Copyright
©The Author(s) 2020.
World J Gastroenterol. Nov 14, 2020; 26(42): 6582-6598
Published online Nov 14, 2020. doi: 10.3748/wjg.v26.i42.6582
Published online Nov 14, 2020. doi: 10.3748/wjg.v26.i42.6582
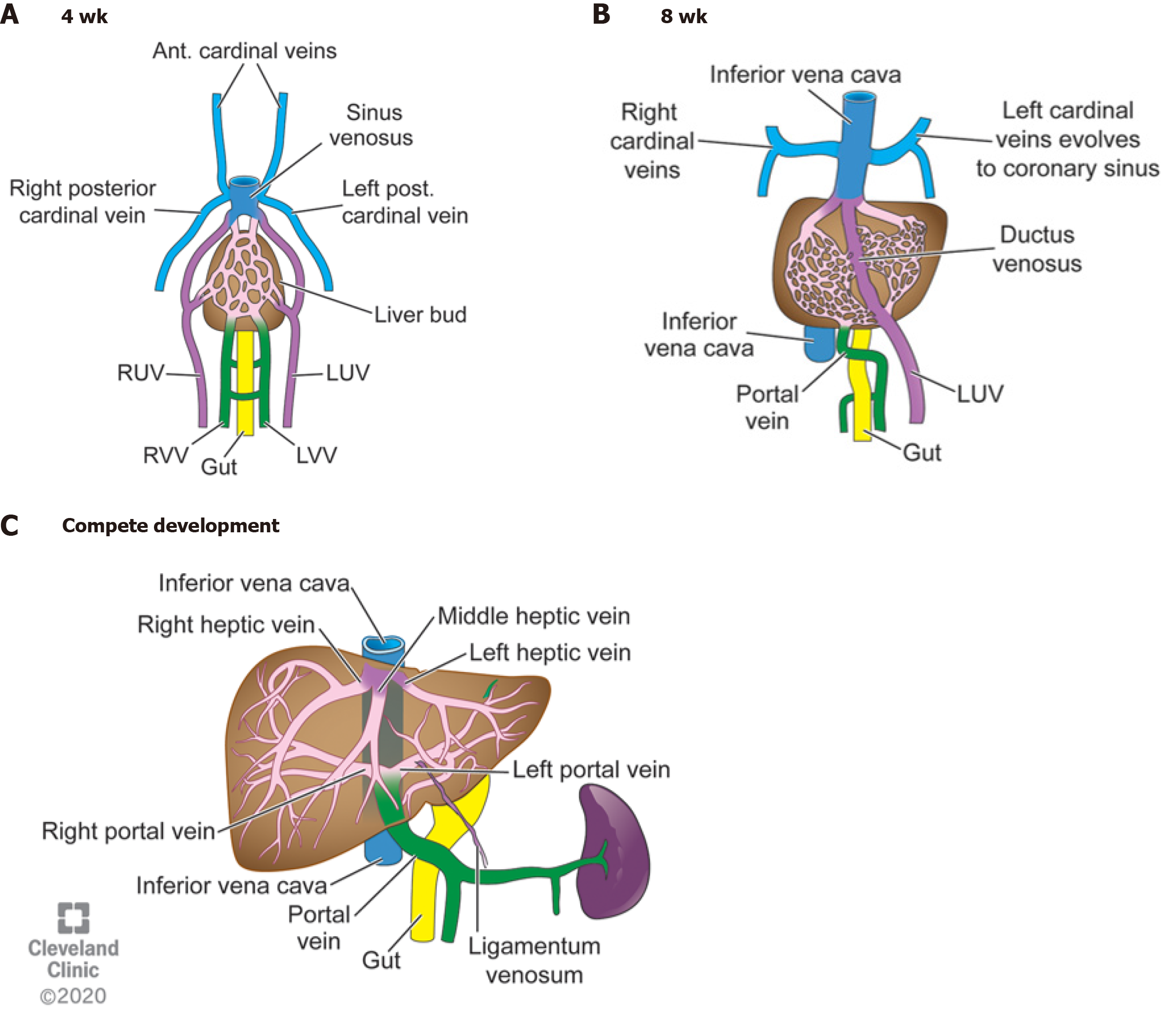
Figure 1 Four weeks gestation, eight weeks gestation, and the mature liver vasculature after birth.
