Copyright
©The Author(s) 2017.
World J Gastroenterol. Nov 14, 2017; 23(42): 7609-7617
Published online Nov 14, 2017. doi: 10.3748/wjg.v23.i42.7609
Published online Nov 14, 2017. doi: 10.3748/wjg.v23.i42.7609
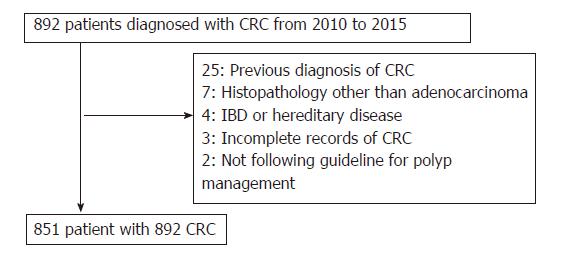
Figure 1 Patient flow chart.
CRC: Colorectal cancer.
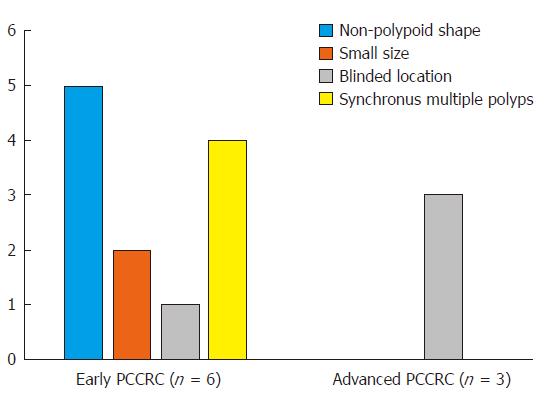
Figure 2 Possible explanations for the 9 “missed or new” post-colonoscopy colorectal cancers.
The bar chart shows the number of each possible explanation for the 6 early “missed or new” PCCRCs (left) and the 3 advanced “missed or new” PCCRCs (right). Among the 6 early “missed or new”PCCRCs, possible explanations were a non-polypoid shape in 5 cases (83%), presence of synchronous multiple (n ≥ 3) polyps at initial colonoscopy in 4 (67%), a small size (< 10 mm) in 2 (33%), and a blind location in 1 (17%). For all 3 (100%) of the advanced “missed or new” PCCRCs, a blind location was considered to have been likely. PCCRC: Post-colonoscopy colorectal cancer.
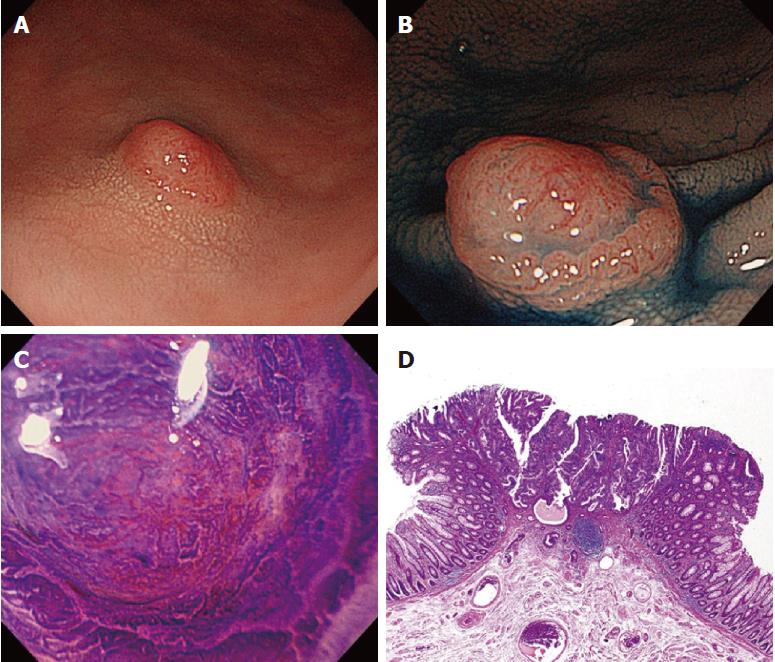
Figure 3 An early “missed or new” post-colonoscopy colorectal cancer case (No.
