Copyright
©The Author(s) 2020.
World J Gastroenterol. Jun 28, 2020; 26(24): 3458-3471
Published online Jun 28, 2020. doi: 10.3748/wjg.v26.i24.3458
Published online Jun 28, 2020. doi: 10.3748/wjg.v26.i24.3458
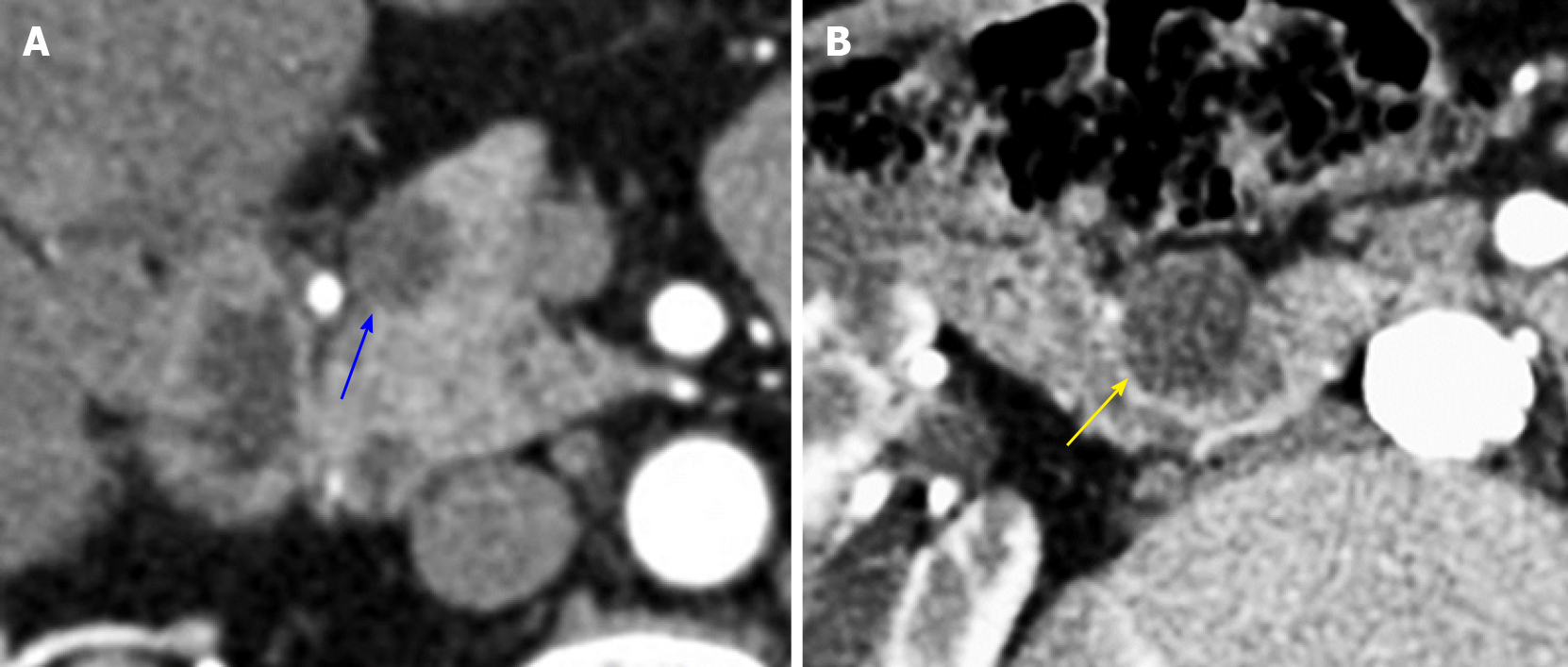
Figure 1 Low and high grade intraductal papillary mucinous neoplasms on computed tomography.
A: Axial post contrast arterial phase computed tomography (CT) image magnified at the pancreatic head shows a hypodense well defined pathology proven intraductal papillary mucinous neoplasm (IPMN) with low grade dysplasia (blue arrow). Arterial gray level co-occurrence matrix (GLCM) entropy was 9.31; B: Axial post contrast arterial phase CT image in a different patient with pathology proven IPMN with high grade dysplasia (yellow arrow). Arterial GLCM entropy was 11.52. These lesions could be described similarly using qualitative terminology, however in this study, quantitative radiomics features improved prediction of malignant pathology compared to conventional measures alone.
