Copyright
©The Author(s) 2015.
World J Gastroenterol. Oct 28, 2015; 21(40): 11304-11311
Published online Oct 28, 2015. doi: 10.3748/wjg.v21.i40.11304
Published online Oct 28, 2015. doi: 10.3748/wjg.v21.i40.11304
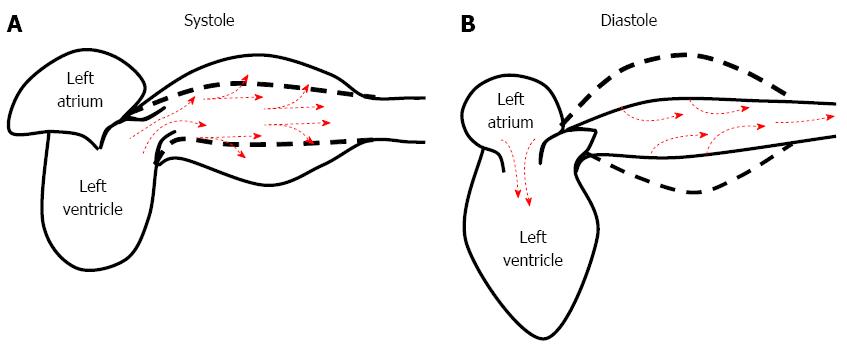
Figure 1 Role of arterial compliance in the damping of blood flow and the pressure oscillations generated by the heart.
A: During systole, a portion of the stroke volume is forwarded directly to the peripheral tissues; approximately 50% of the stroke volume is momentarily stored within the aorta and stretches the arterial walls; B: During diastole, the energy imbricated within the arterial wall is discharged, and the stored blood is forwarded into the peripheral tissues, ensuring continuous flow and contributing to the maintenance of sufficient diastolic blood pressure.
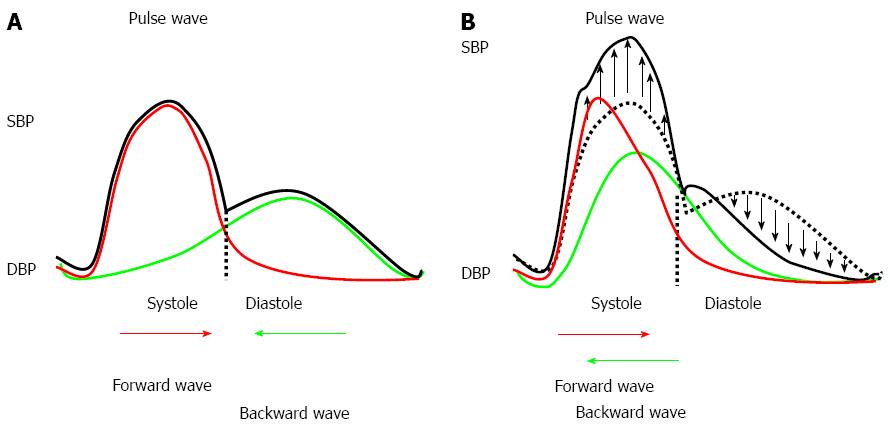
Figure 2 Arterial stiffness and reflection waves.
A: Pulse wave in subjects with normal arterial stiffness; B: Pulse waves in subjects with increased arterial stiffness. DBP: Diastolic blood pressure; SBP: Systolic blood pressure.
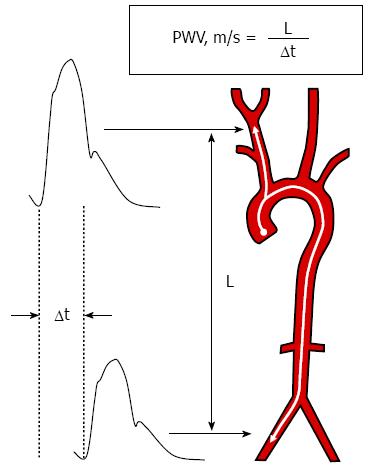
Figure 3 Reference technique utilized to measure carotid-femoral pulse wave velocity.
PWV: Pulse wave velocity; L: The distance between the two measurement sites; Δt: The time lag between the pulse waves acquired at the proximal (carotid) and distal (femoral) sites.
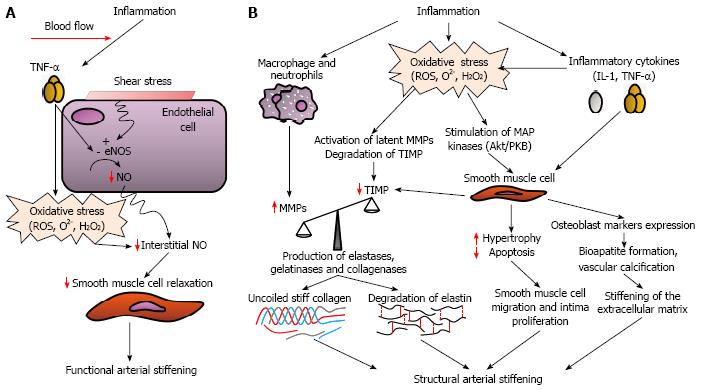
Figure 4 Potential mechanisms by which inflammation can induce functional (A) and structural (B) arterial stiffening.
eNOS: Endothelial nitric oxide synthase; H2O2: Hydrogen peroxide; IL-1: Interleukin-1; MMPs: Matrix metalloproteinases; NO: Nitric oxide; O2-: Superoxide; ROS: Reactive oxygen species; TIMP: Tissue inhibitor of matrix metalloproteinases; TNF-α: Tumor necrosis factor alpha.
- Citation: Zanoli L, Rastelli S, Inserra G, Castellino P. Arterial structure and function in inflammatory bowel disease. World J Gastroenterol 2015; 21(40): 11304-11311
- URL: https://www.wjgnet.com/1007-9327/full/v21/i40/11304.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i40.11304