7 in Table 2). A 79-year-old man underwent initial colonoscopy, and seven small adenomatous polyps in the ascending and sigmoid colon were resected. A: A diminutive lesion 4 mm in size was found in the sigmoid colon during surveillance colonoscopy 15 mo after initial colonoscopy; B: Chromoendoscopy with indigo-carmine dye visualizes the margin of the deep depressed area on the surface of the lesion, and crystal violet stain shows a type-Vi pit with an invasive pattern suggesting submucosal deep invasive cancer (C); D: Histopathological examination of the surgical specimen reveals well to moderately differentiated adenocarcinoma with submucosal deep (3000 μm) invasion and no lymph node metastasis.
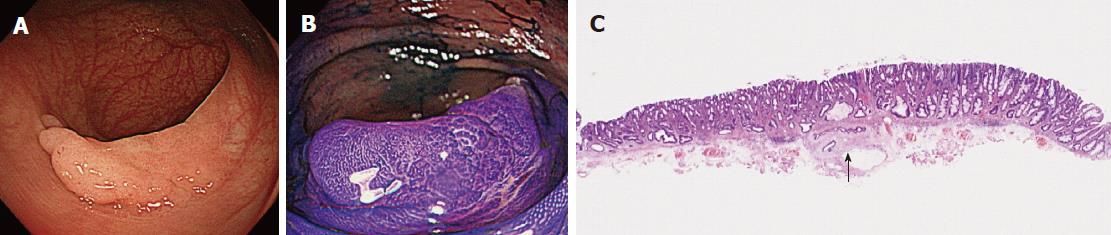
Figure 4 An early “missed or new” post-colonoscopy colorectal cancer case (No.
3 in Table 2). An 82-year-old man underwent initial colonoscopy and was found to have no adenomatous polyps. A: Subsequent colonoscopy 17 mo later revealed a large flat lesion, a laterally spreading non-granular-type tumor (LST-NG), measuring 25 mm in the transverse colon; B: Chromoendoscopy with crystal violet shows a type-Vi pit with a non-invasive pattern suggesting high-grade adenoma or submucosal shallow invasive cancer; C: Histopathological examination of the ESD specimen reveals well differentiated adenocarcinoma with submucosal shallow (200 μm) invasion (arrow) and no lymphovascular involvement. ESD: Endoscopic submucosal dissection.
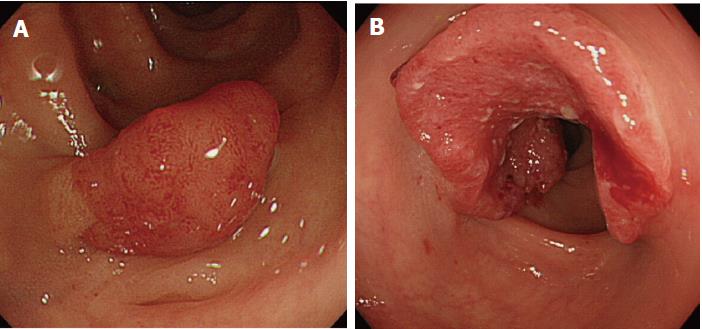
Figure 5 An advanced “missed or new” post-colonoscopy colorectal cancer case (No.
10 in Table 2). A: A 77-year-old woman underwent initial colonoscopy and a pedunculated adenomatous polyp 9 mm in size was resected; B: A large advanced cancer 50 mm in size was found in the recto-sigmoid colon at subsequent colonoscopy for hematochezia 12 mo later. Histopathological examination of the surgical specimen showed well to moderately differentiated adenocarcinoma invading the subserosa, and no lymph node metastasis.
