Copyright
©The Author(s) 2016.
World J Gastroenterol. Aug 14, 2016; 22(30): 6817-6828
Published online Aug 14, 2016. doi: 10.3748/wjg.v22.i30.6817
Published online Aug 14, 2016. doi: 10.3748/wjg.v22.i30.6817
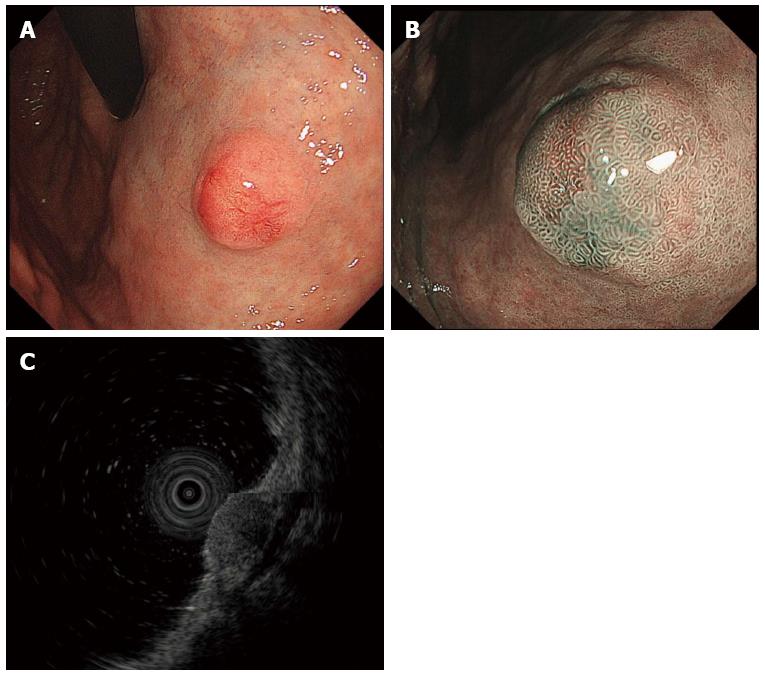
Figure 1 Gastric neuroendocrine tumor.
A: Conventional endoscopic image with white light demonstrates a hemispherical reddish submucosal tumor; B: Magnifying endoscopic image with narrow band imaging demonstrates gastric pit structures present on the surface of the tumor; C: Endoscopic ultrasound (EUS, 20 MHz) demonstrates a hypoechoic intramural structure in the second layer, which corresponds to the submucosal layer of the gastric wall. EUS: Endoscopic ultrasonography.
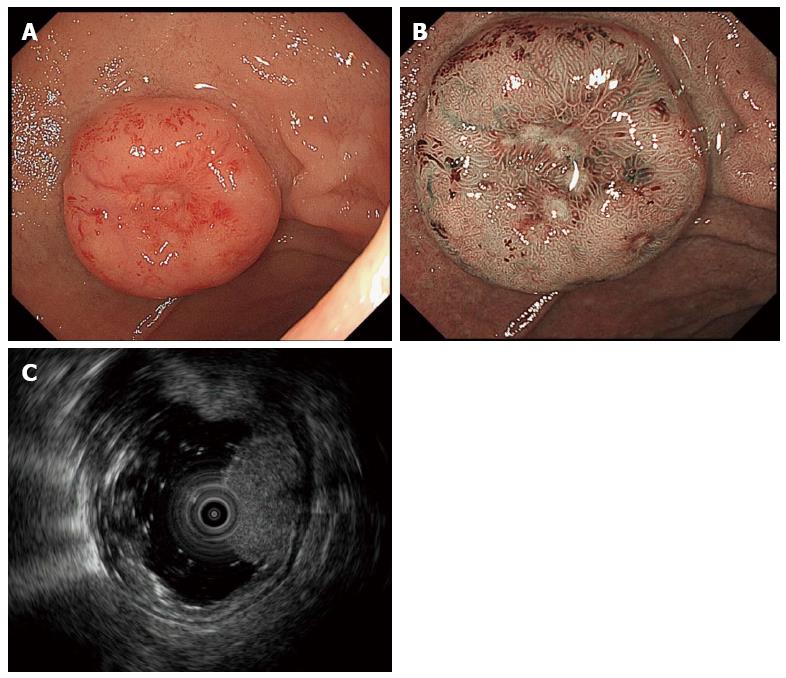
Figure 2 Duodenal neuroendocrine tumor.
A: Conventional endoscopic image with white light demonstrates a hemispherical reddish polyp with central depression; B: Magnifying endoscopic image with narrow band imaging demonstrates duodenal mucosal pit structures present on the entire surface of the tumor except the area over the central depression. Pit structures are absent over the central depression, and instead, cyan colored, cork-screw shaped, thick capillaries are seen; C: Endoscopic ultrasound (EUS, 20 MHz) demonstrates a slightly hyperechoic intramural structure in the second layer, extending to the third layer (corresponding to the duodenal muscularis propria). EUS: Endoscopic ultrasonography.
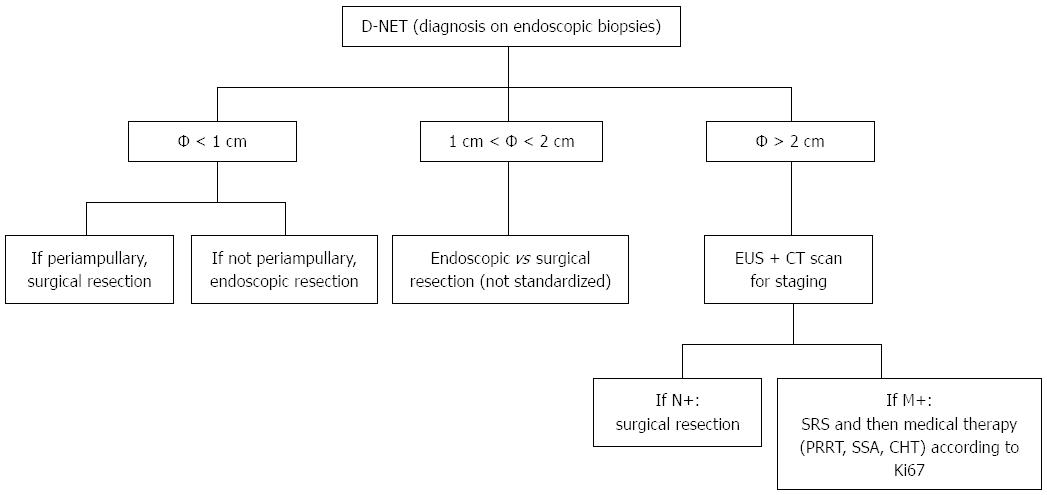
Figure 3 Management of duodenal neuroendocrine tumors.
D-NETs: Duodenal neuroendocrine tumors; EUS: Endoscopic ultrasound; CT: Computed tomography; N+: Lymph node metastasis; M+: Distant metastasis; SRS: Somatostatin receptor scintigraphy; PRRT: Peptide receptor radionuclide therapy; SSA: Somatostatin analogues; CHT: Chemotherapy.
- Citation: Sato Y, Hashimoto S, Mizuno KI, Takeuchi M, Terai S. Management of gastric and duodenal neuroendocrine tumors. World J Gastroenterol 2016; 22(30): 6817-6828
- URL: https://www.wjgnet.com/1007-9327/full/v22/i30/6817.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i30.6817