Copyright
©The Author(s) 2020.
World J Gastroenterol. May 7, 2020; 26(17): 1993-2011
Published online May 7, 2020. doi: 10.3748/wjg.v26.i17.1993
Published online May 7, 2020. doi: 10.3748/wjg.v26.i17.1993
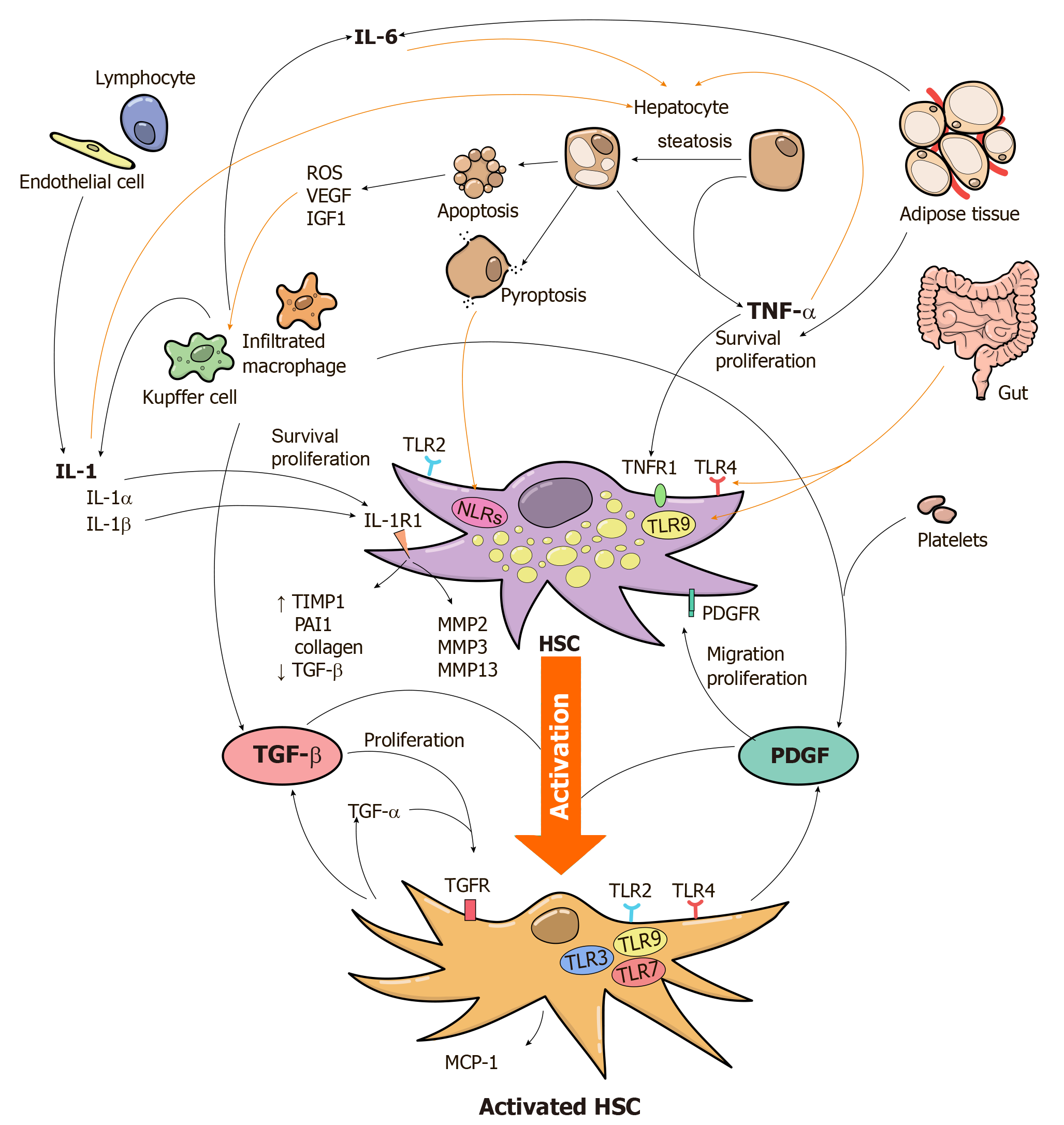
Figure 1 Innate immune pathways and mediators involved in the development of liver fibrosis during non-alcoholic fatty liver disease.
Activation of the HSCs is the major event during the development of liver fibrosis. Various mediators released from parenchymal as well as non-parenchymal cells of the liver, as well as from metabolic organs (adipose tissue, gut) can promote HSCs activation. TGF-β and PDGF, mainly produced by liver macrophages, have a central role in hepatic fibrogenesis. HSCs start to produce TGF-β, PDGF and MCP-1 after their activation. Autocrine production of TGF-β and PDGF by activated HSCs induces their further proliferation. Hepatic macrophages, lymphocytes and endothelial cells secrete IL-1α and IL-1β. These molecules participate in the initial extracellular matrix degradation by induction of MMP2, MMP3 and MMP13 expression by HSCs, while are also implicated in HSC survival and proliferation. IL-1β, in particular, induces the expression of TIMP-1, PAI-1 and collagen. In addition, pro-inflammatory cytokines such as IL-1β, IL-6 and TNF-α can induce lipid accumulation in hepatocytes and in turn cause hepatocyte injury and inflammation. Apoptotic hepatocytes secrete reactive oxygen species, vascular endothelial growth factor and IGF1, which can activate hepatic macrophages. Pyroptosis can also contribute to the development of fibrosis via activation of NLRs in HSCs. Of note, TLR2, TLR4 and TLR9, expressed by liver macrophages and HSCs are the key Toll-like receptors in the pathophysiology of NASH and metabolism-related liver fibrosis by provoking the expression of pro-inflammatory and pro-fibrotic cytokines by these cells.
- Citation: Katsarou A, Moustakas II, Pyrina I, Lembessis P, Koutsilieris M, Chatzigeorgiou A. Metabolic inflammation as an instigator of fibrosis during non-alcoholic fatty liver disease. World J Gastroenterol 2020; 26(17): 1993-2011
- URL: https://www.wjgnet.com/1007-9327/full/v26/i17/1993.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i17.1993