Copyright
©The Author(s) 2016.
World J Gastroenterol. Sep 21, 2016; 22(35): 7973-7982
Published online Sep 21, 2016. doi: 10.3748/wjg.v22.i35.7973
Published online Sep 21, 2016. doi: 10.3748/wjg.v22.i35.7973
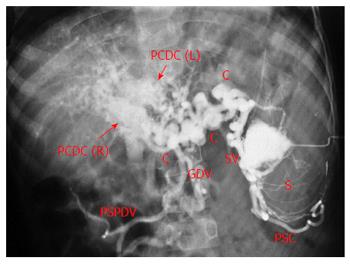
Figure 1 Splenoportovenography in a patient with extrahepatic portal venous obstruction and portal cavernoma.
Contrast within splenic pulp (S) is drained by multiple splenic vein channels (SV) into large peripancreatic collaterals (C). There are two broad parallel conglomerate of veins in the porta hepatis (arrows) formed by right and left paracholedochal collaterals [PCDC (R) and PCDC (L) respectively], forming the portal cavernoma. Main portal vein is not seen (thrombosed). Retrograde filling of perisplenic collaterals (PSC), gastroduodenal vein (GDV) and posterior-superior pancreaticoduodenal vein (PSPDV) is seen.
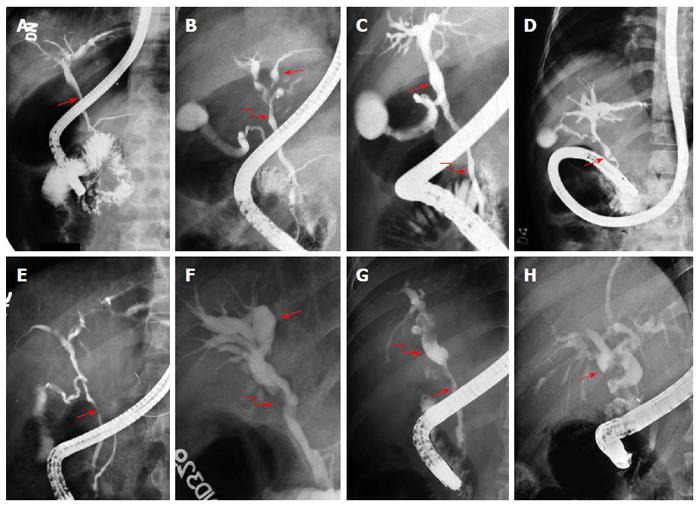
Figure 2 Endoscopic retrograde cholangiograms in 8 patients of portal biliopathy depicting spectrum of cholangiographic abnormalities of portal biliopathy.
A: Extrinsic impression on common bile duct (arrow); B: Ectasia of left hepatic duct (arrow) and caliber irregularity of common hepatic duct (curved arrow); C: Ectasia of common hepatic duct (arrow) and caliber irregularity of common bile duct (curved arrow); D: Angulation (arrow) of common bile duct; E: Large smooth impression (arrow) on common bile duct; F: Angulation common hepatic duct (curved arrow) and gross ectasia of intrahepatic ducts (arrow); G: Long smooth stricture of common bile duct (arrow) with upstream dilatation (curved arrow); H: dilated bile ducts with multiple filling defects (arrow). Adapted and modified from Khuroo et al[3].
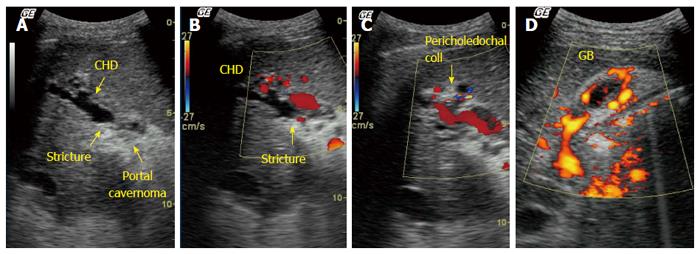
Figure 3 Ultrasound with Doppler in a patient with extrahepatic portal venous obstruction and portal biliopathy.
A: Gray scale image shows an echogenic mass in hilum (portal cavernoma). Common hepatic duct (CHD) shows dilatation and luminal irregularity with a stricture at the level of the cavernoma; B: Color Doppler image showed multiple pericholedochal collaterals around the strictured bile duct (arrow); C: Color Doppler image shows pericholedochal collaterals and recanalized irregular portal vein; D: Power Doppler images of gall bladder. Gall bladder wall is thickened with multiple collaterals within the gall bladder wall.
