Copyright
©The Author(s) 2018.
World J Gastroenterol. Sep 21, 2018; 24(35): 3980-3999
Published online Sep 21, 2018. doi: 10.3748/wjg.v24.i35.3980
Published online Sep 21, 2018. doi: 10.3748/wjg.v24.i35.3980
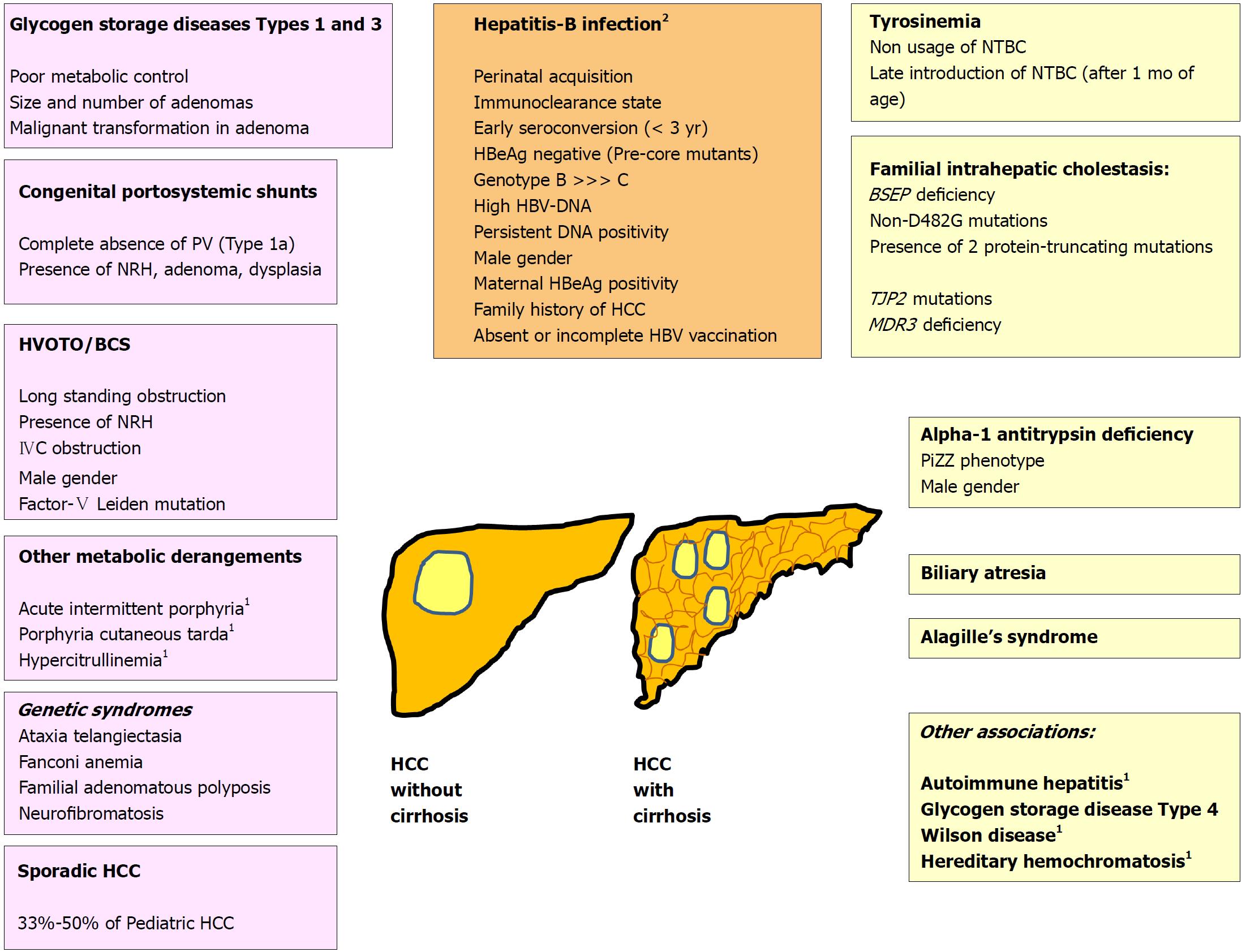
Figure 1 Risk factors for pediatric hepatocellular carcinoma.
