Copyright
©The Author(s) 1999.
World J Gastroenterol. Dec 15, 1999; 5(6): 492-505
Published online Dec 15, 1999. doi: 10.3748/wjg.v5.i6.492
Published online Dec 15, 1999. doi: 10.3748/wjg.v5.i6.492
Figure 1 ① After intratumoral injection of 32P-GMS, SPECT revealed radioactive image condensed in the tumor but not in the non-target tissue.
② On the 14th day tumor in treatment group shrank prominen tly. ③ Increased in size and plenty of blood supply in control group.
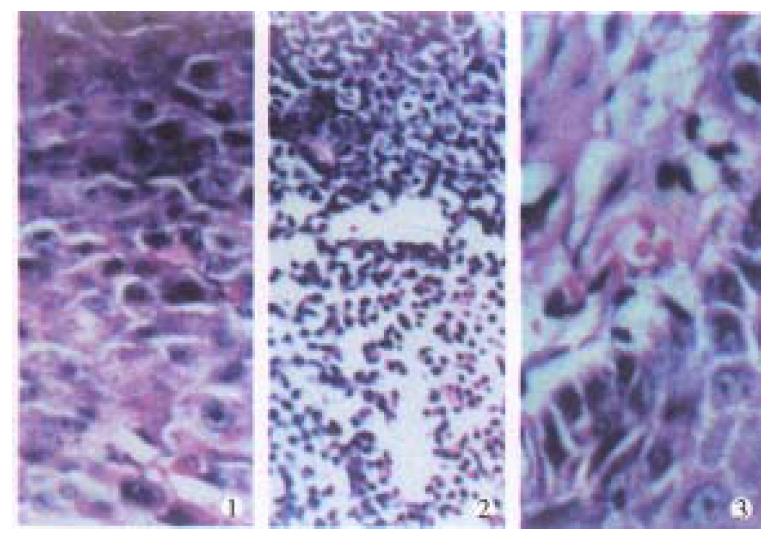
Figure 2 On the 14th day, ① Control group tumor cells densely arranged and actively growing (HE × 100).
② Treatment group, tumor cells in coagulation necrosis (HE×100). ③ Treatment group, radiation injury in neighboring epidermal tissue (HE × 200).
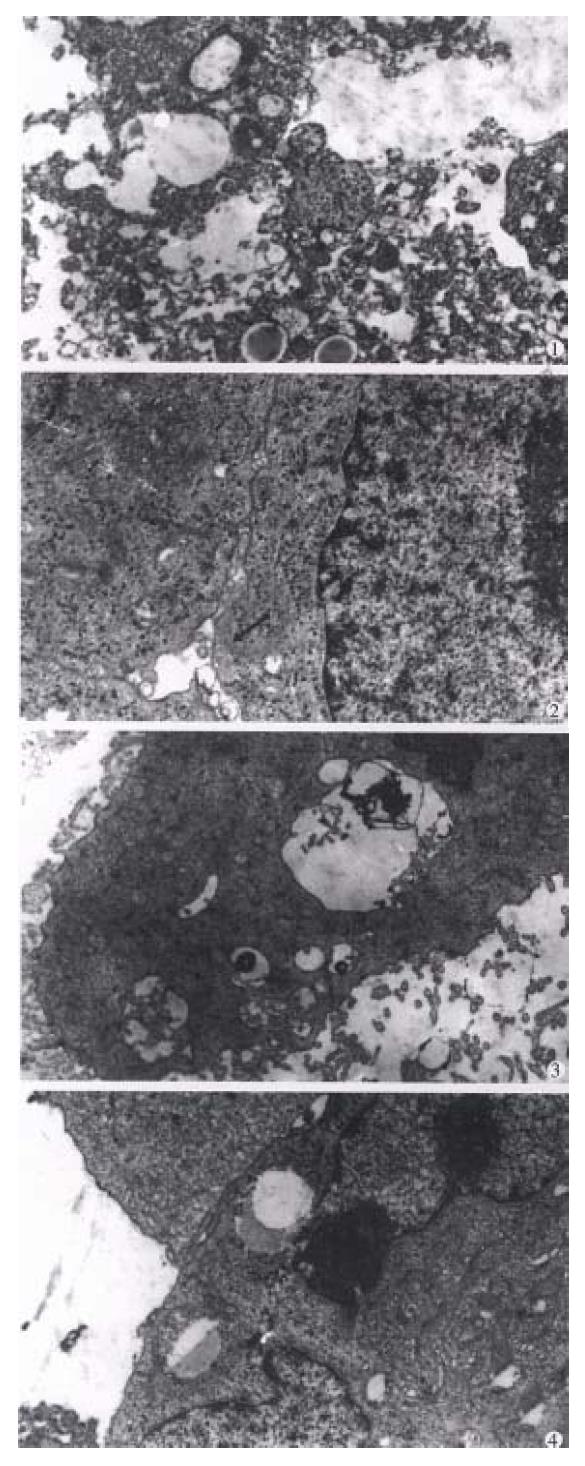
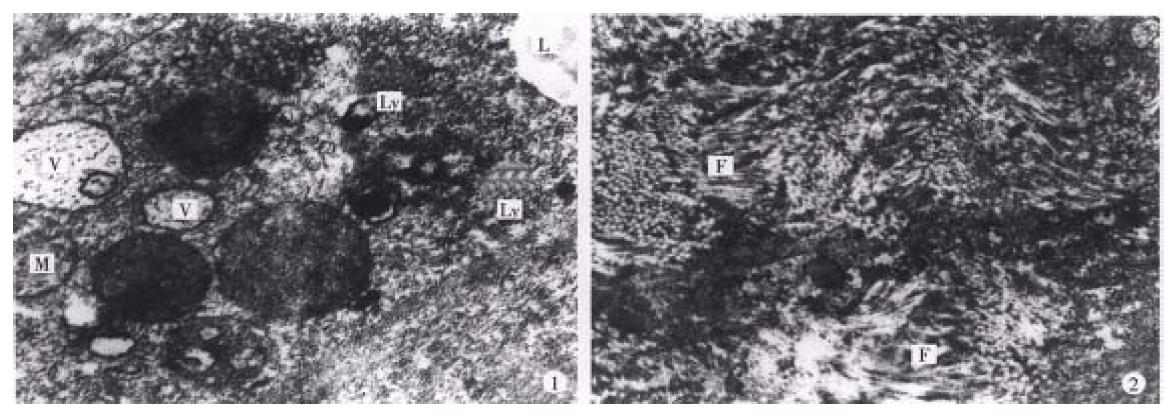
Figure 3 Results of intratumoral injection of 32P-GMS demonstrated by electron microscopy: ① Necrosed tumor cells ( × 5000 ).
② Formation of bile duct-like structure among tumor cells (solid arrow) ( × 8000). ③ Plenty of microvilli on the surface of tumor cell ( × 7000). ④ In control group, intratumoral injection of 32P-GMS showing heteromorphic tumor cell with cleavage of nucleus and scanty microvilli on surface ( × 7000).
Figure 4 Pig no.
10 by intrahepatic artery instillati on of 32P-GMS after 16wk, showing the glass fragments (solid a rrow shows) in the portal area, the distorted venule in the lower part of the picture is the artifact due to compression of interlobular venule by the glass microsphere during preparating slide. HE stain × 400
