Copyright
©The Author(s) 2000.
World J Gastroenterol. Apr 15, 2000; 6(2): 157-168
Published online Apr 15, 2000. doi: 10.3748/wjg.v6.i2.157
Published online Apr 15, 2000. doi: 10.3748/wjg.v6.i2.157
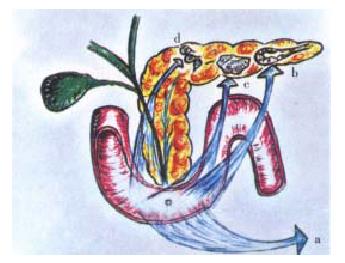
Figure 1 A schematic representation of the duodeno-pancreas.
The image pedagogically resorted to is that of a revolver with its trigger represented by the peri-Vaterian duodenum (a) and the bullets by the pancreon units (b) and the Langerhans islets (c). The intrapancreatic ganglia (d) are also depicted. The latter integrate different nervous arc reflexes and are pivotal in the generation of the intrapancreatic cholinergic tone.
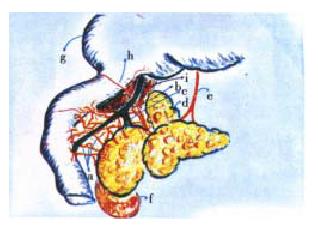
Figure 2 Some anatomical features of the opossum: rich density of nerve fibres jumping the duodeno-pancreatic cleft (a).
The joining of the main pancreatic duct (c) with the bile duct (b) giving origin to a long common bile-pancreatic segment before reaching the outlet into the duodenum. The presence of an extension of the pancreatic gland into the hepatic hilum (d). Arriving to the pancreas of the vagus nerve (e). Right kidney (f). Stomach dis placed upward and to the right (g). Duodenal and pyloric branches of the hepatic artery (h). Liver (i)
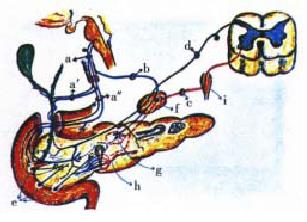
Figure 3 Complex nervous systems that innervate the extrahepatic bile ducts and the duodeno-pancreas.
Vagal: Left or anterior vagus nerve (a). Hepatic branch (a′). Gastric branch (a″). Celiac collateral of the right or posterior vagus (b). Splanchnic-celiac: Pre-ganglionic fibre (c). Celiac ganglion with post-ganglionic neuron (f). Sensory-afferent: Afferent fi bres and neurons of the dorsal roots ganglia of the spinal cord nerves (f). Entero-pancreatic: Nerve fibres connecting the neurons of the enteric plexus with the pancreatic gland (e). Parasympathetic synapses in the intrapancreatic ganglion (g). Arterio-venous shunts of the pancreas’ microcirculation system (h). Ganglia of the sympathetic chain (i)
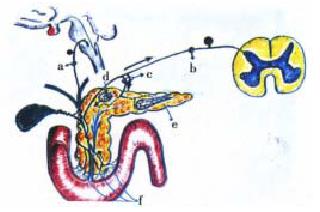
Figure 4 Physiopathogenesis of biliary acute pancrea titis.
Activation of autonomic-arc-reflexes. A: Sympatho-ischemic reflexes. Trigger of the pancreatic revolver, the peri-Vaterian duodenum region (a). Entero-celiac reflex (b). Celiac-pancreatic reflex (c) giving the origin to the opening of the arterio-venous shunts in the pancreatic gland microcirculation. Ce liac ganglia (f)
Figure 5 Activation of autonomic-arc-reflexes.
B: Pseudo-axonic reflex. Afferent nerve fibres of the vagal nervous complex (nodose ganglion) (a). Afferent nerve fibres of the splanchnic-celiac nervous complex (b). Antidromic discharge through a collateral nervous branch (c). Degranulation of mast cells (d). Pancreon units (e). Afferent nerve fibres of the peri-Vaterian duodenum, the trigger zone
Figure 6 Disruption of the entero-pancreatic feedback loop.
A: Normal condition: Brake of CCK release. Direct brake (trypsin, chymotripsin) of the CCK-releasing peptide and of the monitor peptide (a). Indirect brake (bilis). Stabilization of trypsin and chymot rypsin (b). Bile-pancreatic secretion activation of a negative duodeno-pancre atic reflex (c). B: Bile-pancreatic duct obstruction condition-Loss of the normal bile-pancreatic secretion-evoked brake of CCK release. Stone impactation in the Vaterian papilla (a). CCK-induced paracrine-neural duode no-pancreatic reflex (b). CCK-elicited hormonal activation of pancreon units (c). Neural (b) and hormonal (c) mechanisms. Neural (b) and hormonal (c) pathway to the CCK-evoked supramaximal stimulation of the acinar component of the panc reon units.
Figure 7 Experimental mimicking of biliary acute pan creatitis in rats.
Modification of the classical Pfeffer method (closed duodenal loop), the temporary or short term closed duodenal loop method. Filling of a duodenal loop (a) through the gastric antrum (b) with 7% sodium taurocholate and a few drops of meth ylene blue, at constant pressure. Height of liquid infusion column = 110 cm (c)
- Citation: Tiscornia OM, Hamamura S, Lehmann ES, Otero G, Waisman H, Tiscornia-Wasserman P, Bank S. Biliary acute pancreatitis: A review. World J Gastroenterol 2000; 6(2): 157-168
- URL: https://www.wjgnet.com/1007-9327/full/v6/i2/157.htm
- DOI: https://dx.doi.org/10.3748/wjg.v6.i2.157