Copyright
©The Author(s) 2017.
World J Gastroenterol. May 21, 2017; 23(19): 3396-3406
Published online May 21, 2017. doi: 10.3748/wjg.v23.i19.3396
Published online May 21, 2017. doi: 10.3748/wjg.v23.i19.3396
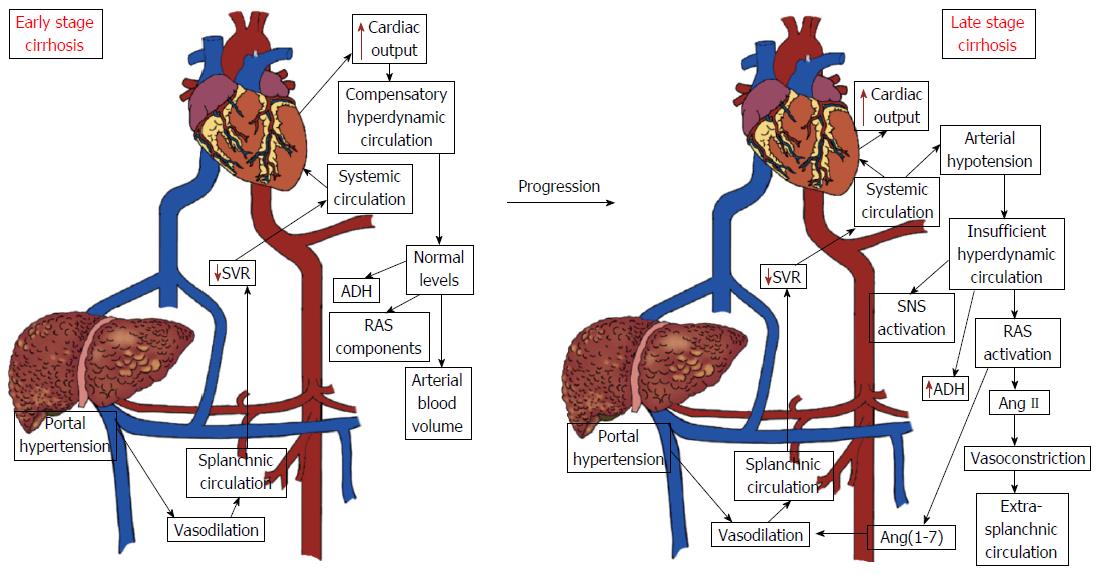
Figure 1 Hemodynamic changes in early and advanced stages of liver cirrhosis.
The early phase of cirrhosis is characterized by elevated cardiac output and low systemic vascular resistance without changes in the circulating levels of renin angiotensin system (RAS) components and antidiuretic hormone (ADH). However, as the disease progresses, activation of the circulating RAS and of the sympathetic nervous system and secretion of the antidiuretic hormone occur in response to persistent arterial hypotension. Legend: Ang II: Angiotensin II; Ang-(1-7): Angiotensin (1-7); SNS: Sympathetic nervous system; SVR: Systemic vascular resistance.
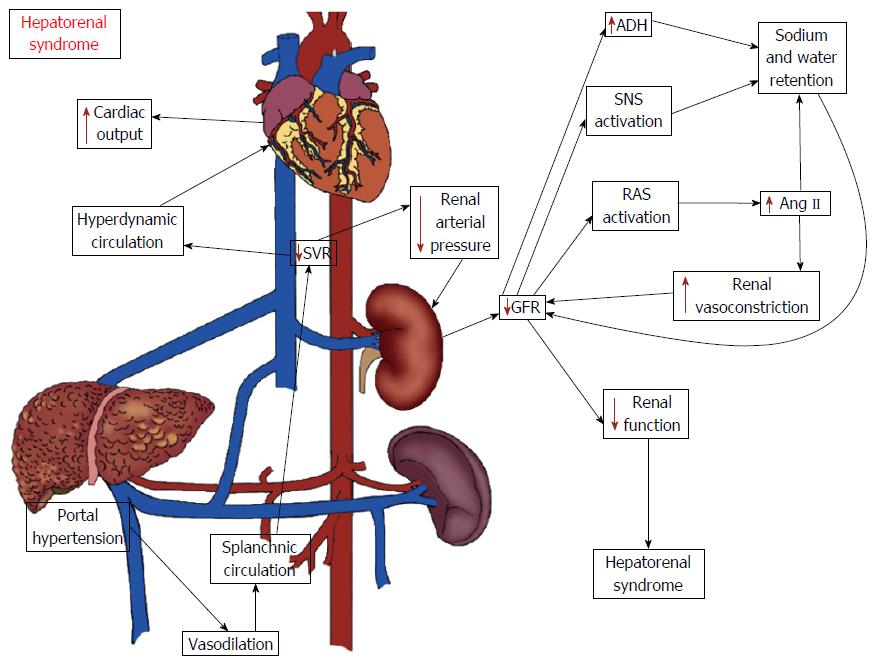
Figure 2 Potential mechanisms of hepatorenal syndrome.
The hemodynamic changes associated with advanced stages of cirrhosis may lead to reductions in renal blood flow and in the glomerular filtration rate (GFR) as a compensatory mechanism to the low systemic vascular resistance and arterial hypotension. The kidney hypoperfusion is the hallmark of hepatorenal syndrome (HRS) and occurs as a consequence of the activation of systemic vasoconstrictor factors, including the classical axis of the renin angiotensin system (RAS), sympathetic nervous system and antidiuretic hormone (ADH). The increase in kidney vasoconstriction negatively influences its function, ultimately leading to HRS. Legend: Ang II: Angiotensin II; SNS: Sympathetic nervous system; SVR: Systemic vascular resistance.
- Citation: Simões e Silva AC, Miranda AS, Rocha NP, Teixeira AL. Renin angiotensin system in liver diseases: Friend or foe? World J Gastroenterol 2017; 23(19): 3396-3406
- URL: https://www.wjgnet.com/1007-9327/full/v23/i19/3396.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i19.3396