A: Right and left umbilical, cardinal, and vitelline veins making up the primitive vasculature to the developing liver bud. Cardinal and umbilical veins converge on top of the liver to form the sinus venosus. The vitelline veins return blood from the developing gut; B: Posterior cardinal veins coalesce to form the upper part of the inferior vena cava. The right umbilical vein involutes and left umbilical vein makes up the ductus venosus (DV). The intrahepatic vessels start to form mature hepatic veins. The vitelline veins start to mature into the portal venous system; C: The DV collapses at birth after the umbilical cord is cut and becomes the ligamentum venosum. The portal veins and hepatic veins are mature. RUV: Right umbilical vein; LUV: Left umbilical vein; RRV: Right vitelline vein; LVV: Left vitelline vein; IVC: Inferior vena cava. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography ©2020. All rights reserved.
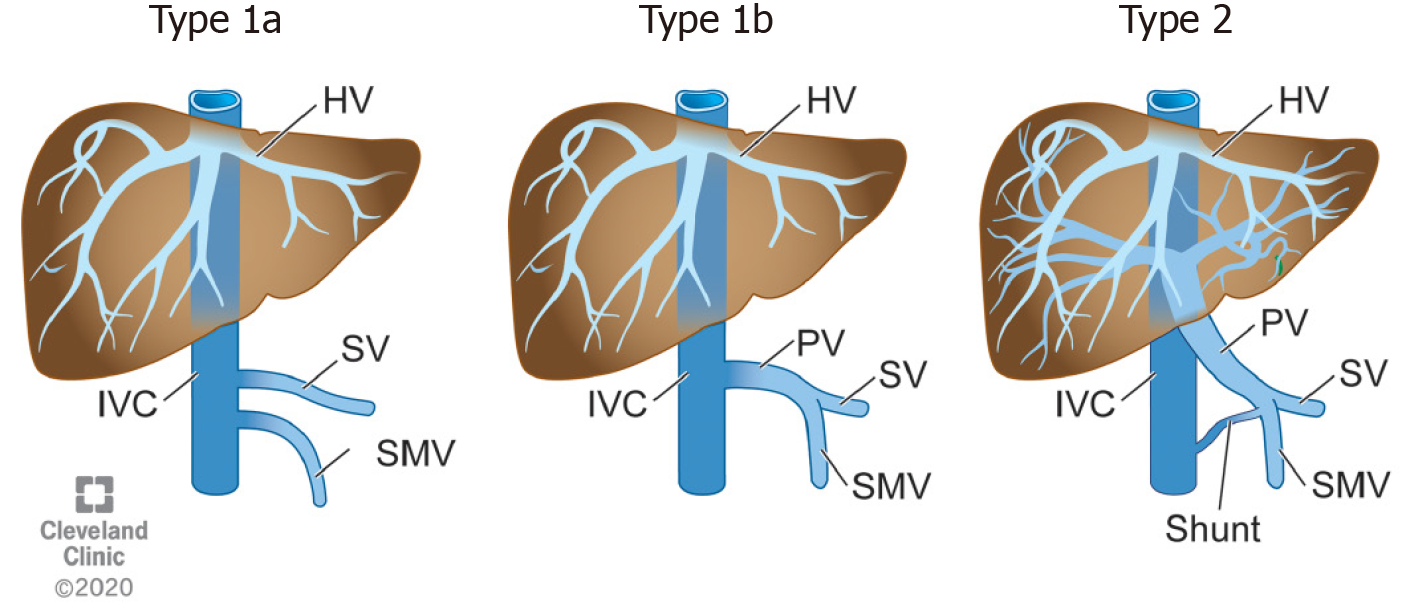
Figure 2 Morgan and Superina congenital extrahepatic portosystemic shunts.
Refer to Table 1 for descriptions. HV: Hepatic vein; SV: Splenic vein; SMV: Superior mesenteric vein; IVC: Inferior vena cava; PV: Portal vein. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography ©2020. All rights reserved.
