Copyright
©The Author(s) 2017.
World J Gastroenterol. Apr 7, 2017; 23(13): 2414-2423
Published online Apr 7, 2017. doi: 10.3748/wjg.v23.i13.2414
Published online Apr 7, 2017. doi: 10.3748/wjg.v23.i13.2414
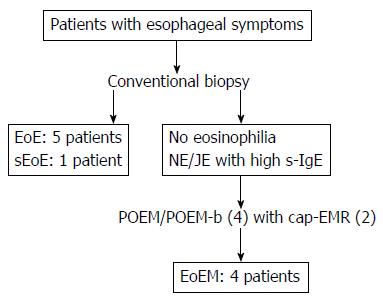
Figure 1 The schema of the present study.
Eosinophilic esophagitis (EoE) was diagnosed by conventional endoscopy in 5 patients, and a subtype of eosinophilic esophagitis (subepithelial eosinophilic esophagitis: sEoE) in 1 patient. Patients with no eosinophilia by conventional biopsy and with a nutcracker esophagus (NE) or jackhammer esophagus (JE) identified on high-resolution manometry received peroral endoscopic myotomy (POEM). These patients also showed elevated serum immunoglobulin E (s-IgE) levels. Four patients were diagnosed with eosinophilic esophageal myositis (EoEM) by peroral esophageal muscle biopsy (POEM-b), with cap-fitted endoscopic mucosal resection used in two of these four patients to facilitate POEM/POEM-b entry.
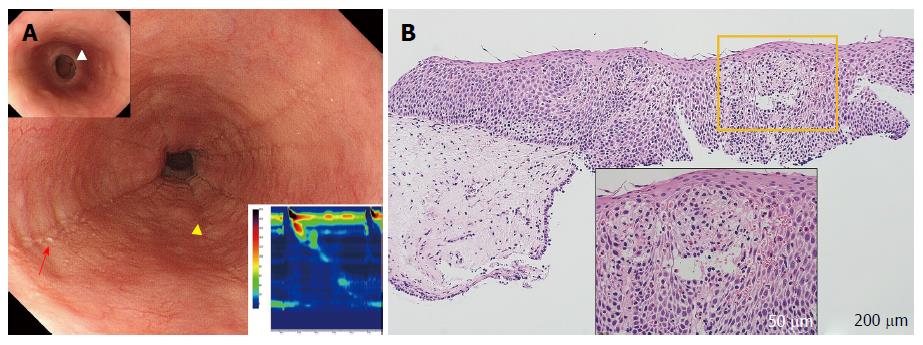
Figure 2 Eosinophilic esophagitis (case 3).
A: Endoscopy shows longitudinal furrows (yellow triangles) and white plaques (red arrow) in the medial esophagus, and the presence of fixed rings in the lower esophagus [upper insert (white triangle)]. High-resolution manometry (HRM) results showing highly disrupted distal contractile integral (DCI; 54.8 mmHg/[s•cm], lower insert). The patient was diagnosed with failed peristalsis based on the Chicago classification criteria; B: Histology at 100 × magnification, showing significant eosinophil inflammation was observed (50 eosinophils per high-power field) in the esophageal epithelium with dilated intercellular spaces (lower insert).
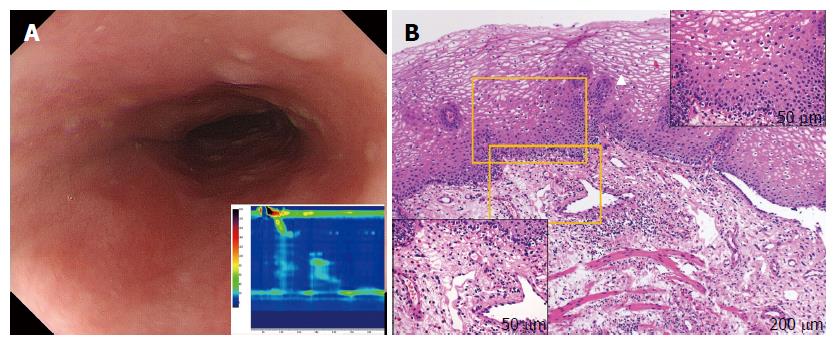
Figure 3 Subepithelial eosinophilic esophagitis (case 6).