1Conditions cause HCC in adults, and very rarely in children; 2HBV related HCC may occur in presence or absence of cirrhosis. BCS: Budd-Chiari syndrome; HCC: Hepatocellular carcinoma; HVOTO: Hepatic venous outflow tract obstruction; IVC: Inferior vena cava; NRH: Nodular regenerative hyperplasia; BSEP: Bile salt export pump; HCC: Hepatocellular carcinoma; MDR3: Multidrug resistance protein-3; NTBC: [2-(2-nitro-4-trifluoromethylbenzoyl)-1,3-cyclohexanedione (Nitisinone); PiZZ: Homozygous PiZ phenotype of alpha-1 antitrypsin; PV: Portal vein, TJP: Tight junction protein.
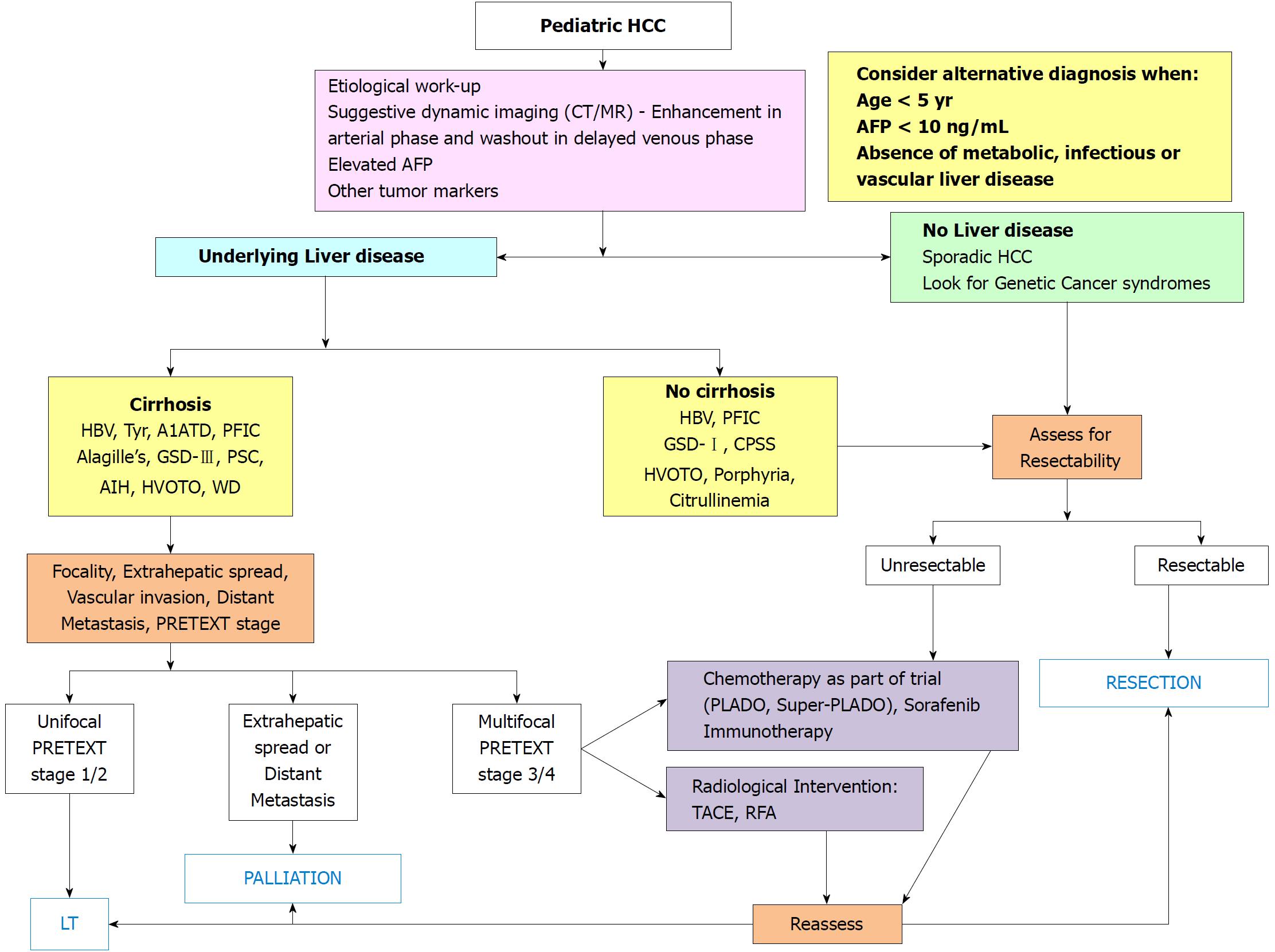
Figure 2 Algorithmic management of pediatric hepatocellular carcinoma.
