Copyright
©The Author(s) 2021.
World J Gastroenterol. Aug 14, 2021; 27(30): 5019-5036
Published online Aug 14, 2021. doi: 10.3748/wjg.v27.i30.5019
Published online Aug 14, 2021. doi: 10.3748/wjg.v27.i30.5019
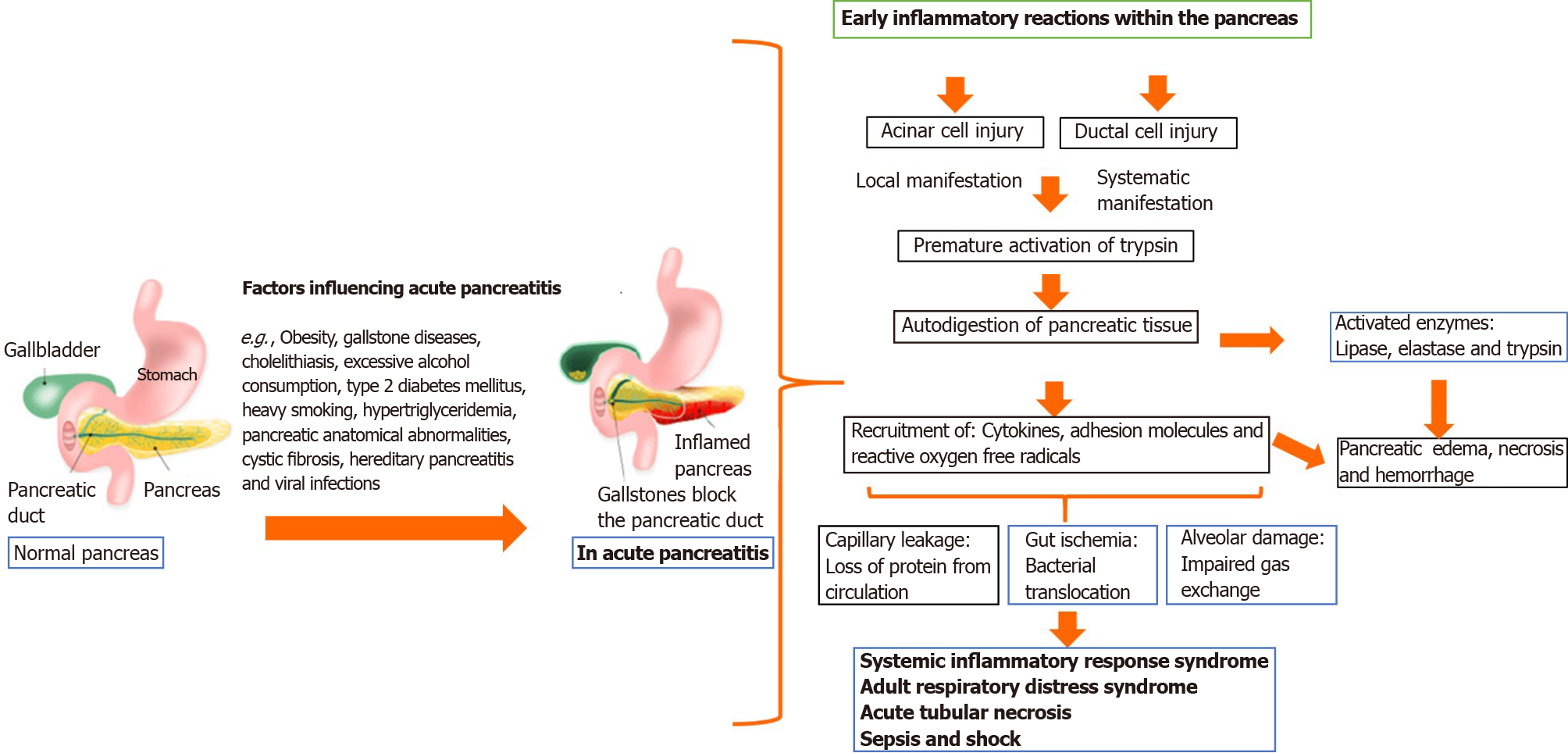
Figure 1 Pathophysiology of acute pancreatitis.
Damage in the pancreas' acinar cell causes trypsin activation following cell membrane trafficking impairment, with subsequent activation of the zymogen cascade by trypsin. Attraction and activation of leukocytes occur with the release of many proinflammatory and anti-inflammatory cytokines, as well as chemokines. An overt and sustained activation of proinflammatory mediators leads to systemic inflammatory response syndrome (SIRS), which may further proceed to multiorgan failure, pancreatic necrosis and sepsis with late complications of acute pancreatitis.
