Copyright
©The Author(s) 2016.
World J Gastroenterol. Jan 14, 2016; 22(2): 618-627
Published online Jan 14, 2016. doi: 10.3748/wjg.v22.i2.618
Published online Jan 14, 2016. doi: 10.3748/wjg.v22.i2.618
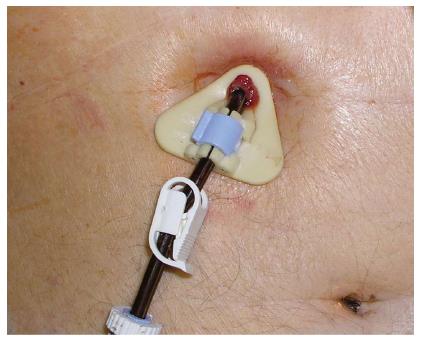
Figure 1 Buried bumper syndrome.
External view demonstrates tight position of the external fixator with peristomal granulations.
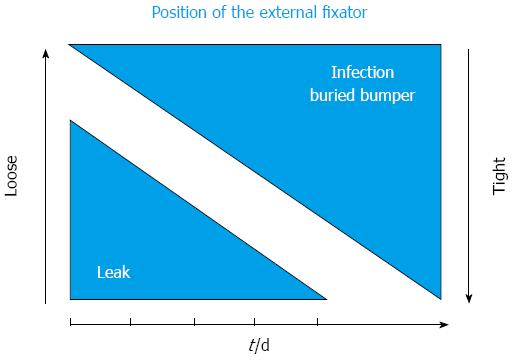
Figure 2 This chart demonstrates conflicting influence of the position of the external fixator (loose-tight) on the risk of complications (stomal infection, buried bumper syndrome and peritoneal leakage) as a function of time.
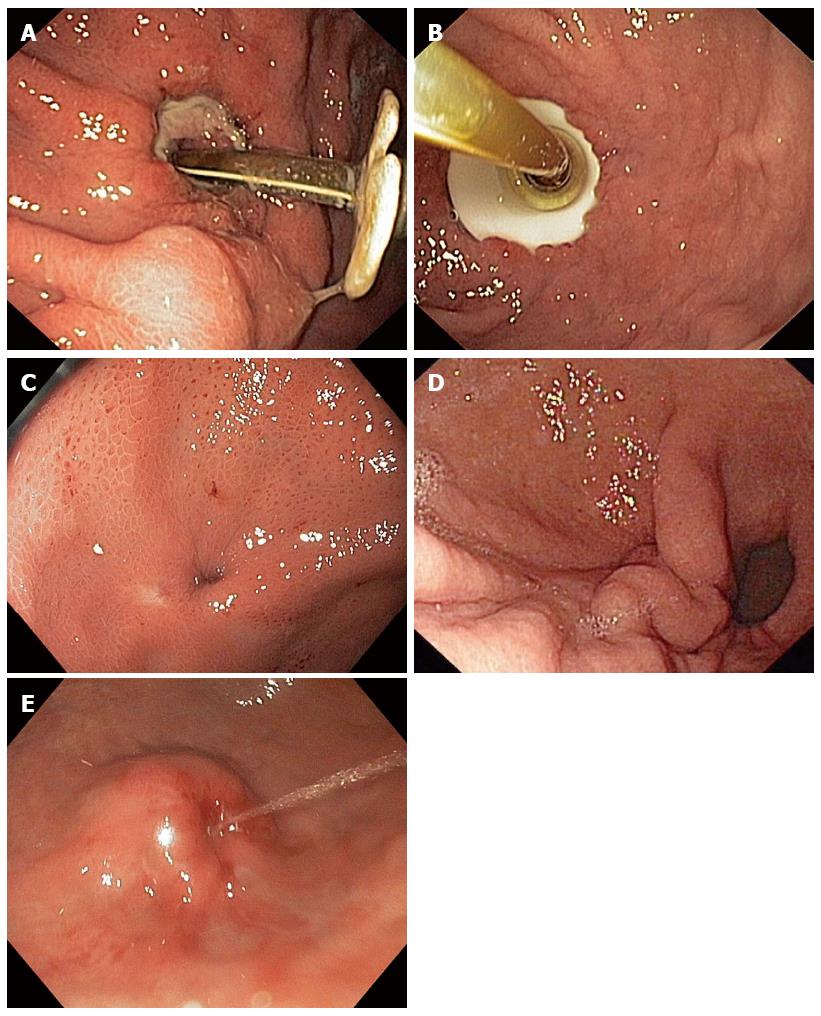
Figure 3 Buried bumper syndrome, gastroscopy.
A: Pressure ulcer under the internal bolster repositioned to the gastric lumen; B: Hyperplastic tissue growing over the edge of the disk; C: Flat stomach wall with fistula orifice covering totally the internal bolster; D: Completely buried disc retracting the gastric mucosa; E: Internal bolster totally embedded in the stomach wall resembling a submucosal tumor. Flushing solution running from the internal orifice of the residual fistula.
Figure 4 Buried bumper syndrome, fluoroscopy (tubogram).
Cavity around the buried bolster filled with contrast agent leaking through the fistula (arrow) to the stomach lumen.
Figure 5 Buried bumper syndrome, abdominal ultrasound.
Internal retention disc (arrowheads) located out of the lamina muscularis propria of the stomach (arrow).
Figure 6 Buried bumper syndrome, computed tomography.
Internal retention disc localized between the gastric and abdominal wall (courtesy of Pavel Ryska, MD, PhD, Department of radiology, University Hospital Hradec Kralove, Czech Republic).
Figure 7 Treatment methods of buried bumper syndrome.
A: Extraction of the buried gastrostomy tube with simultaneous pull through of the new one (adapted from[36,63]); B: “Push-pull T technique”. Endoscopist pulls the buried gastrostomy tube by a polypectomy snare anchored using a “T-arm”, while the system is stabilized and pushed inside using a clamp (adapted from[27,72]); C: A polypectomy snare entraps the buried cannula as close to the skin as possible (thanks to splitting) (adapted from[75]); D: Papillotome introduced through a shortened cannula cuts the overgrowing tissue (adapted from[78-81]).
- Citation: Cyrany J, Rejchrt S, Kopacova M, Bures J. Buried bumper syndrome: A complication of percutaneous endoscopic gastrostomy. World J Gastroenterol 2016; 22(2): 618-627
- URL: https://www.wjgnet.com/1007-9327/full/v22/i2/618.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i2.618