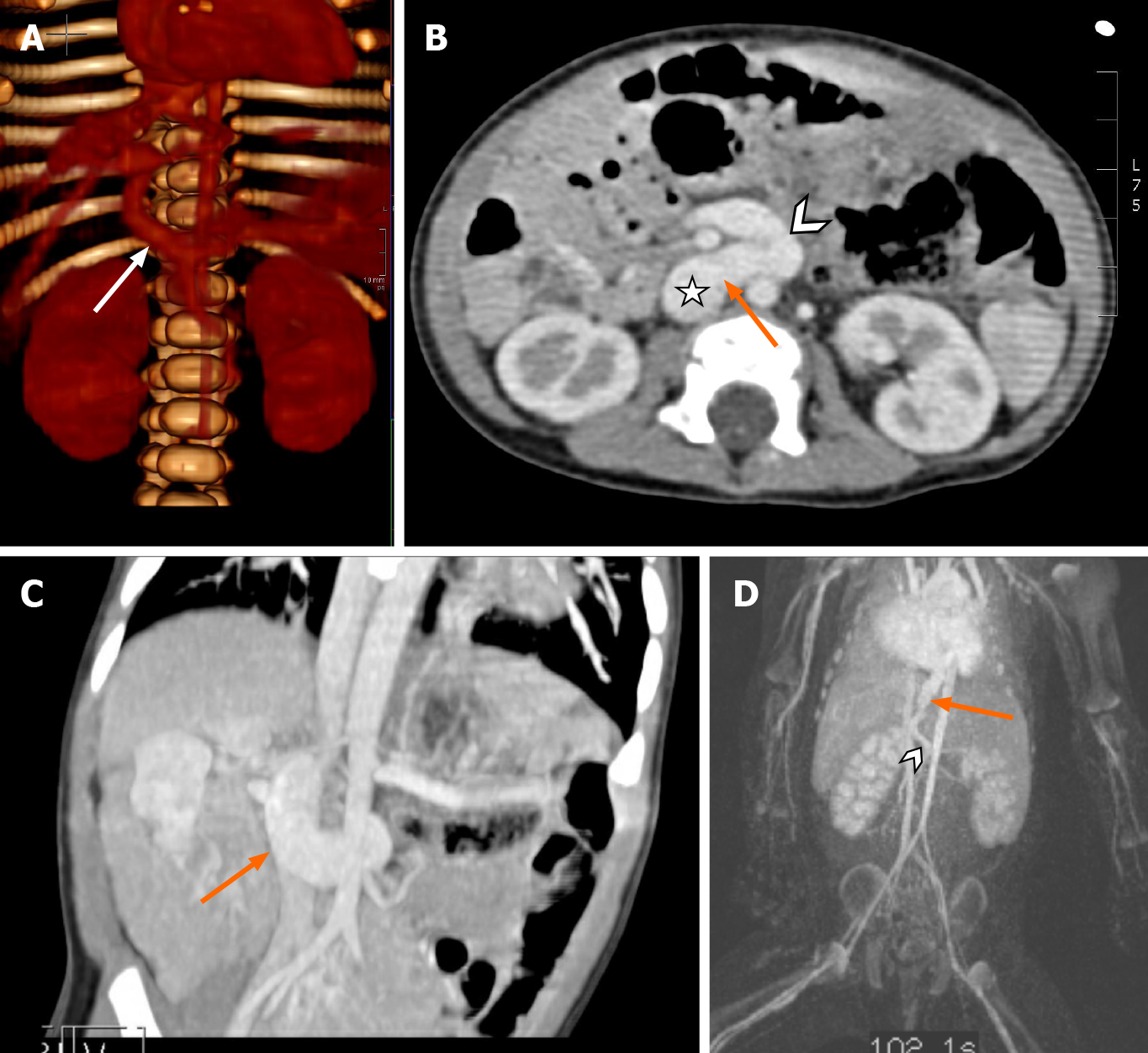
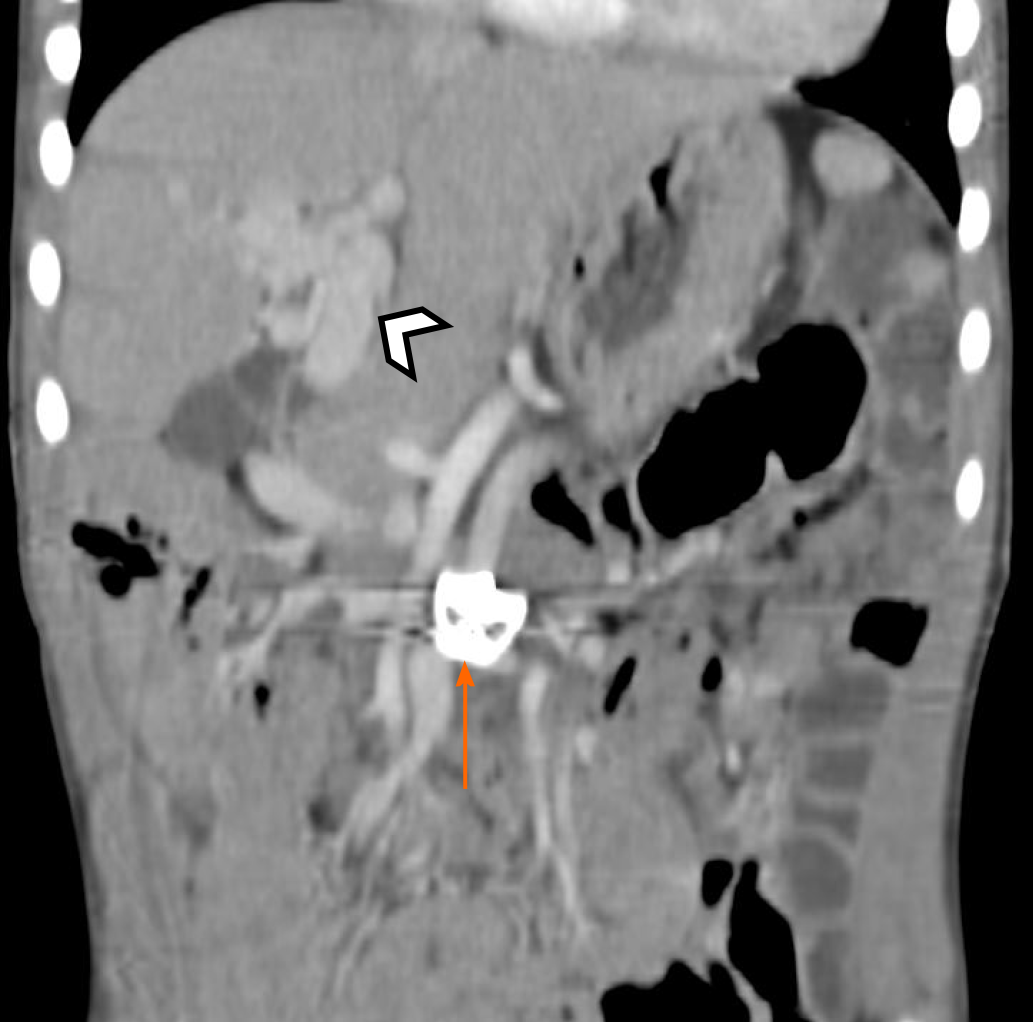
Figure 3 Two-year-old with Abernethy Malformation Type 1b (arrow).
A connection from superior mesenteric vein (chevron) to the inferior vena cava (star).
Figure 4 Examples of congenital extrahepatic portosystemic shunts.
A: Nineteen-month-old with congenital extrahepatic porto-systemic shunts (CEPSS) Type II. Connection (arrow) of portal vein to inferior vena cava (IVC). Reconstruction 3D rendering of a computed tomography scan; B and C: One year old with a history of heterotaxia, intestinal malrotation, pulmonary arteriovenous malformations and CEPSS Type II (orange arrow), portal vein (chevron) to IVC (star); D: Type II extrahepatic shunt superior mesenteric vein (chevron) and shunt (arrow) draining directly into the right atrium.
Figure 5 Computed tomography abdomen showing congenital cavernous malformation of the portal vein (arrow).