A1ATD: Alpha-1 antitrypsin deficiency; AFP: Alpha-fetoprotein; AIH: Autoimmune hepatitis; CPSS: Congenital portosystemic shunt; GSD: Glycogen storage disorder; HBV: Hepatitis-B virus; HVOTO: Hepatic venous outflow tract obstruction; LT: Liver transplantation; PFIC: Progressive familial intrahepatic cholestasis; PLADO: Cisplatin + Doxorubicin; PRETEXT: Pretreatment tumor extent evaluation; PSC: Primary sclerosing cholangitis; RFA: Radiofrequency ablation; Super-PLADO: Cisplatin, Carboplatin and Doxorubicin; TACE: Transarterial chemo-embolization; Tyr: Tyrosinemia; WD: Wilson disease.
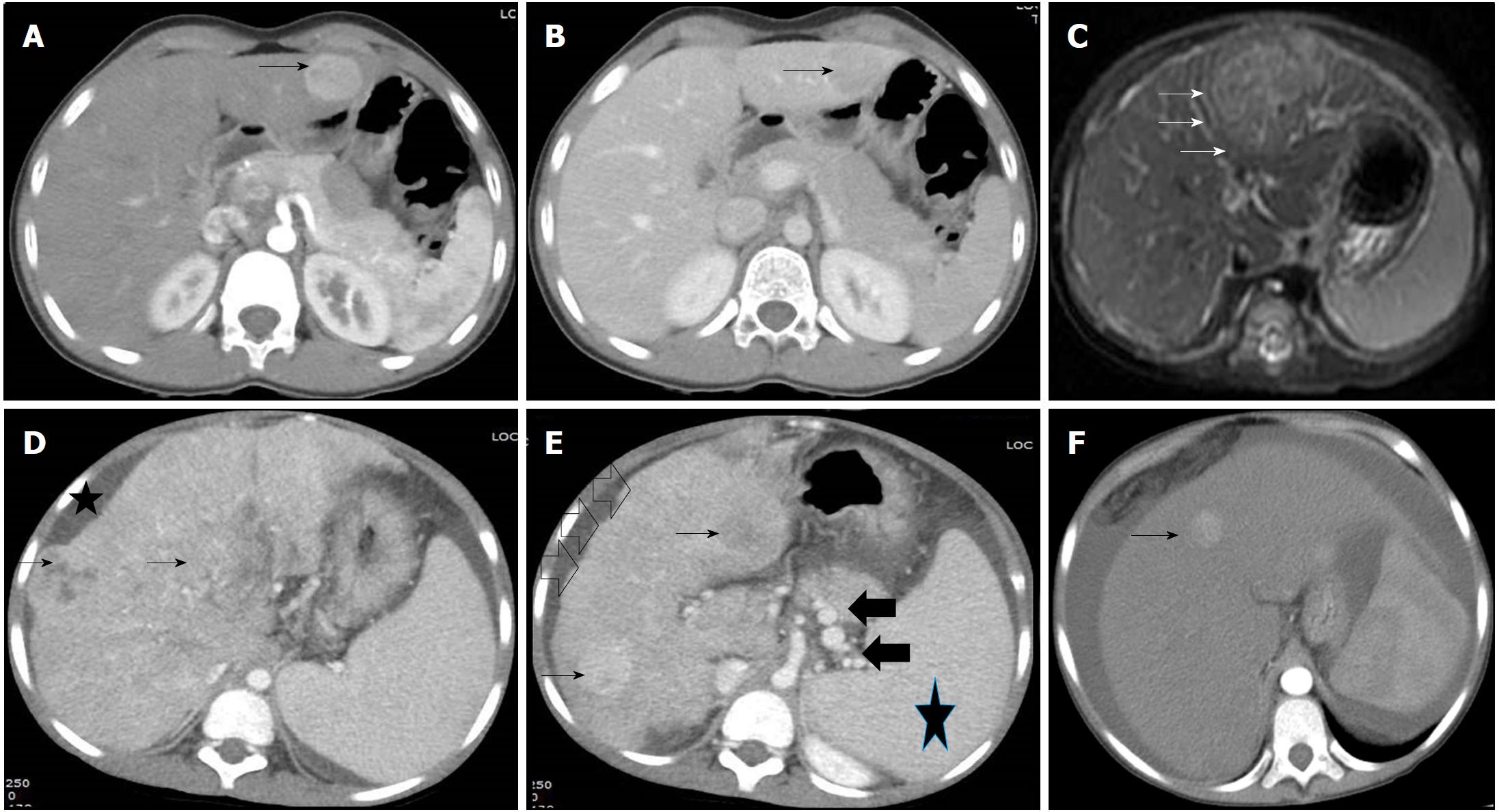
Figure 3 Radiological images in children with hepatocellular carcinoma.
A and B: 14 and half years old boy with chronic hepatitis-B (Immunoclearance phase), HBeAg+, DNA 5 log, AFP = 3 ng/mL (normal), with a segment 3 lesion (2.5 cm × 2.4 cm), BCLC stage A. Contrast-enhanced CT (CECT) image showing enhancement of the lesion (arrow) in the arterial phase (A) and washout in delayed venous phase (B) in a background of non-cirrhotic liver; C: 10 mo old boy with infantile cholestasis, bile salt export pump (BSEP) deficiency on immunostaining, incidentally found to have lesion in segment II and IVa abutting the capsule, BCLC stage B. The lesion was T2 hyperintense with enhancement in the arterial phase (arrows) and washout in the delayed phase; D and E: 8-1/2 yr old boy with decompensated chronic liver disease, chronic hepatitis-B (Immunoclearance phase), HBeAg+, DNA 7 log, AFP = 250000 ng/mL, with multifocal HCC, BCLC stage D, Child-Pugh C. Contrast-enhanced CT (CECT) image showing heterogenous lesion (arrows, D and E) involving whole of the right lobe with enhancement in the arterial phase in few lesions (arrows, E) in a background of cirrhotic liver with nodular margins (open black arrows, E), ascites (star, D) and collaterals (black solid arrows, E) and splenomegaly (star, E); F: 14 yr old girl with hepatic venous outflow tract obstruction, ascites, portal hypertension, incidentally found to have a lesion in segment 4 (1 cm × 1 cm), BCLC stage D, Child-Pugh C. Contrast-enhanced CT (CECT) image showing enhancement of lesion in the arterial phase (arrow).
