sex or age but, unlike the parents, the highest level of infected people were male, probably in association with different hygienic practices for each sex. This difference agrees with Yoon et al's[3] report about 10.1% of boys and 8.1% of girls with parasites, and Kim et al's[10] about 10.8% in male and 8.7% in female schoolchildren. However, Kim[10] reports 7.1% and 12.5% positive values for male and female kindergarten children, respectively. In our study, parasite infected kindergarten infantile population, sex distribution was 50% (13/26).
Among the PF there was a high percentage of non-infected parents and only 5% of these families had all of their members infected. With these results we could infer that when someone is detected to have parasites, the treatment of all the members of his/her family is not necessary, especially if we take into account that the cost of the treatment has to be afforded by each family in our region. This would make a regular control of the population so as to detect positive cases and treat them appropriately and thus reduce the prevalence of this parasitosis.
Socio-cultural and environmental factors studied in this study showed no statistically significant associations between PF and NF, which are in agreement with Nithikathkul et al[7] not with Kim et al[10].
Overcrowding was significantly associated for Acosta et al[1] (P < 0.001) with this parasitosis in children in Venezuela, but this association could not be shown in our study, in agreement with Norhayati et al's[26] findings in children in Malaysia.
In this study, a significant association was proved by the presence of anal itch, sleeping disorders and abdominal pain, and the detection of this parasite. But these symptoms were not exclusive for the parasite-infected population since 20% to 35% of the non-parasite infected people showed at least one of these symptoms. Venezuela[1] reported that 53.9% of the parasite-infected population showed anal itch.
As a conclusion of this work we point out that enterobiosis was present in a percentage close to 30% of the general population and over 40% in children in our region (Province of Buenos Aires, Argentina).
Contrary to what was expected, the risk of getting this helminthosis was not related to age, sex, or most of the socio-cultural and environmental factors studied (habitat, consumption water, disposal of waste, garbage collection, bathroom characteristics and overcrowding). An association was determined between the variable affiliations, where the risk category was "being the son/daughter of".
The type of housing categorized as "satisfactory" was also related to this parasitosis. This contradictory situation could be due to the fact that people living in this type of housing show hygienic practices in the home favouring the distribution of eggs in the atmosphere (e.g., shaking the sheets, using a feather dust for cleaning, etc.)
These results also strengthen the need of regular control of the population reporting at least one of these symptoms: anal itch, sleeping disorders, and/or abdominal pain.
The authors wish to thank Dr. Roberto Zungri for his permanent "field work" contribution to this study.
Edited by Chen WW Proofread by Xu FM
| 1. | Acosta M, Cazorla D, Garvett M. [Enterobiasis among schoolchildren in a rural population from Estado Falcón, Venezuela, and its relation with socioeconomic level]. Invest Clin. 2002;43:173-181. [PubMed] |
| 2. | Atias A. Enterobiosis u Oxiuriosis. In: Atías A, editor. Parasitología Médica. Editorial Mediterráneo, Santiago, Chile. 1999;188-193. |
| 3. | Yoon HJ, Choi YJ, Lee SU, Park HY, Huh S, Yang YS. Enterobius vermicularis egg positive rate of pre-school children in Chunchon, Korea (1999). Korean J Parasitol. 2000;38:279-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 4. | Kim BJ, Yeon JW, Ock MS. Infection rates of Enterobius vermicularis and Clonorchis sinensis of primary school children in Hamyang-gun, Gyeongsangnam-do (province), Korea. Korean J Parasitol. 2001;39:323-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Smolyakov R, Talalay B, Yanai-Inbar I, Pak I, Alkan M. Enterobius vermicularis infection of female genital tract: a report of three cases and review of literature. Eur J Obstet Gynecol Reprod Biol. 2003;107:220-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Nithikathkul C, Changsap B, Wannapinyosheep S, Poister C, Boontan P. The prevalence of Enterobius vermicularis among primary school students in Samut Prakan Province, Thailand. Southeast Asian J Trop Med Public Health. 2001;32 Suppl 2:133-137. [PubMed] |
| 7. | Nithikathkul C, Changsap B, Wannapinyosheep S, Poister C, Boontan P. The prevalence of enterobiasis in children attending mobile health clinic of Huachiew Chalermprakiet University. Southeast Asian J Trop Med Public Health. 2001;32 Suppl 2:138-142. [PubMed] |