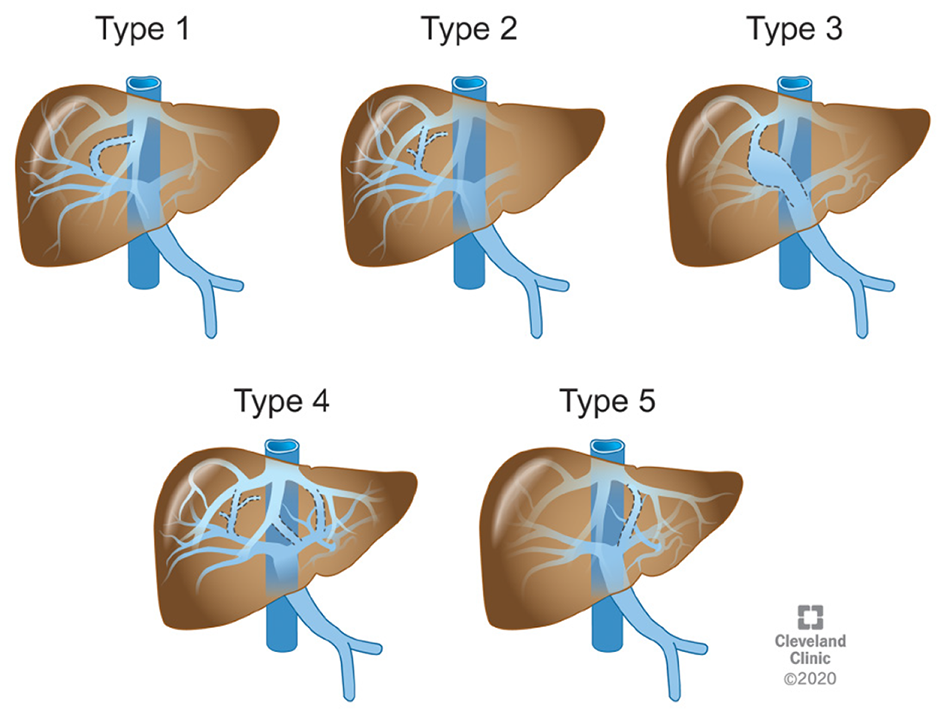
Figure 6 Park’s classifications of congenital intrahepatic portosystemic shunts.
Refer to Table 2 for description. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography ©2020. All rights reserved.
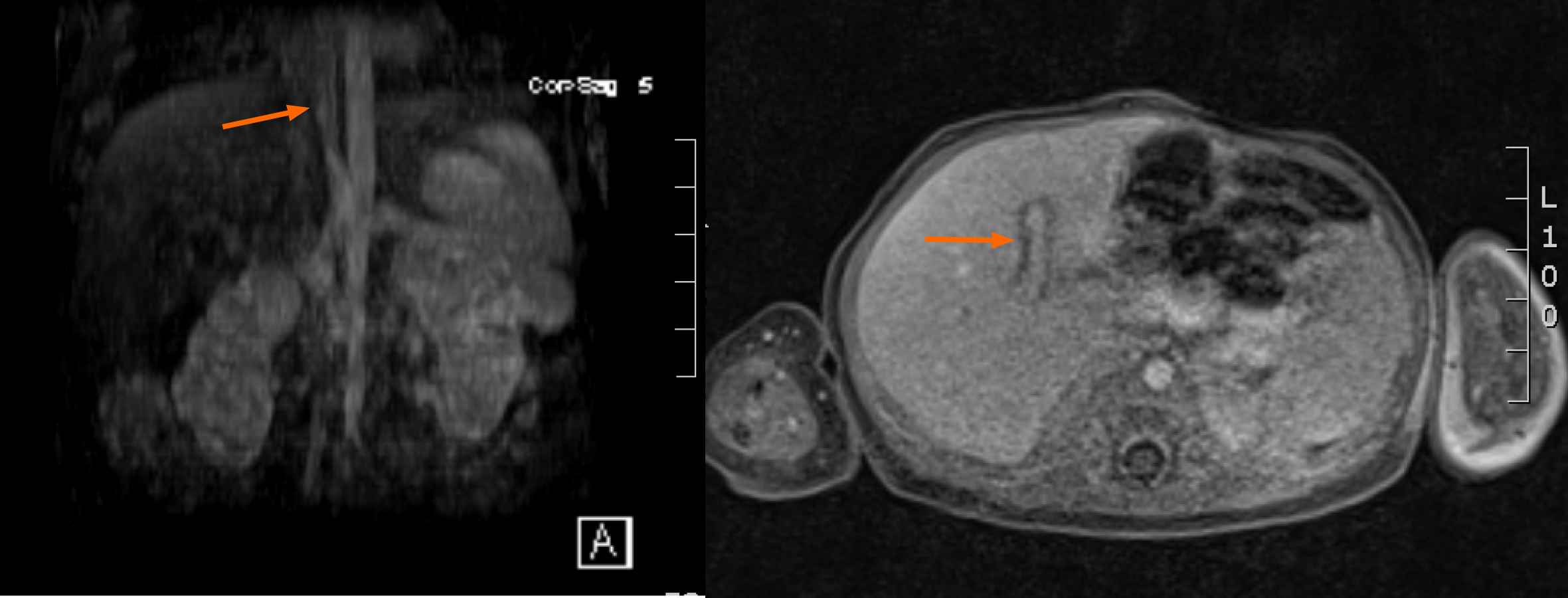
Figure 7 Intrahepatic shunt, main portal vein to the left hepatic vein (arrow).
