Copyright
©The Author(s) 2015.
World J Gastroenterol. Feb 21, 2015; 21(7): 2067-2072
Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2067
Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2067
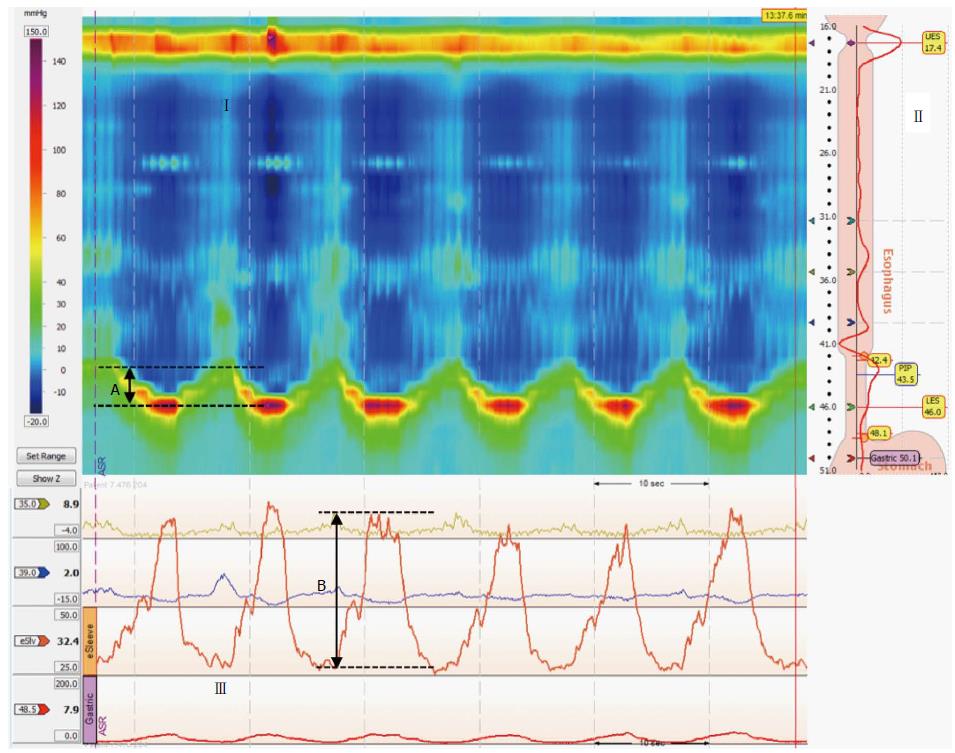
Figure 1 Sinus arrhythmia maneuver.
(Upper panels) Esophageal and esophagogastric junction (EGJ) pressure topography is shown during six 5-s inhalations (I). Inspiratory diaphragm lowering was then determined (A). The analysis landmarks are presented in the upper right panel (II). In this case, the e-sleeve extended approximately 6 cm across the EGJ. (Lower panel) (III) Esophageal and EGJ pressure tracings during sinus arrhythmia maneuver (SAM) where inspiratory peak pressures were measured (B) relative to expiratory pressure.
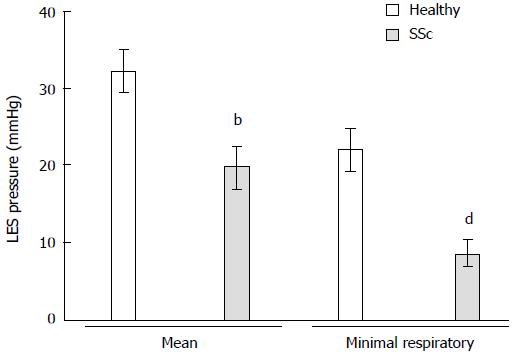
Figure 2 Mean lower esophageal sphincter pressure and minimal respiratory lower esophageal sphincter pressure in particular were significantly lower in systemic sclerosis patients than in healthy volunteers.
bP < 0.01, dP < 0.01 vs healthy. SSc: Systemic sclerosis; LES: Lower esophageal sphincter.
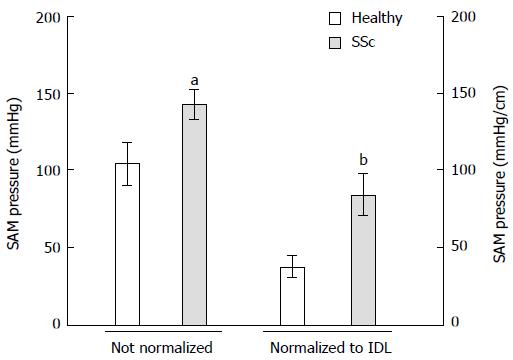
Figure 3 Esophagogastric junction pressure during sinus arrhythmia maneuver is higher in systemic sclerosis patients than in healthy volunteers.
This difference is even more pronounced if this parameter is normalized to the degree of inspiratory diaphragm lowering (IDL). aP < 0.05, bP < 0.01 vs Healthy. SSc: Systemic sclerosis; SAM: Sinus arrhythmia maneuver.
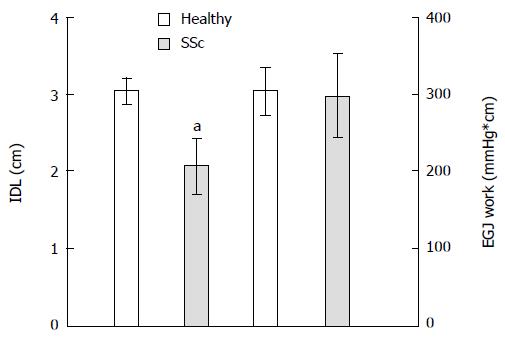
Figure 4 Degree of inspiratory diaphragm lowering is less in systemic sclerosis patients than in healthy volunteers.
Esophagogastric junction (EGJ) work is similar across these two groups. aP < 0.05 vs healthy. SSc: Systemic sclerosis; SAM: Sinus arrhythmia maneuver; IDL: Inspiratory diaphragm lowering.
- Citation: Nobre e Souza MÂ, Bezerra PC, Nobre RA, Holanda ESDF, Santos AAD. Increased inspiratory esophagogastric junction pressure in systemic sclerosis: An add-on to antireflux barrier. World J Gastroenterol 2015; 21(7): 2067-2072
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2067.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2067