A: Endoscopy showing the compressed lumen. Characteristic findings for eosinophilic esophagitis such as longitudinal furrows, white plaques, or fixed rings are not seen. High-resolution manometry (HRM) results, showing highly disrupted distal contractile integral (42.5 mmHg/[s•cm], lower insert). The patient was diagnosed with failed peristalsis based on the Chicago classification criteria; B: Mucosal histology by conventional biopsy at 100 × magnification. The white triangle indicates upward papillae elongation. In the upper-right inset, there is an absence of eosinophil infiltration in the epithelium (400 × magnification). Subepithelial eosinophilia (35 eosinophils per high-power field) is shown in the left lower inset (400 × magnification).
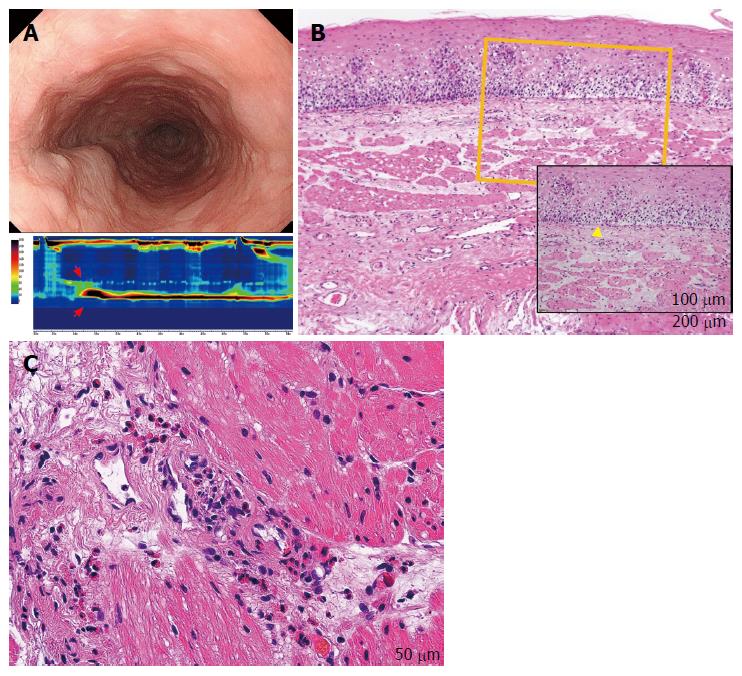
Figure 4 Eosinophilic esophageal myositis (case 10).
A: Endoscopy showing a compressed lumen similar to that in a case of subepithelial eosinophilic esophagitis (sEoE) and different to that in a case of eosinophilic esophagitis (EoE). Results of the high-resolution manometry are shown in the lower insert. An extremely high maximum distal contractile integral (DCI) is observable (13462.2 mmHg/[s•cm], red arrows). The patient was diagnosed with a jackhammer esophagus based on the Chicago classification criteria; B: The entry site for peroral esophageal muscle biopsy (POEM-b) was created by cap-fitted endoscopic mucosal resection in order to obtain mucosal and submucosal specimens. Epithelial eosinophilia was not seen, with only basal layer destruction (yellow triangle) apparent. In the subepithelial layer, the number of eosinophils was elevated, although the eosinophil number was less than that in the muscle layer; C: Muscle-layer histopathology by POEM-b, showing a severe eosinophilic infiltration in the perivascular and perimysial area of the muscle specimens (48 eosinophils per high-power field) at 400 × magnification.
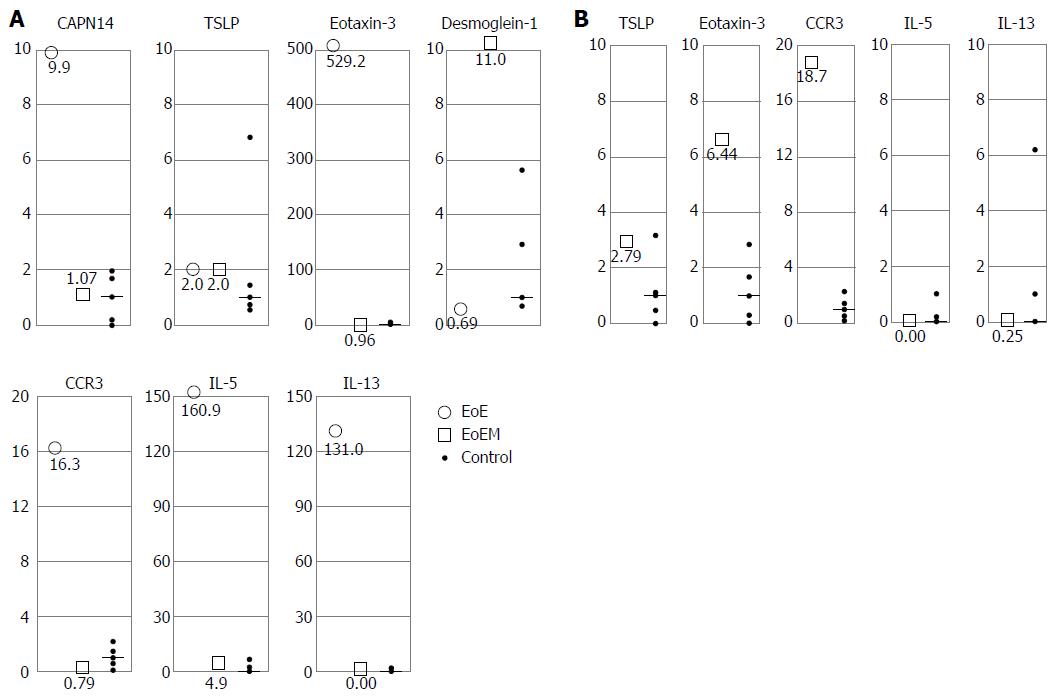
Figure 5 Real-time quantitative reverse transcription polymerase chain reaction analysis for esophageal mucosal and muscle layer samples (a vertical axis scale indicates the relative ratio compared with median control value converted to 1).