Figure 8 Intravascular closure.
A: Angiography showing a large congenital extrahepatic porto-systemic shunts (CEPSS) Type II (arrow); B: Balloon occlusion of the shunt revealing multiple large intrahepatic collateral vessels (arrows) (CIPSS Type IV); C: Anteroposterior; D: Lateral views of repeat angiography several months post partial occlusion of shunt showing improvement in portal venous flow after partial occlusion with better visualization of the right portal vein (chevron). Occlusion device not seen.
Figure 9 Four-year-old boy with heterotaxia and congenital extrahepatic porto-systemic shunts Type II two years post device closure (arrow).
He subsequently developed a cavernous transformation of the portal vein (chevron).
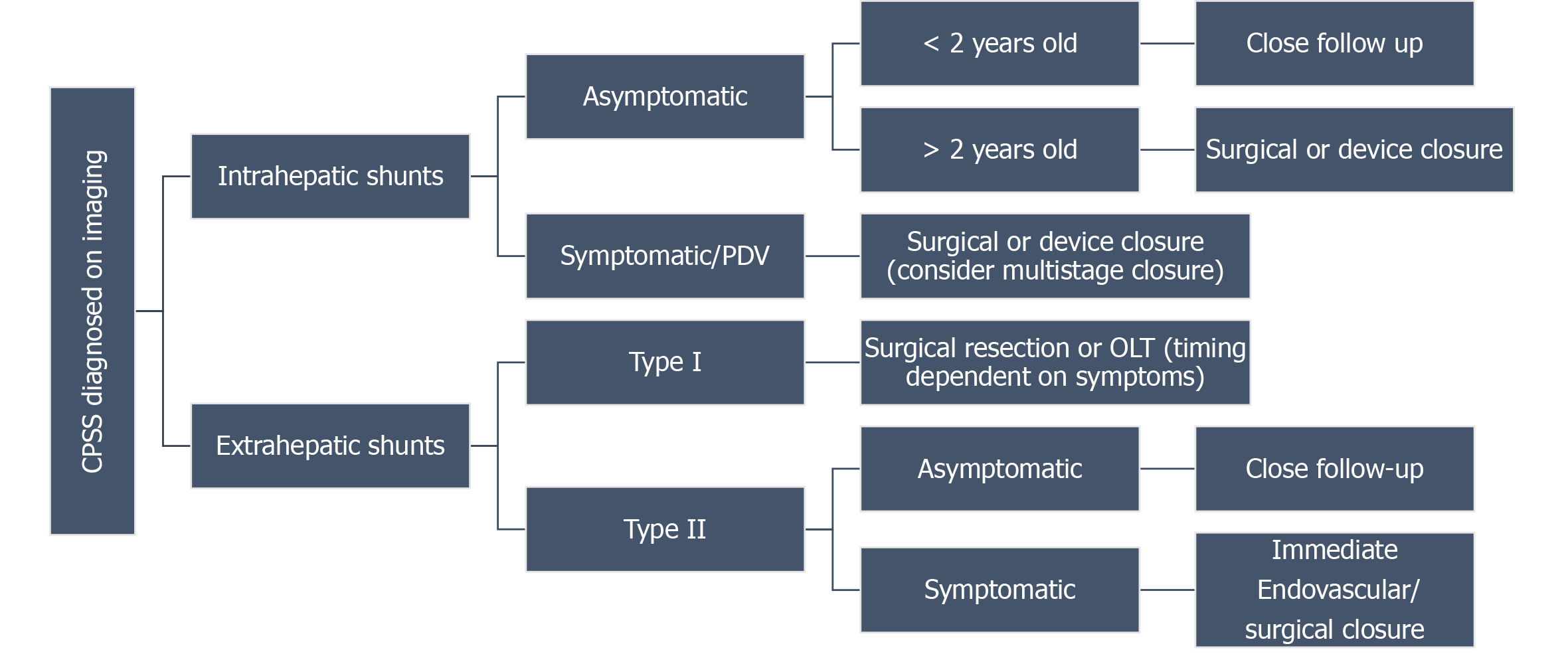
Figure 10 Congenital portosystemic shunts treatment algorithm.