| 8. | Grencis RK, Cooper ES. Enterobius, trichuris, capillaria, and hookworm including ancylostoma caninum. Gastroenterol Clin North Am. 1996;25:579-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Nokes C, Bundy DA. Compliance and absenteeism in school children: implications for helminth control. Trans R Soc Trop Med Hyg. 1993;87:148-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Kim BJ, Lee BY, Chung HK, Lee YS, Lee KH, Chung HJ, Ock MS. Egg positive rate of Enterobius vermicularis of primary school children in Geoje island. Korean J Parasitol. 2003;41:75-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Lee KJ, Lee IY, Im K. Enterobius vermicularis egg positive rate in a primary school in Chungchongnam-do (province) in Korea. Korean J Parasitol. 2000;38:177-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Lee KJ, Ahn YK, Ryang YS. Enterobius vermicularis egg positive rates in primary school children in Gangwon-do (province), Korea. Korean J Parasitol. 2001;39:327-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Fernandez MC, Verghese S, Bhuvaneswari R, Elizabeth SJ, Mathew T, Anitha A, Chitra AK. A comparative study of the intestinal parasites prevalent among children living in rural and urban settings in and around Chennai. J Commun Dis. 2002;34:35-39. [PubMed] |
| 14. | Fan PC. Review of enterobiasis in Taiwan and offshore islands. J Microbiol Immunol Infect. 1998;31:203-210. [PubMed] |
| 15. | Gürses N, Ozkan Y, Pekşen Y, Uysal S, Aydin M. [Intestinal parasites in primary schools of different socioeconomic status and environmental conditions]. Mikrobiyol Bul. 1991;25:57-62. [PubMed] |
| 16. | Oothuman P, Noor Hayati MI, Mastura MH, Rampal L, Jeffery J, Rubiah M, Ismail G, Fatmah MS. Prevalence of Enterobius vermicularis amongst adults living in hostels by six successive day examination. Southeast Asian J Trop Med Public Health. 1992;23:82-86. [PubMed] |
| 17. | Płonka W, Dzbeński TH. [The occurrence of intestinal parasites among children attending first classes of the elementary schools in Poland in the school year 1997/1998]. Przegl Epidemiol. 1999;53:331-338. [PubMed] |
| 18. | Herrström P, Friström A, Karlsson A, Högstedt B. Enterobius vermicularis and finger sucking in young Swedish children. Scand J Prim Health Care. 1997;15:146-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Schupf N, Ortiz M, Kapell D, Kiely M, Rudelli RD. Prevalence of intestinal parasite infections among individuals with mental retardation in New York State. Ment Retard. 1995;33:84-89. [PubMed] |
| 20. | Devera R, Pérez C, Ramos Y. [Enterobiasis in students from Ciudad Bolivar, Venezuela]. Bol Chil Parasitol. 1998;53:14-18. [PubMed] |
| 21. | Maco Flores V, Marcos Raymundo LA, Terashima Iwashita A, Samalvides Cuba F, Gotuzzo Herencia E. [Distribution of entero-parasitic infections in the Peruvian Highland: study carried out in six rural communities of the department of Puno, Peru]. Rev Gastroenterol Peru. 2002;22:304-309. [PubMed] |
| 22. | Ilkow C, Digiani MC, Navone GT. Prevalencias y cargas parasitarias intestinales en dos comunidades mbya guaraní (provincia de Misiones, Argentina). [Intestinal prevalences and burden in two mbya guaraní communities-province of Misiones, Argentina)] 3º Congreso Argentino de Parasitología 2000. Libro de Resúmenes. Tomo II, p 393. . |
| 23. | Flores J, Páez S, Toro A, Bellegarde E, Córdoba P. Prevalencia de Enterobius vermicularis en la capital de la provincia de la rioja. [Prevalence of Enterobius vermicularis in the capital city of La Rioja´s province ] 3º Congreso Argentino de Parasitologia 2002. Libro de Resúmenes. Tomo II, p 418. . |
| 24. | Menghi C, Clementel V, Zadcovich S, Gatta C, Fernández GG, Szmulewicz G, Mendez O. Enteroparasitosis halladas en una población asistida en un hospital de la ciudad de Buenos Aires. [Enteroparasitoses in hospital population of Buenos Aires city] 3º Congreso Argentino de Parasitología 2000. Libro de Resúmenes. Tomo II, p 425. . |
| 25. | Soriano SV, Barbieri LM, Pierángeli NB, Giayetto AL, Manacorda AM, Castronovo E, Pezzani BC, Minvielle M, Basualdo JA. Intestinal parasites and the environment: frequency of intestinal parasites in children of Neuquén, Patagonia, Argentina. Rev Latinoam Microbiol. 2001;43:96-101. [PubMed] |
| 26. | Norhayati M, Hayati MI, Oothuman P, Azizi O, Fatmah MS, Ismail G, Minudin YM. Enterobius vermicularis infection among children aged 1-8 years in a rural area in Malaysia. Southeast Asian J Trop Med Public Health. 1994;25:494-497. [PubMed] |
| 27. | Bahader SM, Ali GS, Shaalan AH, Khalil HM, Khalil NM. "Effects of Enterobius vermicularis infection on intelligence quotient (I.Q) and anthropometric measurements of Egyptian rural children". J Egypt Soc Parasitol. 1995;25:183-194. [PubMed] |
| 28. | Gilman RH, Marquis GS, Miranda E. Prevalence and symptoms of Enterobius vermicularis infections in a Peruvian shanty town. Trans R Soc Trop Med Hyg. 1991;85:761-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Mercado R, García M. [Various epidemiological aspects of Enterobius vermicularis infection inpatients served at public outpatient clinics and hospitals from the northern section of Santiago, Chile, 1995]. Bol Chil Parasitol. 1996;51:91-94. [PubMed] |