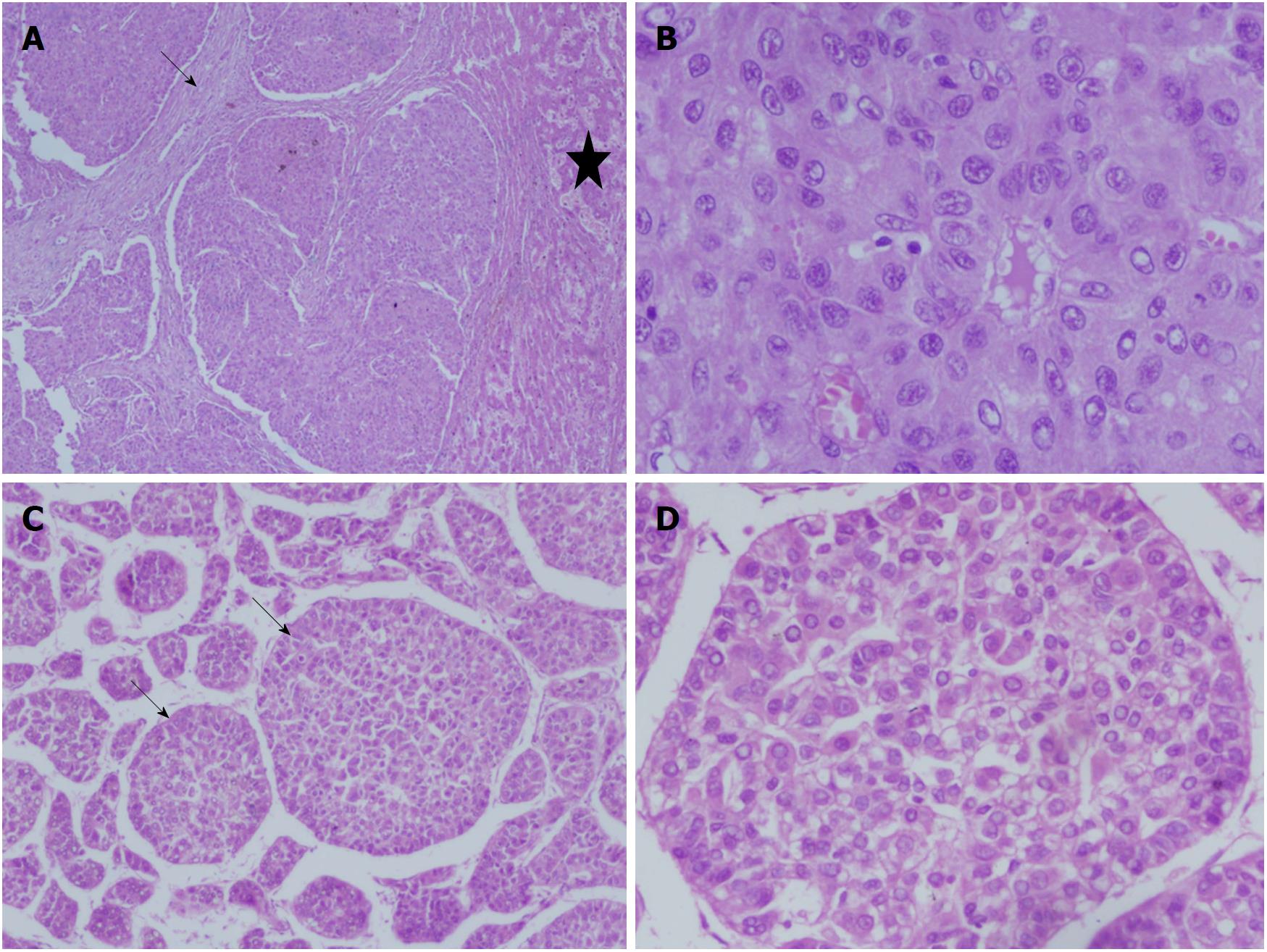
Figure 4 Liver histology images in children with hepatocellular carcinoma.
A and B: 15 yr old boy with HBeAg negative chronic hepatitis-B, DNA 4 log, precore mutant, AFP = 150000 ng/mL, with a large HCC in right lobe, with portal vein thrombosis, BCLC stage C, Child Pugh A, underwent right hepatectomy. Low power view showing tumor nodules separated by fibrous bands (arrow), adjacent non-malignant parenchyma (star) (100 ×, HE stain) (A). High power view showing malignant nuclear details with prominent nucleoli and eoisnophilic cytoplasm (400 ×, HE stain) (B); C and D: 14 and half years old boy with chronic hepatitis-B (Immunoclearance phase), HBeAg+, DNA 5 log, AFP = 3 ng/mL (normal), with a segment 3 lesion (2.5 cm × 2.4 cm), BCLC stage A, underwent non-anatomic resection. Low power view of tumor showing broadened trabeculae (arrows) (100 ×, HE stain) (C). Trabeculae with malignant cytological features - nuclear atypia and anisocytosis (200 ×, HE stain) (D).
- Citation: Khanna R, Verma SK. Pediatric hepatocellular carcinoma. World J Gastroenterol 2018; 24(35): 3980-3999
- URL: https://www.wjgnet.com/1007-9327/full/v24/i35/3980.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i35.3980