A: mRNA analysis for esophageal mucosal specimens in eosinophilic esophagitis (○), and eosinophilic esophageal myositis (□). In cases 1, 3, 4, and 5 with eosinophilic esophagitis (EoE), the expression of CAPN14, eotaxin-3, CCR3, IL-5, and IL-13 was increased, while the expression of DSG1 was decreased. In cases of eosinophilic esophageal myositis (case 9, and 10), no change was observed in CAPN14, TSLP, eotaxin-3, CCR3, IL-5, and IL-13 expression levels. The expression level of DSG1 was highly preserved in EoEM; B: mRNA analysis for esophageal muscle specimens in eosinophilic esophageal myositis (□). In eosinophilic esophageal myositis (case 9 and 10), muscle-layer samples by peroral esophageal muscle biopsy were also sent for mRNA expression analysis. The levels of eotaxin-3 and CCR3 were increased, although TSLP, IL-5, and IL-13 were within control value ranges.
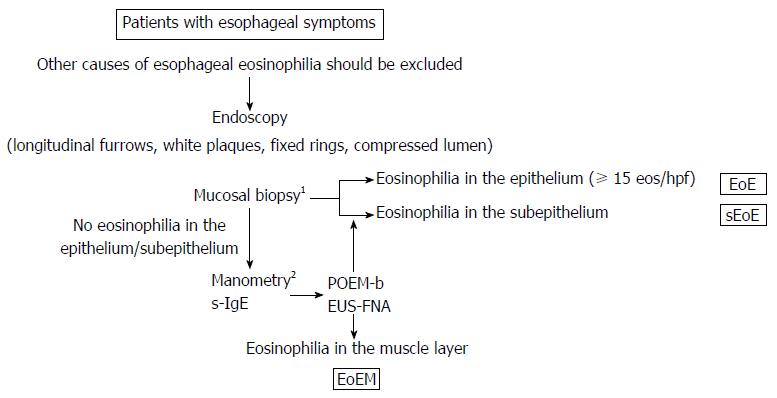
Figure 6 Proposed diagnostic criteria for eosinophilic gastrointestinal disorders in the esophagus.
Patients with esophageal symptoms receive endoscopy. 1Mucosal biopsy should include a sufficient amount of subepithelium together with epithelium to allow subepithelial eosinophilia to be identified. If no or low degree of eosinophilia is seen in the epithelium/subepithelium but manometry shows abnormal peristalsis and elevated serum immunoglobulin E (s-IgE) level, peroral esophageal muscle biopsy (POEM-b) or endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) is recommended to detect eosinophilia in deeper layers. 2Manometry findings and s-IgE levels are variable, careful follow-up is recommended even if the findings are normal initially; Other alternative causes of esophageal symptoms should be ruled out.
- Citation: Sato H, Nakajima N, Takahashi K, Hasegawa G, Mizuno KI, Hashimoto S, Ikarashi S, Hayashi K, Honda Y, Yokoyama J, Sato Y, Terai S. Proposed criteria to differentiate heterogeneous eosinophilic gastrointestinal disorders of the esophagus, including eosinophilic esophageal myositis. World J Gastroenterol 2017; 23(13): 2414-2423
- URL: https://www.wjgnet.com/1007-9327/full/v23/i13/2414.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i13.2414