Copyright
©The Author(s) 2023.
World J Gastroenterol. Mar 21, 2023; 29(11): 1651-1668
Published online Mar 21, 2023. doi: 10.3748/wjg.v29.i11.1651
Published online Mar 21, 2023. doi: 10.3748/wjg.v29.i11.1651
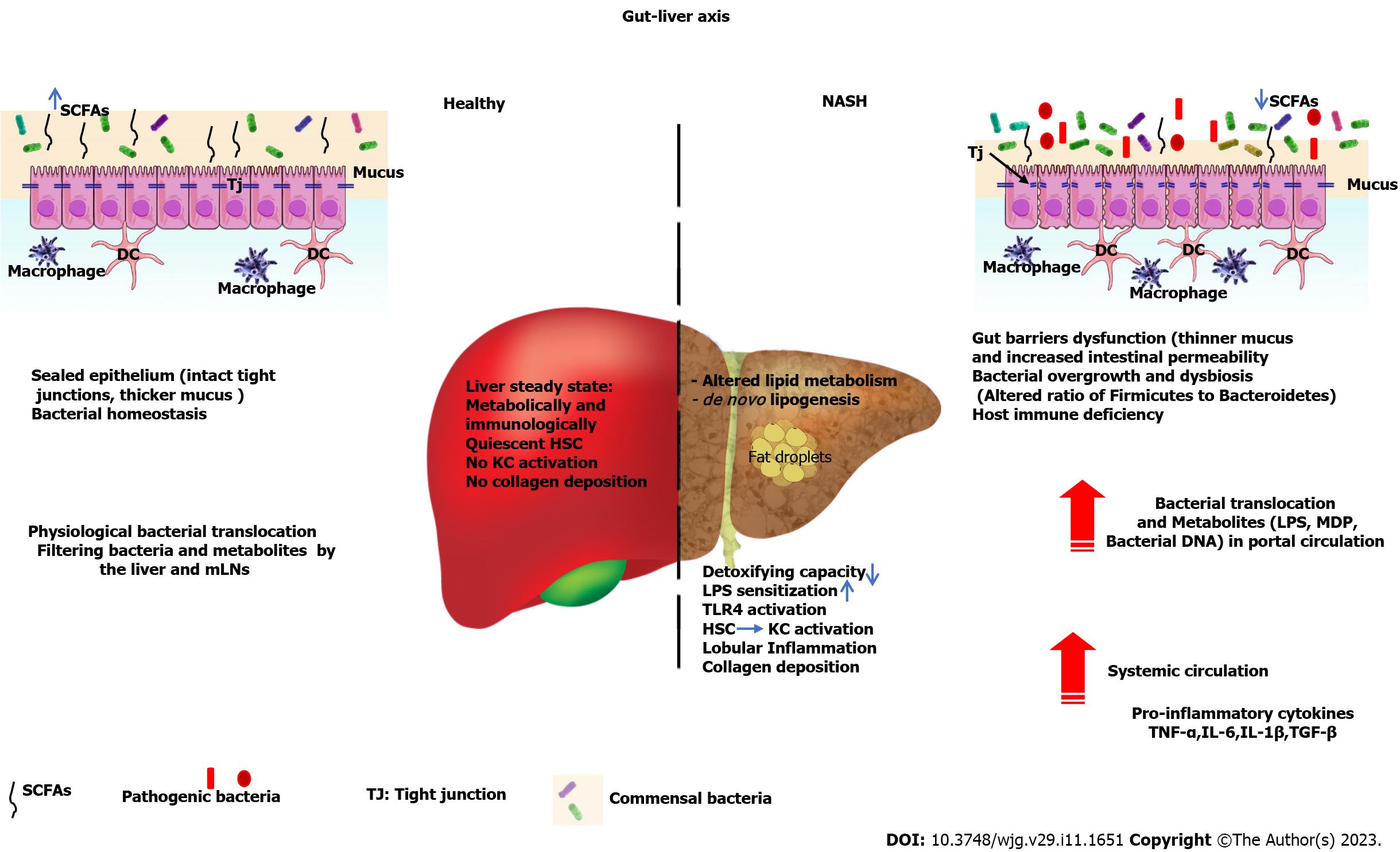
Figure 1 During development of nonalcoholic steatohepatitis, several immunological and metabolic pathways intersect, thus promoting progression of liver injury and nonalcoholic steatohepatitis.
In healthy conditions, gut-liver axis homeostasis is guaranteed by intact intestinal epithelium barriers and proper liver-host immune functions that limit the translocation of bacteria and their metabolites. In nonalcoholic steatohepatitis (NASH), on the one hand, the intestinal barriers are disrupted (thin mucus layer, decreased expression of tight junction proteins, altered ratio of Firmicutes to Bacteroidetes, dysbiosis, decreased short-chain fatty acids that result in increased leakage of bacteria and their metabolites (Lipopolysaccharide, MDP, flagellin, bacterial DNA) into the portal vein and systemic circulation, consequently stimulating the production of inflammatory cytokines in the systemic circulation. On the other hand, liver function is compromised because of the accumulation of fat, altered lipid metabolism, and increased microbial burden, which in turn elicits hepatic inflammation, hepatic stellate cell activation and collagen deposition, Kupffer cell activation, and triggering of the toll-like receptor 4 signaling pathway, which altogether contribute to the development of NASH. Tj: Tight junction; SCFAs: Short-chain fatty acids; KC: Kupffer cell; HSC: Hepatic stellate cell; LPS: Lipopolysaccharide; mLN: Mesenteric lymph nodes; TLR4: Toll-like receptor 4; TNF-α: Tumor necrosis factor-α; IL-6: Interleukin-6; TGF-β: Transforming growth factor-β; IL-1β: Interleukin-1β.
- Citation: Kirundi J, Moghadamrad S, Urbaniak C. Microbiome-liver crosstalk: A multihit therapeutic target for liver disease. World J Gastroenterol 2023; 29(11): 1651-1668
- URL: https://www.wjgnet.com/1007-9327/full/v29/i11/1651.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i11.1651