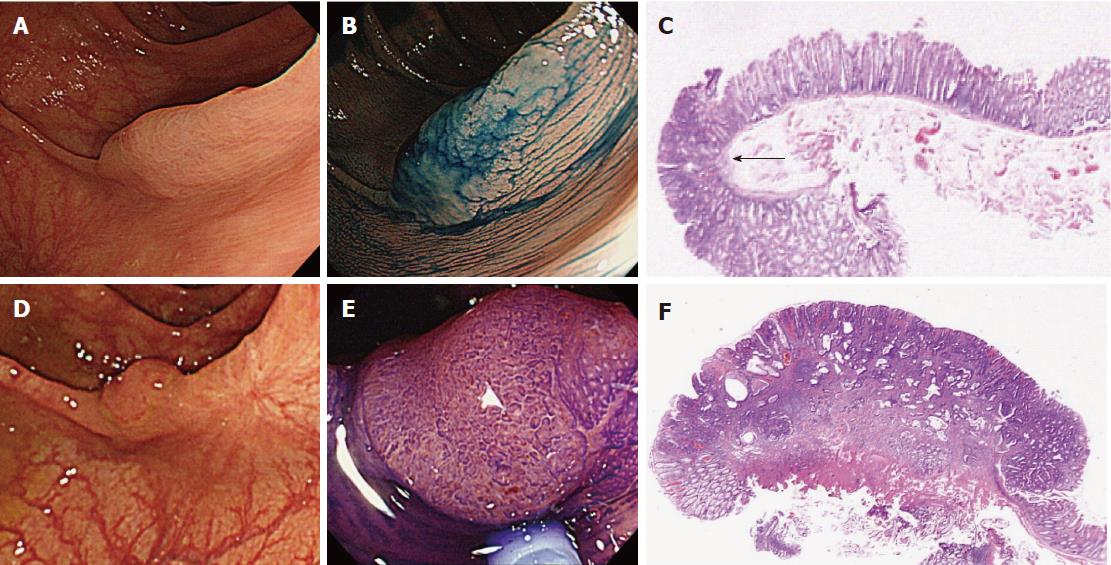
Figure 6 An early post-colonoscopy colorectal cancer case resulting from incomplete resection (No.
6 in Table 2). A 73-year-old woman underwent initial colonoscopy. A large flat lesion 20 mm in size showing type-II and open type-II pits, suggestive of SSA/P, was found by chromoendoscopy in the transverse colon and resected by piecemeal EMR with no macroscopically evident residual lesion (A and B); C: Histopathology of the resected specimen divided into 3 pieces revealed high-grade dysplasia (arrow) in SSA/P with intact vertical and horizontal margins of the dysplasia; D: Surveillance colonoscopy 11 months after initial colonoscopy detected a flat 10-mm lesion on the scar of the initial EMR in the transverse colon; E: Chromoendoscopy with crystal violet revealed unusual type-Vi pits suggesting submucosal invasive cancer; F: Histopathological examination of the EMR specimen revealed moderately differentiated adenocarcinoma invading the deep (2500 μm) submucosa with lymphovascular involvement. Finally, surgery was performed and histopathological examination revealed no residual cancer at the EMR site in the transverse colon and no lymph node metastasis. EMR: Endoscopic mucosal resection; SSA/P: Sessile serrated adenoma/polyp.
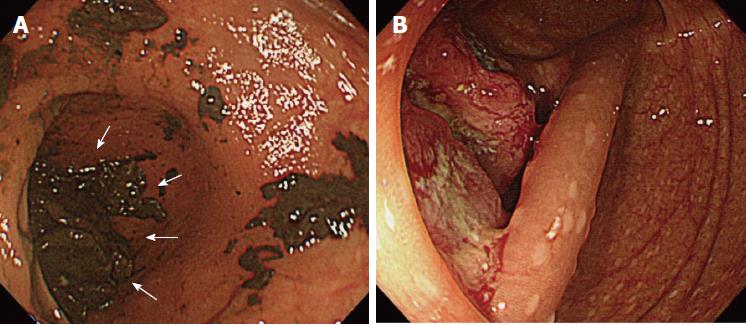
Figure 7 An advanced post-colonoscopy colorectal cancer case resulting from inadequate examination (No.
8 in Table 2). A 70-year-old woman underwent emergency colonoscopy with poor bowel preparation. A: No polyp was found in the colon but a quantity of residual stools covered the lower end of the cecum (arrow); B: Subsequent colonoscopy for hematochezia 9 mo after initial colonoscopy detected a large advanced cancer 30 mm in size at the cecum bottom. Histopathological examination of the surgically resected specimen revealed well differentiated adenocarcinoma invading the subserosa and no lymph node metastasis.
- Citation: Iwatate M, Kitagawa T, Katayama Y, Tokutomi N, Ban S, Hattori S, Hasuike N, Sano W, Sano Y, Tamano M. Post-colonoscopy colorectal cancer rate in the era of high-definition colonoscopy. World J Gastroenterol 2017; 23(42): 7609-7617
- URL: https://www.wjgnet.com/1007-9327/full/v23/i42/7609.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i42.7609