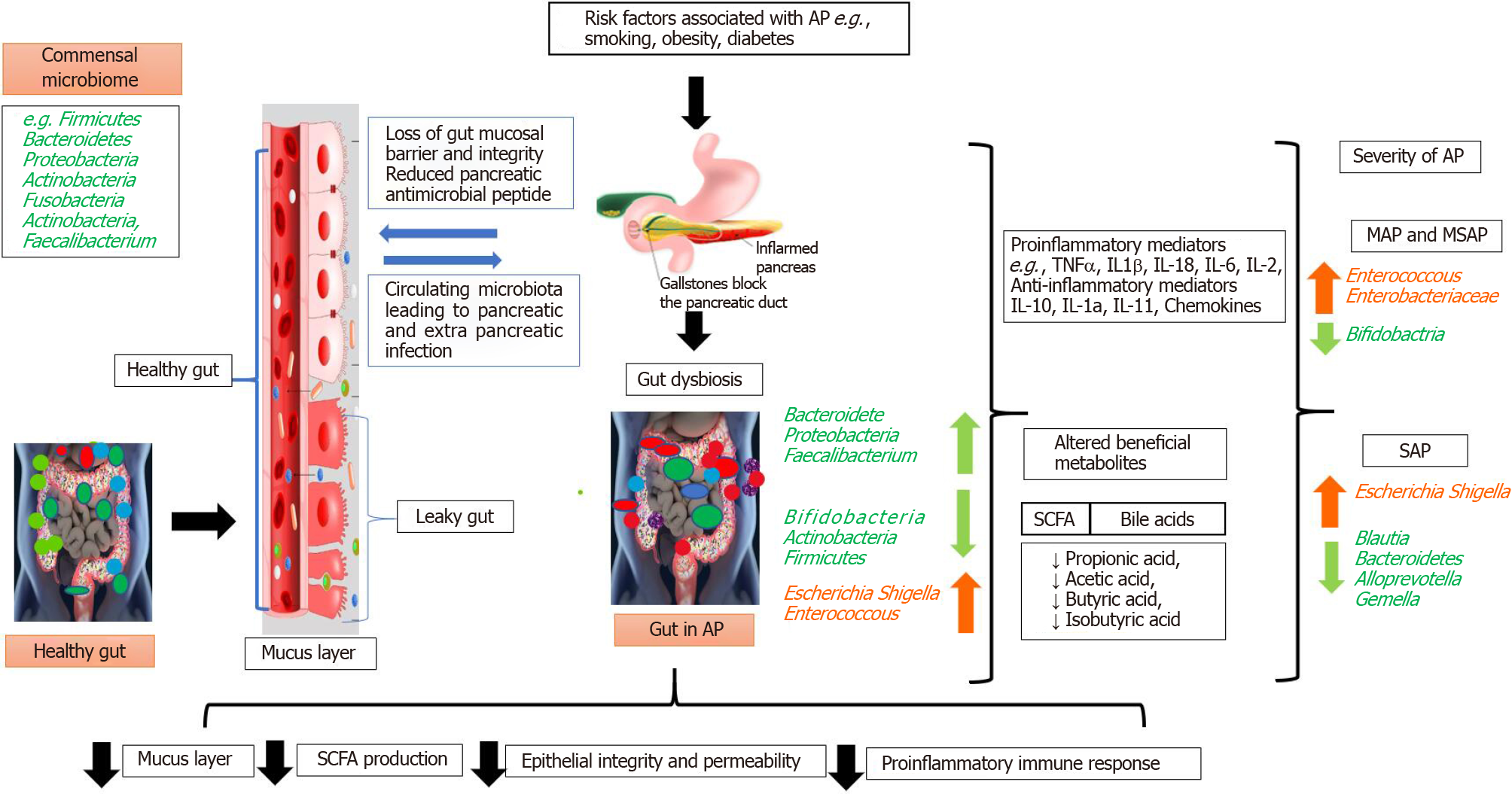
Figure 2 Role of the gut microbiota in inflammation of the pancreas and acute pancreatitis.
Breakdown of the relationship between physiologic and pathogenic bacteria, the immune system, and the intestinal epithelial barrier leads to gut dysbiosis. Inflammation and gut dysbiosis causes the translocation of microbes to the pancreas. The translocation of bacteria results in pancreatic inflammation due to toxin diffusion and complications like fibrosis, digestive and absorption disorders, diabetes, and other metabolic disorders. AP: Acute pancreatitis; MAP: Mild acute pancreatitis; MSAP: Moderate severe acute pancreatitis; TNF: Tumor necrosis factor; IL: Interleukin; SAP: Severe acute pancreatitis; SCFA: Short-chain fatty acids.
- Citation: Patel BK, Patel KH, Bhatia M, Iyer SG, Madhavan K, Moochhala SM. Gut microbiome in acute pancreatitis: A review based on current literature. World J Gastroenterol 2021; 27(30): 5019-5036
- URL: https://www.wjgnet.com/1007-9327/full/v27/i30/5019.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i30.5019