Figure 5 ① First week of internal irradiation irreg ularly distorted nuclei of hepatocytes, aggregation of heterochromatin at the pe riphery of nuclei, distension of perinuclei gap (solid arrow); decreased number of mitochondria in cytoplasm with heavy or light stained substance: dilatation of rough endoplasmic reticulum, depleted glycogen, and increased lysosomes and vacuoles.
× 10000 ② 16wk of internal irradiation: normal configuration of hepatocytes, plenty of plasmic mitochondria with normal cristae (curved arrow), no distention of the rough endoplasmic reticulum pool (small arrow), nor mal cellular conjunction (solid arrow). × 6000
Figure 6 ① Case 1.
Hepatic carcinoma, massive type, apparent decreased in size two months after 32P-GMS treatment (solid arrow). ② Case 2. Multiple metastatic hepatic tumor apparently decreased in size of left lobe focus after 32P-GMS treatment (solid arrow).
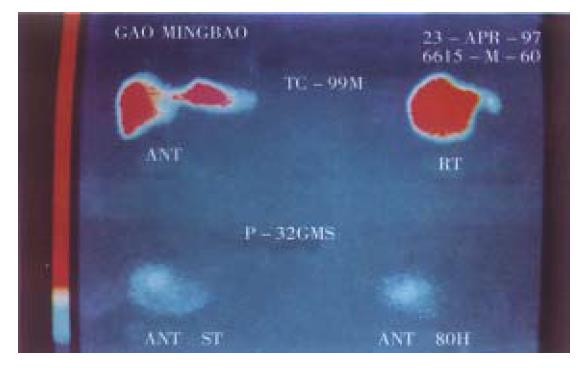
Figure 7 SPECT imaging before and after 32P-GMS internal irradiation in patients with relapsed HCC (interlobular) after operation.
Upper picture demonstrates interlobular colloidal image (anterio-posterior and light lateral position). Lower picture shows 80 h after 32P-GMS treatment, most of 32P-GMS cumulated in the foci, no extrahepatic organ imaging was found.