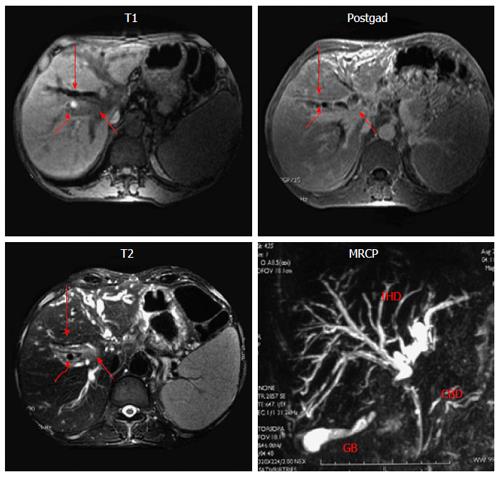
Figure 4 Magnetic resonance imaging with Magnetic retrograde cholangiogram in a patient with portal biliopathy.
T1 weighted, T2 weighted and post-gadolinium (postgad) images. Mass lesion (short arrow) is seen at the level of porta hepatis with dilated bile ducts (long arrow) and signal void (curved arrow), depicting collateral channels compressing bile ducts, MRCP. Common bile duct (CBD) shows luminal irregularity. There is a localized irregular stricture in common hepatic duct with upstream gross dilatation of intrahepatic ducts (IHD).
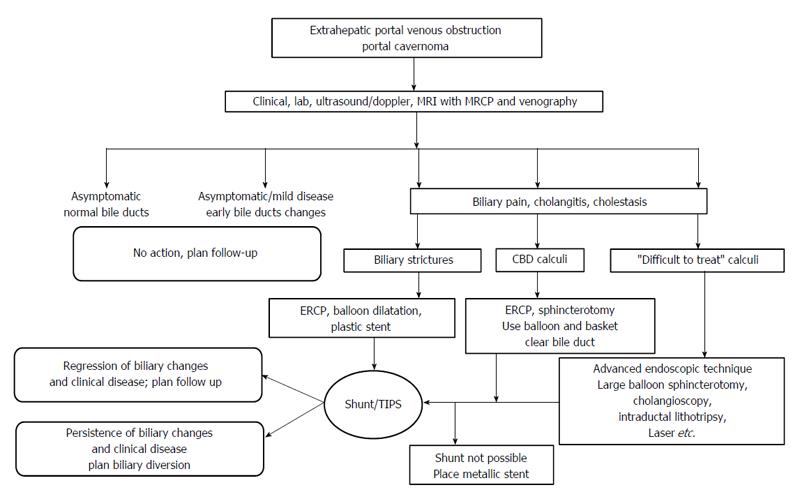
Figure 5 Management algorithm in patients of extrahepatic portal venous obstruction and portal biliopathy.
See text under “Management” for details. TIPS: Transjugular intrahepatic portosystemic shunt.
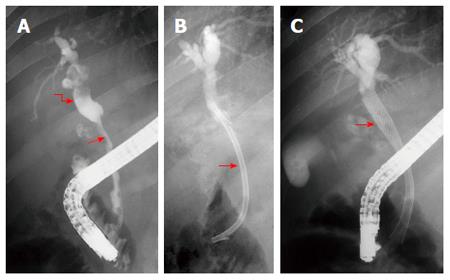
Figure 6 Endoscopic retrograde cholangiogram and metallic biliary stenting in a patient with portal biliopathy.
A: Long smooth stricture common bile duct (arrow) with upstream dilatation of intrahepatic ducts (curved arrow); B: A 12 Fr plastic stent (arrow) is placed across the stricture. Patient needed repeated stent replacement in the follow up and was considered for shunt surgery. Shunt surgery was not possible due unavailability of a shuntable portal vein; C: Self-expanding nitinol biliary stent (arrow) placed across the stricture. Patient stays asymptomatic over long-term follow up.
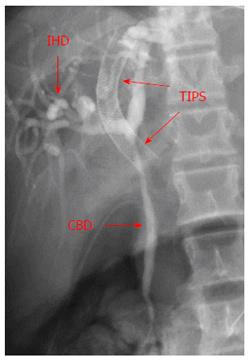
Figure 7 Transjugular intrahepatic porto-systemic shunt in a patient with extrahepatic portal venous obstruction and portal biliopathy.
Common bile duct shows a long smooth stricture (CBD) with upstream dilatation of intrahepatic ducts (IHD). Transjugular intrahepatic porto-systemic shunt (TIPS) (arrows) was placed to decompress the portal venous circulation. Follow-up showed significant improvement in cholangiographic appearances.
- Citation: Khuroo MS, Rather AA, Khuroo NS, Khuroo MS. Portal biliopathy. World J Gastroenterol 2016; 22(35): 7973-7982
- URL: https://www.wjgnet.com/1007-9327/full/v22/i35/7973.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i35.7973