OLT: Orthotopic liver transplant; CPSS: Congenital portosystemic shunts.
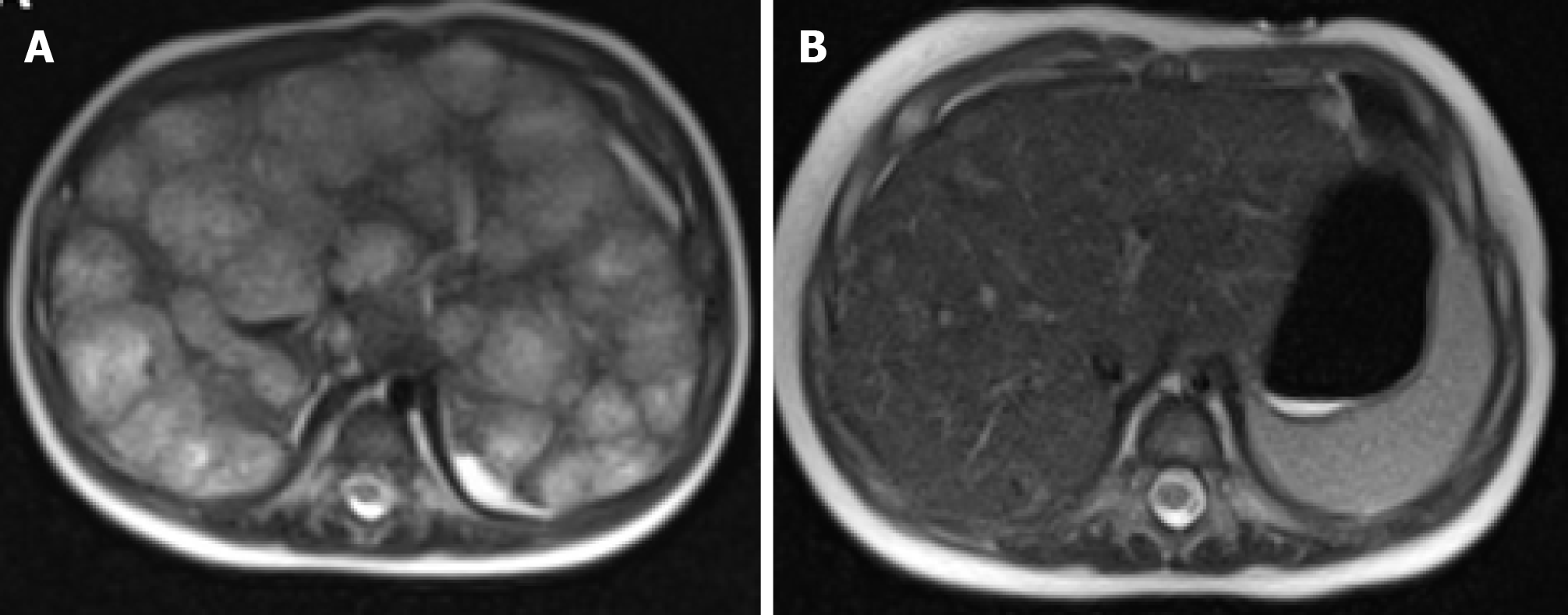
Figure 11 Magnetic resonance imaging results.
A: Magnetic resonance imaging (MRI) of liver in a 4-month-old at the time of the diagnosis, axial T2-weighted (HASTE) image showing multiple nodular hyperintense lesions with centripetal fill-in on the delayed phase; B: MRI of the liver 3 mo after starting atenolol treatment, subsequent axial T2-weighted image showing interval decrease in size of enhancing lesions and improving hepatomegaly.
- Citation: Schmalz MJ, Radhakrishnan K. Vascular anomalies associated with hepatic shunting. World J Gastroenterol 2020; 26(42): 6582-6598
- URL: https://www.wjgnet.com/1007-9327/full/v26/i42/6582.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i42.6582