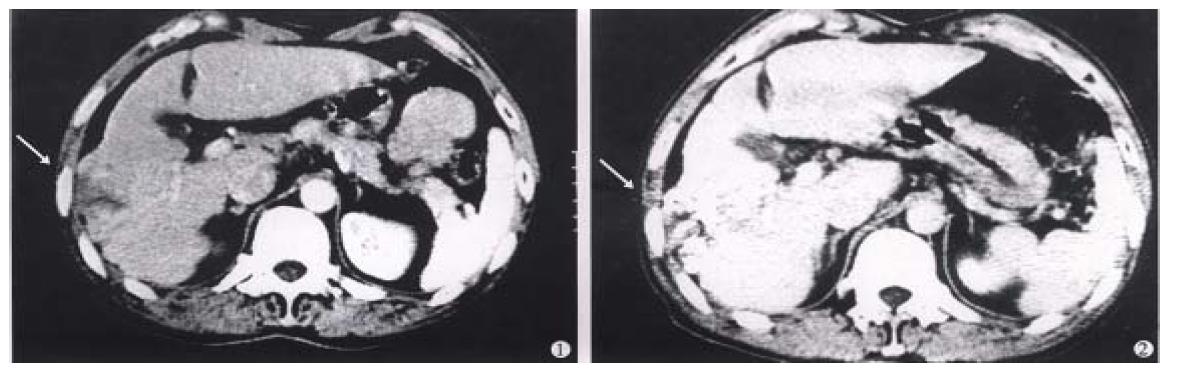
Figure 8 Male, aged 60, hospital no.
202929, clinical diagnosis: right lobe medium sized hepatic carcinoma (4 cm × 5 cm), treated by regimen A and B with an interval of 2 months. AFP from 103 μg/L restored to normal range, tumor size decreased > 50%, CT: 1, on pre-treatment showing a low density region in right lobe (arrow), 2, on post-treatment iodized oil distributed in fragments or encapsulated forms (arrow). Body weight gained more than 5kg and no subjective symptoms on 36 months follow-up.
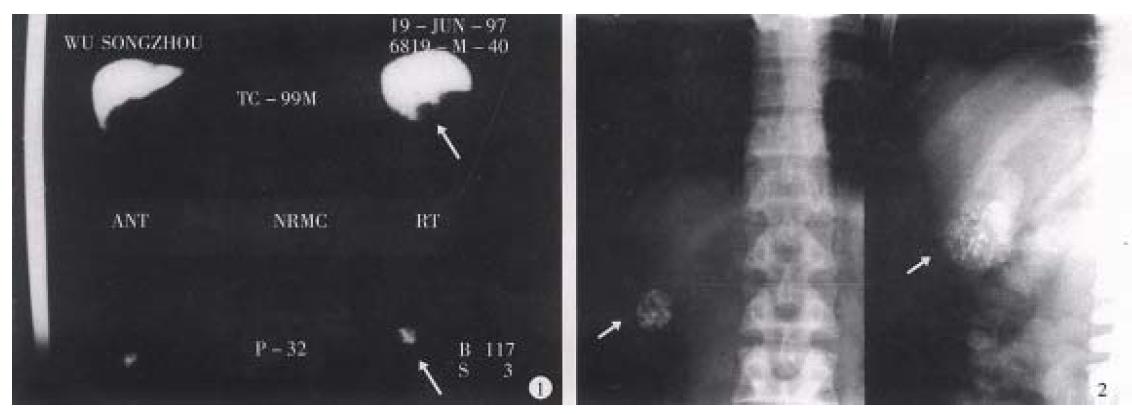
Figure 9 Male, aged 55, hospital no.
202295, clinical diagnosis: left lobe medium sized hepatic carcinoma (5 cm × 6 cm) near t he hepatic hilus, treated by TAE and regimen B, with interval of 2 months, and left hepatic lobectomy was performed 6 months later. The tumor (4 cm × 4 cm) was with hard consistency, and encapsulated fibrotic degeneration . Most of the cancer cells showed necrosis under light microscopy. Some cancer c ells in the cholecystic wall were alive (may be due to the blood supply from cho lecystic artery). The electron microscopy showed: 1, cancer cells degenerated and necrosed; in cytoplasm some vacuolized mitochondria (M), irregular sized vacuol es (V) and lysosome (Ly) and lipid droplet (L) were seen. The rest struct ures were not clear ( × 30000). 2, Prominent fibro-connective tissue hyperplasi a (F) in the tumor tissue ( × 10000) was found. Patient gained body weight and no subjective upset on follow up until 12 mos after operation.
Figure 10 Male, aged 41, hospital no.
207089, clinical diagnosis: uremia, right hepatic small carcinoma (4 cm × 3 cm), with A FP > 400 μg/L treated by regimen A for 2 courses with interval of 3 months, resulted in AFP restored to normal level and decreased tumor size over 50%. 1, Colloidal SPECT imaging showed the space occupying lesion in the right liver lobe (as shown by arrow). 2, Comparing the tumor size before and after treatment of plain film (as arrow shown), the patient died from renal failure 26 months after operation.
- Citation: Liu L, Jiang Z, Teng GJ, Song JZ, Zhang DS, Guo QM, Fang W, He SC, Guo JH. Clinical and experimental study on regional administration of phosphorus 32 glass microspheres in treating hepatic carcinoma. World J Gastroenterol 1999; 5(6): 492-505
- URL: https://www.wjgnet.com/1007-9327/full/v5/i6/492.htm
- DOI: https://dx.doi.org/10.3748/wjg.v5.i6.492