Copyright
©The Author(s) 2016.
World J Gastroenterol. Nov 14, 2016; 22(42): 9257-9278
Published online Nov 14, 2016. doi: 10.3748/wjg.v22.i42.9257
Published online Nov 14, 2016. doi: 10.3748/wjg.v22.i42.9257
Figure 1 Albert J Czaja, MD, Professor Emeritus of Medicine, Mayo Clinic College of Medicine, Rochester, Minnesota, United States.
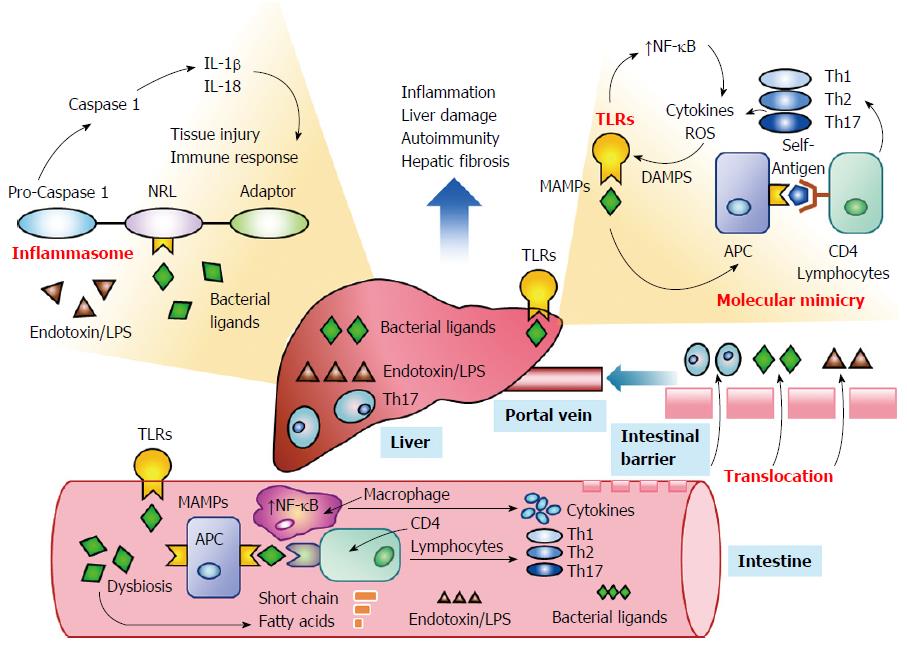
Figure 2 Interactions between the intestinal microbiome and the liver.
Dysbiosis can generate microbe-associated molecular patterns (MAMPs) that activate toll-like receptors (TRLs) in the intestine. Activated TLRs can stimulate the transcription factor, nuclear factor-kappa B (NF-κB), in macrophages and generate pro-inflammatory cytokines. They can also increase the expression of the major histocompatibility complex on antigen presenting cells (APCs) and sensitize CD4 lymphocytes to bacterial ligands. The activated lymphocytes can proliferate as T helper (Th) 1, Th2, and Th17 cells. The dysbiosis can also generate short chain fatty acids, endotoxin, lipopolysaccharide (LPS), and bacterial components that can serve as antigenic ligands. Tight junctions within the intestinal mucosa may weaken with the dysbiosis and allow paracellular translocation of lymphocytes, bacterial ligands and endotoxin. These gut-derived elements can then enter the portal vein and be delivered to the liver. The bacterial ligands within the liver can activate TLRs within hepatocytes, hepatic stellate cells, Kupffer cells, and sinusoidal epithelial cells and generate pro-inflammatory cytokines and reactive oxygen species (ROS) that can produce damage-associated molecular patterns (DAMPs) that activate TLRs in a self-amplification loop (upper right corner blow-up). The hepatic TLRs can also contribute to the sensitization of CD4 lymphocytes to bacterial ligands and self-antigens that resemble bacterial ligands (molecular mimicry). Concurrently, the bacterial ligands and gut-derived endotoxin can activate the non-obese diabetes-like receptor (NLR) of inflammasomes within hepatocytes and hepatic stellate cells (upper left corner blow-up). The release of caspase 1 can generate interleukin (IL) 1β and IL-18 and promote tissue injury and the immune response. The net effect is to increase hepatic inflammation and liver damage and predispose to autoimmunity and hepatic fibrosis.
- Citation: Czaja AJ. Factoring the intestinal microbiome into the pathogenesis of autoimmune hepatitis. World J Gastroenterol 2016; 22(42): 9257-9278
- URL: https://www.wjgnet.com/1007-9327/full/v22/i42/9257.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i42.9257