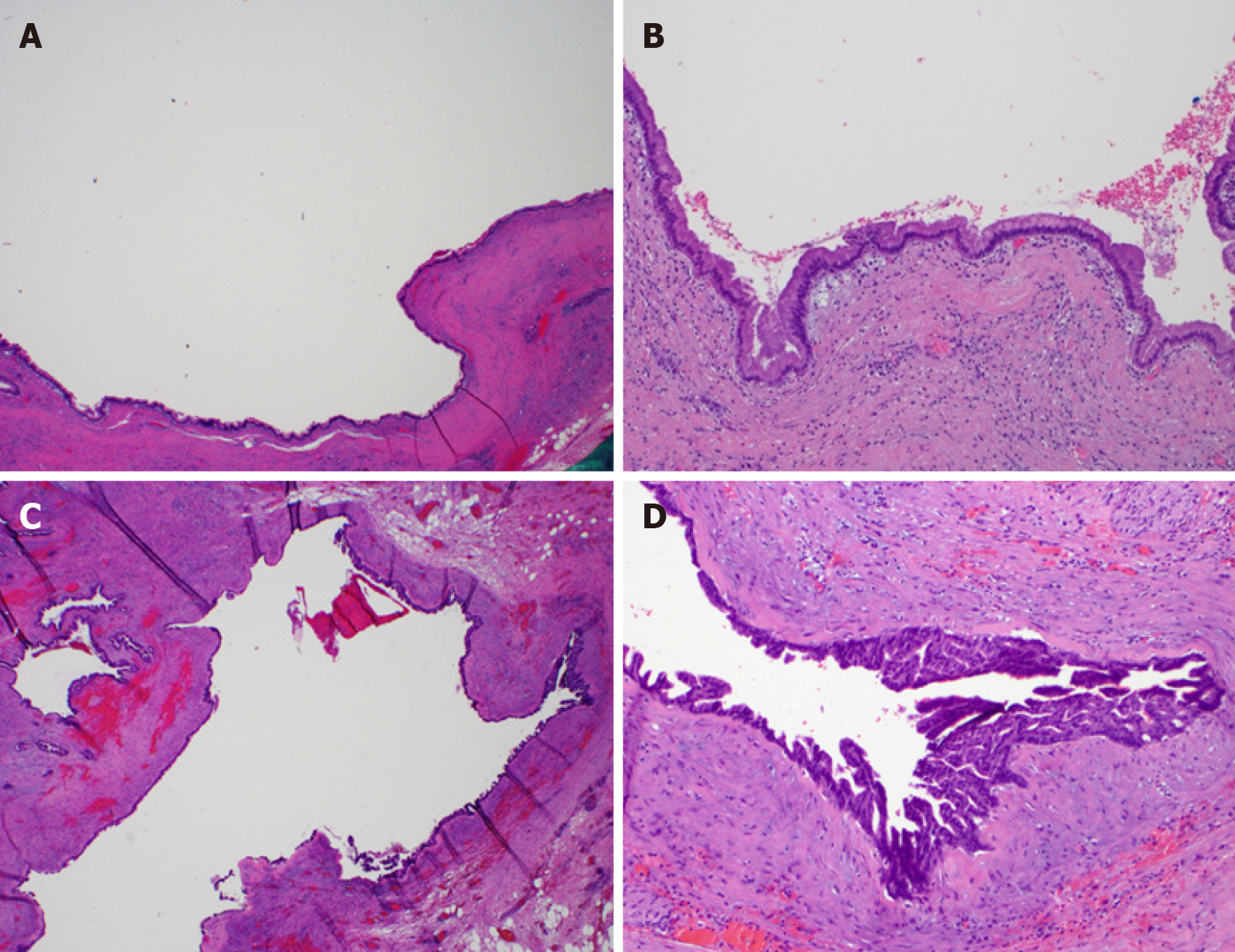
Figure 2 Histology of low grade and high grade intraductal papillary mucinous neoplasm lesions are shown.
A: Low grade intraductal papillary mucinous neoplasm (IPMN) hematoxylin and eosin stain (HE) at 20 × magnification; B: Low grade IPMN HE at 100 × magnification. Low grade IPMN is represented by a single layer of mucinous epithelium containing columnar, palisading nuclei and abundant mucinous cytoplasm, with low nuclei/cytoplasmic ratio, minimal cytologic atypia and an absence of obvious mitosis; C: High grade IPMN HE at 20 × magnification; D: High grade IPMN HE at 100 × magnification. In contrast to low grade, high grade IPMN frequently demonstrates decreased cytoplasmic mucin contents, loss of nuclear polarity with nuclear overlapping, higher nuclei/cytoplasmic ratio, significant cytologic atypia and easily identifiable mitosis.
- Citation: Polk SL, Choi JW, McGettigan MJ, Rose T, Ahmed A, Kim J, Jiang K, Balagurunathan Y, Qi J, Farah PT, Rathi A, Permuth JB, Jeong D. Multiphase computed tomography radiomics of pancreatic intraductal papillary mucinous neoplasms to predict malignancy. World J Gastroenterol 2020; 26(24): 3458-3471
- URL: https://www.wjgnet.com/1007-9327/full/v26/i24/3458.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i24.3458